Abstract
Purpose
Oral anticoagulants are crucial for preventing systemic thromboembolism in atrial fibrillation (AF), with guidelines preferring non-vitamin K antagonist oral anticoagulants (NOACs) over vitamin K antagonists (VKAs) in the general AF population. However, as NOACs are administered in fixed doses, concerns of unintentional underdosing in morbidly obese patients and unintentional overdosing in underweight patients have emerged. Therefore, a critical appraisal of the benefit-risk profile of NOACs in AF patients across the body weight spectrum is needed.
Methods and Results
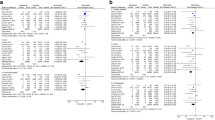
After searching Medline, this systematic review discusses the impact of body weight on the risk-benefit profile of NOACs versus VKAs. The meta-analysis demonstrated that NOAC use in obese and class III obese AF patients (body mass index (BMI) ≥ 30 and ≥ 40 kg/m2, respectively) was associated with significantly lower stroke/systemic embolism (stroke/SE) risks (RR 0.82, 95%CI [0.71–0.96] and RR 0.75, 95%CI [0.64–0.87], respectively), similar to lower major bleeding risks (RR 0.83, 95%CI [0.69–1.00] and RR 0.74, 95%CI [0.57–0.95], respectively) and similar mortality risks (RR 0.92, 95%CI [0.73–1.15] and RR 1.17, 95%CI [0.83–1.64], respectively) compared to VKAs. In AF patients ≤ 60 kg, significantly lower stroke/SE (RR 0.63, 95%CI [0.56–0.71]) and major bleeding risks (RR 0.71, 95%CI [0.62–0.80]), but similar mortality risks (RR 0.68, 95%CI [0.42–1.10]), were observed for NOAC- versus VKA-treated patients.
Conclusion
The benefit-risk profile of NOACs seems preserved in (morbidly) obese AF patients and patients with low body weight. However, more data are needed on underweight AF patients (BMI < 18.5 kg/m2) and on differences between NOACs in these patients.





Similar content being viewed by others
Data Availability
The data underlying this article are available in the article and in its online supplemental materials.
References
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330–93.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. Stroke. 1991;22(8):983–8.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Eliquis. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/eliquis-epar-product-information_en.pdf. Accessed 10 July 2020
Lixiana. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/lixiana-epar-product-information_en.pdf. Accessed 10 July 2020
Pradaxa. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/pradaxa-epar-product-information_en.pdf. Accessed 10 July 2020
Xarelto. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/xarelto-epar-product-information_en.pdf. Accessed 10 July 2020
World Health Organization (WHO) Body mass index (BMI) classification. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 10 July 2020.
Upreti VV, Wang J, Barrett YC, Byon W, Boyd RA, Pursley J, et al. Effect of extremes of body weight on the pharmacokinetics, pharmacodynamics, safety and tolerability of apixaban in healthy subjects. Br J Clin Pharmacol. 2013;76(6):908–16.
Yamashita T, Koretsune Y, Yasaka M, Inoue H, Kawai Y, Yamaguchi T, et al. Randomized, multicenter, warfarin-controlled phase II study of edoxaban in Japanese patients with non-valvular atrial fibrillation. Circ J. 2012;76(8):1840–7.
Boriani G, Ruff CT, Kuder JF, Shi M, Lanz HJ, Rutman H, et al. Relationship between body mass index and outcomes in patients with atrial fibrillation treated with edoxaban or warfarin in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2019;40(19):1541–50.
Reilly PA, Lehr T, Haertter S, Connolly SJ, Yusuf S, Eikelboom JW, et al. The effect of dabigatran plasma concentrations and patient characteristics on the frequency of ischemic stroke and major bleeding in atrial fibrillation patients: the RE-LY Trial (Randomized Evaluation of Long-Term Anticoagulation Therapy). J Am Coll Cardiol. 2014;63(4):321–8.
Kubitza D, Becka M, Zuehlsdorf M, Mueck W. Body weight has limited influence on the safety, tolerability, pharmacokinetics, or pharmacodynamics of rivaroxaban (BAY 59-7939) in healthy subjects. J Clin Pharmacol. 2007;47(2):218–26.
Hohnloser SH, Fudim M, Alexander JH, Wojdyla DM, Ezekowitz JA, Hanna M, et al. Efficacy and safety of apixaban versus warfarin in patients with atrial fibrillation and extremes in body weight. Circulation. 2019;139(20):2292–300.
Kmet L, Lee R, Cook L (2004) The quality assessment tool ‘QUALSYST’ from the “Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields”. https://www.ihe.ca/advanced-search/standard-quality-assessment-criteria-for-evaluating-primary-research-papers-from-a-variety-of-fields. Accessed 1 August 2020
Boehringer Ingelheim Pharmaceuticals. FDA Briefing Information, Dabigatran Etexilate Mesylate Capsules, for the September 20, 2010 Meeting of the Cardiovascular and Renal Drugs Advisory Committee. https://wayback.archive-it.org/7993/20170405212218/https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/CardiovascularandRenalDrugsAdvisoryCommittee/UCM247244.pdf. Accessed 10 July 2020
Balla SR, Cyr DD, Lokhnygina Y, Becker RC, Berkowitz SD, Breithardt G, et al. Relation of risk of stroke in patients with atrial fibrillation to body mass index (from patients treated with rivaroxaban and warfarin in the rivaroxaban once daily oral direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation trial). Am J Cardiol. 2017;119(12):1989–96.
