Abstract
Purpose
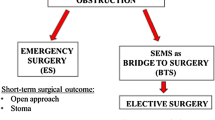
After almost three decades since the first description of colonic stents, the controversies of its safe application continue to impede the readiness of adoption by clinicians for malignant left bowel obstruction. This review seeks to address some of the controversial aspects of stenting and its impact on surgical and oncological outcomes.
Methods
Medline, Embase, and CNKI were searched for articles employing SEMS for left colonic obstruction. Outcomes analyzed include success rates, complications, and long-term survival. Pooled risk ratio (RR) and 95% confidence interval (CI) were estimated.
Results
36 studies were included with 2002 patients across seven randomized controlled trials and 29 observational studies. High technical (92%) and clinical (82%) success rates, and low rates of complications, including perforation (5%), were found. Those with > 8% perforation rates had poorer technical success rates than those with ≤ 8%, but there were no significant differences in 90-day in-hospital mortality and three and 5-year overall and disease-free survival. A significant increase was found in technical (RR = 1.094; CI, 1.041–1.149; p < 0.001) and clinical (RR = 1.158; CI, 1.064–1.259; p = 0.001) success rates when the duration between stenting and surgery was ≥ 2 weeks compared to < 2 weeks, but there were no significant differences in perforation rates, 90-day in-hospital mortality, and long-term survival.
Conclusions
Colonic stenting is safe and effective with high success rates and low complication rates. However, outcomes of higher perforation rates and optimal timing from stent till surgery remain unclear, with only a few studies reporting on these outcomes, leaving areas for future research.







Similar content being viewed by others
References
Jain SR, Yaow CYL, Ng CH, Neo VSQ, Lim F, Foo FJ, Wong NW, Chong CS (2020) Comparison of colonic stents, stomas and resection for obstructive left colon cancer: a meta-analysis. Techn Coloproctol 24(11):1121–1136. https://doi.org/10.1007/s10151-020-02296-5
Williams D, Law R, Pullyblank AM (2011) Colorectal stenting in malignant large bowel obstruction: the learning curve. Int J Surg Oncol 2011:917848–917844. https://doi.org/10.1155/2011/917848
Rodrigues-Pinto E, Morais R, Coelho C, Pereira P, Repici A, Macedo G (2019) Bridge-to-surgery versus emergency surgery in the management of left-sided acute malignant colorectal obstruction - efficacy, safety and long-term outcomes. Dig Liver Dis 51(3):364–372. https://doi.org/10.1016/j.dld.2018.11.006
Baron TH (2014) Technique of colonic stenting. Tech Gastrointest Endosc 16(3):108–111
Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Sagar J (2013) Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol 22(1):14–21. https://doi.org/10.1016/j.suronc.2012.10.003
Tang MH, Ross T, Yeo SA, Ng CY (2019) Colonic stenting for malignant large bowel obstruction is safe and effective: a single-surgeon experience. Singapore Med J 60(7):347–352. https://doi.org/10.11622/smedj.2019010
Kim HJ, Choi G-S, Park JS, Park SY, Jun SH (2013) Higher rate of perineural invasion in stent–laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Color Dis 28(3):407–414. https://doi.org/10.1007/s00384-012-1556-x
Repici A, de Paula Pessoa Ferreira D (2011) Expandable metal stents for malignant colorectal strictures. Gastrointest Endosc Clin N Am 21(3):511–533, ix. https://doi.org/10.1016/j.giec.2011.04.005
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A (2020) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2020. Endoscopy 52(5):389–407. https://doi.org/10.1055/a-1140-3017
Lee H, Bae SU, Baek SK, Jeong WK (2017) Comparison of early and late surgery following colonic stenting for obstructive colorectal cancer. Korean J Clin Oncol 13(2):96–101. https://doi.org/10.14216/kjco.17014
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Ho KS, Quah HM, Lim JF, Tang CL, Eu KW (2012) Endoscopic stenting and elective surgery versus emergency surgery for left-sided malignant colonic obstruction: a prospective randomized trial. Int J Color Dis 27(3):355–362. https://doi.org/10.1007/s00384-011-1331-4
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):13. https://doi.org/10.1186/1471-2288-5-13
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135. https://doi.org/10.1186/1471-2288-14-135
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N (2006) Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol 59(1):7–10. https://doi.org/10.1016/j.jclinepi.2005.06.006
Nyaga VN, Arbyn M, Aerts M (2014) Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72(1):39. https://doi.org/10.1186/2049-3258-72-39
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Koo CH, Chang JHE, Syn NL, Wee IJY, Mathew R (2020) Systematic review and meta-analysis on colorectal cancer findings on colonic evaluation after CT-confirmed acute diverticulitis. Dis Colon Rectum 63(5):701–709. https://doi.org/10.1097/dcr.0000000000001664
Ow ZGW, Jain SR, Ng CH (2020) Letter to the editor: midterm results of a contemporary, porous-coated acetabular system in patients undergoing primary total hip replacement for degenerative hip disease: a prospective, multicenter Study. J Arthroplast. https://doi.org/10.1016/j.arth.2020.07.079
