Abstract
Objectives
To determine the correlation between CT-diagnosed extra-pancreatic extension of pancreatic ductal adenocarcinoma (PDAC), pathology-diagnosed extra-pancreatic extension, and survival in patients with PDAC.
Methods
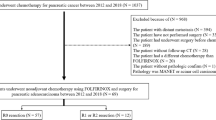
This retrospective study included 87 patients with resected PDAC. Two radiologists evaluated negative ((i) tumours surrounded by the pancreatic parenchyma and (ii) tumours contacting the pancreatic surface) or positive ((iii) tumours with peri-pancreatic strand appearances and/or with expansive growth) CT-diagnosed extra-pancreatic extension. Clinical, pathological, and CT imaging characteristics predicting disease-free survival (DFS) and overall survival (OS) were assessed using Cox proportional-hazards models. Diagnostic accuracy for pathology-diagnosed extra-pancreatic extension was also assessed.
Results
CT-diagnosed extra-pancreatic extension (42/87 tumours, 48.3%; κ = 0.82) had a higher hazard ratio (HR) for the DFS (HR, 5.30; p < 0.01) and OS (HR, 5.31; p < 0.01) rates than pathology-diagnosed extension in univariable analyses. It was also an independent prognostic factor for the DFS (HR, 4.22; p < 0.01) and OS (HR, 4.38; p < 0.01) rates in multivariable analyses. Of 45 tumours without CT-diagnosed extra-pancreatic extension, pathology-diagnosed extra-pancreatic extension was observed in 2/8 (25.0%) and 32/37 (86.5%) tumours with CT categories (i) and (ii), respectively. However, the differences in the survival rates between patients with CT categories (i) and (ii) were insignificant, although those in the latter category had significantly better survival rates than those with CT-diagnosed extra-pancreatic extension (category (iii)).
Conclusions
CT-diagnosed extra-pancreatic extension was a better prognostic factor than pathology-diagnosed extension and considered an independent factor for the postoperative DFS and OS rates with reasonable frequency and high reproducibility, despite the low diagnostic accuracy for predicting pathology-diagnosed extra-pancreatic extension.
Key Points
• A CT-diagnosed extra-pancreatic extension had a higher hazard ratio for both disease-free survival and overall survival compared to pathology-diagnosed extension in univariable survival analyses.
• A CT-diagnosed extra-pancreatic extension was a significant independent predictor of both disease-free survival and overall survival, as observed in multivariable survival analyses.
• Patients with tumours contacting with the pancreatic surface on CT images (CT category (ii)) showed similar survival rates to those whose tumours were surrounded by the pancreatic parenchyma (CT category (i)), although many tumours with CT category (ii) extended pathologically beyond the pancreas.





Similar content being viewed by others
Abbreviations
- 95% CI:
-
95% confidence interval
- DFS:
-
Disease-free survival
- HR:
-
Hazard ratio
- LN:
-
Lymph nodule
- NCCN:
-
National Comprehensive Cancer Network
- OS:
-
Overall survival
- PDAC:
-
Pancreatic ductal adenocarcinoma
- UICC:
-
Union for International Cancer Control
References
Fitzgerald TL, Hickner ZJ, Schmitz M, Kort EJ (2008) Changing incidence of pancreatic neoplasms: a 16-year review of stagewide tumor registry. Pancreas 37:134–138
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30
Winter JM, Cameron JL, Campbell KA et al (2006) 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 10:1199–1211
Jiang Y, Su Y, Chen Y, Li Z (2017) Refining the American Joint Committee on Cancer staging scheme for resectable pancreatic ductal adenocarcinoma using recursive partitioning analysis. J Cancer 8:2765–2773
Kamarajah SK, Burns WR, Frankel TL, Cho CS, Nathan H (2017) Validation of the American Joint Commission on Cancer (AJCC) 8th edition staging system for patients with pancreatic adenocarcinoma: a Surveillance, Epidemiology, and End Results (SEER) analysis. Ann Surg Oncol 24:2023–2030
van Roessel S, Kasumova GG, Veheji J et al (2018) International validation of the eighth edition of the American Joint Committee on Cancer (AJCC) TNM staging system in patients with resected pancreatic cancer. JAMA Surg 153:e183617
Saka B, Balci S, Basturk O et al (2016) Pancreatic ductal adenocarcinoma is spread to the peripancreatic soft tissue in the majority of resected cases, rendering the AJCC T-stage protocol (7th edition) inapplicable and insignificant: a size-based staging system (pT1:≤2, pT2:>2-≤4, pT3:>4 cm) is more valid and clinically relevant. Ann Surg Oncol 23:2010–2018
Jamieson NB, Foulis AK, Oien KA et al (2011) Peripancreatic fat invasion is an independent predictor of poor outcome following pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. J Gastrointest Surg 15:512–524
Park H, An S, Eo SH et al (2014) Survival effect of tumor size and extrapancreatic extension in surgically resected pancreatic cancer: proposal for improved T classification. Hum Pathol 45:2341–2346