Sandhu RK, Ezekowitz J, Andersson U, Alexander JH, Granger CB, Halvorsen S, et al. The 'obesity paradox’ in atrial fibrillation: observations from the ARISTOTLE (Apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation) trial. Eur Heart J. 2016;37(38):2869–78.
Eikelboom JW, Wallentin L, Connolly SJ, Ezekowitz M, Healey JS, Oldgren J, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2011;123(21):2363–72.
Proietti M, Guiducci E, Cheli P, Lip GY. Is there an obesity paradox for outcomes in atrial fibrillation? A systematic review and meta-analysis of non-vitamin K antagonist Oral anticoagulant trials. Stroke. 2017;48(4):857–66.
Malik AH, Yandrapalli S, Shetty S, Aronow WS, Jain D, Frishman WH, et al. Impact of weight on the efficacy and safety of direct-acting oral anticoagulants in patients with non-valvular atrial fibrillation: a meta-analysis. Europace. 2020;22(3):361–7.
Costa OS, Beyer-Westendorf J, Ashton V, Milentijevic D, Moore KT, Bunz TJ, et al. Effectiveness and safety of rivaroxaban versus warfarin in obese nonvalvular atrial fibrillation patients: analysis of electronic health record data. Curr Med Res Opin. 2020;36(7):1081–8.
Deitelzweig S, Keshishian A, Kang A, et al. Effectiveness and safety of oral anticoagulants among NVAF patients with obesity: insights from the ARISTOPHANES study. J Clin Med. 2020;9(6):1633. https://doi.org/10.3390/jcm9061633.
Peterson ED, Ashton V, Chen YW, Wu B, Spyropoulos AC. Comparative effectiveness, safety, and costs of rivaroxaban and warfarin among morbidly obese patients with atrial fibrillation. Am Heart J. 2019;212:113–9.
Patil T, Lebrecht M. A single center retrospective cohort study evaluating use of direct oral anticoagulants (DOACs) in morbidly obese veteran population. Thromb Res. 2020;192:124–30.
Patti G, Pecen L, Manu MC, Huber K, Rohla M, Renda G, et al. Thromboembolic and bleeding risk in obese patients with atrial fibrillation according to different anticoagulation strategies. Int J Cardiol. 2020;318:67–73.
Kido K, Shimizu M, Shiga T, Hashiguchi M. Meta-analysis comparing direct oral anticoagulants versus warfarin in morbidly obese patients with atrial fibrillation. Am J Cardiol. 2020;126:23–8.
Boehringer Ingelheim. Pradaxa (dabigatran), U.S. Food and Drug Administration Highlights of Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022512s027lbl.pdf. Accessed 10 July 2020
Xarelto (rivaroxaban). U.S. food and drug administration highlights of prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022406s028lbl.pdf. Accessed 10 July 2020
Savaysa (edoxaban). U.S. food and drug administration highlights of prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206316lbl.pdf. Accessed 10 July 2020
Lee SR, Choi EK, Park CS, Han KD, Jung JH, Oh S, et al. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019;73(8):919–31.
Russo V, Attena E, Di Maio M, et al. Non-vitamin K vs vitamin K oral anticoagulants in patients aged > 80 year with atrial fibrillation and low body weight. Eur J Clin Investig. 2020;50(11):e13335. https://doi.org/10.1111/eci.13335.
Hori M, Connolly SJ, Zhu J, Liu LS, Lau CP, Pais P, et al. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke. 2013;44(7):1891–6.
Chiang C-E, Wang K-L, Lip GYH. Stroke prevention in atrial fibrillation: an Asian perspective. Thromb Haemost. 2014;111(5):789–97.
Chao TF, Chen SA, Ruff CT, Hamershock RA, Mercuri MF, Antman EM, et al. Clinical outcomes, edoxaban concentration, and anti-factor Xa activity of Asian patients with atrial fibrillation compared with non-Asians in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2019;40(19):1518–27.
Piccini JP, Hellkamp AS, Lokhnygina Y, Patel MR, Harrell FE, Singer DE, et al. Relationship between time in therapeutic range and comparative treatment effect of rivaroxaban and warfarin: results from the ROCKET AF trial. J Am Heart Assoc. 2014;3(2):e000521.
Funding
This research was supported by grants from the Fund for Scientific Research Flanders (FWO) [grant number 11C0820N to Maxim Grymonprez].
Author information
Authors and Affiliations
Contributions
Maxim Grymonprez and Lies Lahousse contributed to the concept and design of the systematic review. Maxim Grymonprez performed the literature search, data analysis, interpretation and writing. The first draft of the manuscript was written by Maxim Grymonprez. Tine De Backer, Stephane Steurbaut, Koen Boussery and Lies Lahousse revised the manuscript critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 1342 kb)
Rights and permissions
About this article
Cite this article
Grymonprez, M., De Backer, T.L., Steurbaut, S. et al. Non-Vitamin K Antagonist Oral Anticoagulants (NOACs) Versus Warfarin in Patients with Atrial Fibrillation and (Morbid) Obesity or Low Body Weight: a Systematic Review and Meta-Analysis. Cardiovasc Drugs Ther 36, 749–761 (2022). https://doi.org/10.1007/s10557-020-07122-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-07122-6