Adsay NV, Bagci P, Tajiri T et al (2012) Pathologic staging of pancreatic, ampullary, biliary, and gallbladder cancers: pitfalls and practical limitations of the current AJCC/UICC TNM staging system and opportunities for improvement. Semin Diagn Pathol 29:127–141
Matsumoto S, Mori H, Kiyonaga M et al (2012) “Peripancreatic strands appearance” in pancreatic body and tail carcinoma: evaluation by multi-detector CT with pathological correlation. Abdom Imaging 37:602–608
National Comprehensive Cancer Network Pancreatic adenocarcinoma (version 1. 2021). Available via https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed 2 February 2021
Bae JS, Kim JH, Joo I, Chang W, Han JK (2019) MDCT findings predicting post-operative residual tumor and survival in patients with pancreatic cancer. Eur Radiol 29:3714–3724
Chang ST, Jeffrey RB, Patel BN et al (2016) Preoperative multidetector CT diagnosis of extrapancreatic perineural or duodenal invasion is associated with reduced postoperative survival after pancreaticoduodenectomy for pancreatic adenocarcinoma: preliminary experience and implications for patient care. Radiology 281:816–825
Park SJ, Kim JH, Joo I et al (2020) Important CT and histopathological findings for recurrence and overall survival in patients with pancreatic ductal adenocarcinoma who underwent surgery after neoadjuvant FOLFIRINOX. Eur Radiol 31:3616–3626
Kim JH, Eun HW, Kim KW et al (2013) Diagnostic performance of MDCT for predicting important prognostic factors in pancreatic cancer. Pancreas 42:1316–1322
Mochizuki K, Gabata T, Kozaka K et al (2010) MDCT findings of extrapancreatic nerve plexus invasion by pancreatic head carcinoma: correlation with en bloc pathological specimens and diagnostic accuracy. Eur Radiol 20:1757–1767
Ma C, Yang P, Li J, Bian Y, Wang L, Lu J (2020) Pancreatic adenocarcinoma: variability in measurements of tumor size among computed tomography, magnetic resonance imaging, and pathologic specimens. Abdom Radiol (NY) 45:782–788
Janssen QP, Buettner S, Suker M et al (2019) Neoadjuvant FOLFIRINOX in patients with borderline resectable pancreatic cancer: a systematic review and patient-level meta-analysis. J Natl Cancer Inst 111:782–794
Dhir M, Zenati MS, Hamad A et al (2018) FOLFIRINOX versus gemcitabine/nab-paclitaxel for neoadjuvant treatment of resectable and borderline resectable pancreatic head adenocarcinoma. Ann Surg Oncol 25:1896–1903
Zins M, Matos C, Cassinotto C et al (2018) Pancreatic adenocarcinoma staging in the era of preoperative chemotherapy and radiation therapy. Radiology 287:374–390
Park S, Jang JK, Byun JH et al (2021) CT in the prediction of margin-negative resection in pancreatic cancer following neoadjuvant treatment: a systematic review and meta-analysis. Eur Radiol 31:3383–3393
Jang JK, Byun JH, Kang JH et al (2021) CT-determined resectability of borderline resectable and unresectable pancreatic adenocarcinoma following FOLFIRINOX therapy. Eur Radiol 31:813–823
Marchegiani G, Todaro V, Boninsegna E et al (2018) Surgery after FOLFIRINOX treatment for locally advanced and borderline resectable pancreatic cancer: increase in tumour attenuation on CT correlates with R0 resection. Eur Radiol 28:4265–4273
Wanger M, Antunes C, Pietrasz D et al (2017) CT evaluation after neoadjuvant FOLFIRINOX chemotherapy for borderline and locally advanced pancreatic adenocarcinoma. Eur Radiol 27:3104–3116
Joo I, Lee JM, Lee ES et al (2018) Preoperative MDCT assessment of resectability in borderline resectable pancreatic cancer: effect of neoadjuvant chemoradiation therapy. AJR Am J Roentgenol 210:1059–1065
Kim YE, Park MS, Hong HS et al (2009) Effects of neoadjuvant combined chemotherapy and radiation therapy on the CT evaluation of resectability and staging in patients with pancreatic head cancer. Radiology 250:758–765
Cassinotto C, Cortade J, Belleannée G et al (2013) An evaluation of the accuracy of CT when determining resectability of pancreatic head adenocarcinoma after neoadjuvant treatment. Eur J Radiol 82:589–593
Pietrasz D, Marthey L, Wagner M et al (2015) Pathologic major response after FOLFIRINOX is prognostic for patients secondary resected for borderline or locally advanced pancreatic adenocarcinoma: an AGEO-FRENCH, prospective, multicentric cohort. Ann Surg Oncol 22:s1196–s1205
Ferrone CR, Marchegiani G, Hong TS et al (2015) Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg 261:12–17
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dai Inoue, M.D., Ph.D.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toshima, F., Inoue, D., Yoshida, K. et al. CT-diagnosed extra-pancreatic extension of pancreatic ductal adenocarcinoma is a more reliable prognostic factor for survival than pathology-diagnosed extension. Eur Radiol 32, 22–33 (2022). https://doi.org/10.1007/s00330-021-08180-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08180-6