Katz D, Baptista J, Azen SP, Pike MC (1978) Obtaining confidence intervals for the risk ratio in cohort studies. Biometrics 34(3):469–474. https://doi.org/10.2307/2530610
Harbord RM, Higgins JPT (2008) Meta-regression in Stata. Stata J 8(4):493–519. https://doi.org/10.1177/1536867X0800800403
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2000) The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. https://www.researchgate.net/publication/261773681_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_the_Quality_of_Non-Randomized_Studies_in_Meta-Analysis
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
McGuinness L, Higgins J (2020) Risk-Of-Bias VISualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. https://doi.org/10.1002/jrsm.1411
Ghazal AH, El-Shazly WG, Bessa SS, El-Riwini MT, Hussein AM (2013) Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg 17(6):1123–1129. https://doi.org/10.1007/s11605-013-2152-2
Öistämö E, Hjern F, Blomqvist L, Falkén Y, Pekkari K, Abraham-Nordling M (2016) Emergency management with resection versus proximal stoma or stent treatment and planned resection in malignant left-sided colon obstruction. World J Surg Oncol 14(1):232–232. https://doi.org/10.1186/s12957-016-0994-2
Li ZZQ, Ma Y, Zhang Q, Li S, Yu T (2019) Self-expanding metallic stent implantation in treatment of acute left-side malignant colorectal obstruction. Chin J Interv Imaging Ther 16(4):211–214. https://doi.org/10.13929/j.1672-8475.201807024
Han L, Song X, Yu B, Zhou M, Zhang L, Sun G (2020) Safety evaluation of preoperative stent insertion and clinical analysis on comparison of outcomes between preoperative stent insertion and emergency surgery in the treatment of obstructive left-sided colorectal cancer. Pak J Med Sci 36(3):376–381. https://doi.org/10.12669/pjms.36.3.1707
Kawachi J, Kashiwagi H, Shimoyama R, Isogai N, Fukai R, Miyake K, Egashira H, Sugitani A, Ogino H (2018) Comparison of efficacies of the self-expandable metallic stent versus transanal drainage tube and emergency surgery for malignant left-sided colon obstruction. Asian J Surg 41(5):498–505. https://doi.org/10.1016/j.asjsur.2017.06.003
Shimizu H, Yamazaki R, Ohtsuka H, Osaka I, Takuma K, Morita Y (2018) Feasibility of laparoscopic surgery after stent insertion for obstructive colorectal cancer. Asian J Endosc Surg 11(2):118–122. https://doi.org/10.1111/ases.12434
Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL (2011) Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 25(6):1814–1821. https://doi.org/10.1007/s00464-010-1471-6
Sabbagh C, Browet F, Diouf M, Cosse C, Brehant O, Bartoli E, Mauvais F, Chauffert B, Dupas JL, Nguyen-Khac E, Regimbeau JM (2013) Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg 258(1):107–115. https://doi.org/10.1097/SLA.0b013e31827e30ce
Mege D, Sabbagh C, Manceau G, Bridoux V, Lakkis Z, Momar D, Sielezneff I, Karoui M (2019) What is the best option between primary diverting stoma or endoscopic stent as a bridge to surgery with a curative intent for obstructed left colon cancer? Results from a propensity score analysis of the French surgical association multicenter cohort of 518 patients. Ann Surg Oncol 26(3):756–764. https://doi.org/10.1245/s10434-018-07139-0
Occhionorelli S, Tartarini D, Cappellari L, Stano R, Vasquez G (2014) Colonic stent placement as a bridge to surgery in patients with left-sided malignant large bowel obstruction. An observational study. G Chir 35(11–12):283–289
Parodi A, De Ceglie A, De Luca L, Conigliaro R, Naspetti R, Arpe P, Coccia G, Conio M (2016) Endoscopic stenting as bridge-to-surgery (BTS) in left-sided obstructing colorectal cancer: experience with conformable stents. Clin Res Hepatol Gastroenterol 40(5):638–644. https://doi.org/10.1016/j.clinre.2016.03.007
Arezzo A, Balague C, Targarona E, Borghi F, Giraudo G, Ghezzo L, Arroyo A, Sola-Vera J, De Paolis P, Bossotti M, Bannone E, Forcignano E, Bonino MA, Passera R, Morino M (2017) Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc 31(8):3297–3305. https://doi.org/10.1007/s00464-016-5362-3
Johnson R, Marsh R, Corson J, Seymour K (2004) A comparison of two methods of palliation of large bowel obstruction due to irremovable colon cancer. Ann R Coll Surg Engl 86(2):99–103. https://doi.org/10.1308/003588404322827473
Knight AL, Trompetas V, Saunders MP, Anderson HJ (2012) Does stenting of left-sided colorectal cancer as a “bridge to surgery” adversely affect oncological outcomes? A comparison with non-obstructing elective left-sided colonic resections. Int J Color Dis 27(11):1509–1514. https://doi.org/10.1007/s00384-012-1513-8
Gorissen KJ, Tuynman JB, Fryer E, Wang L, Uberoi R, Jones OM, Cunningham C, Lindsey I (2013) Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg 100(13):1805–1809. https://doi.org/10.1002/bjs.9297
Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK (2009) Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg 144(12):1127–1132. https://doi.org/10.1001/archsurg.2009.216
Quereshy FA, Poon JT, Law WL (2014) Long-term outcome of stenting as a bridge to surgery for acute left-sided malignant colonic obstruction. Color Dis 16(10):788–793. https://doi.org/10.1111/codi.12666
Ho KM, Chan KM, Kwok SY, Lau PY (2017) Colonic self-expanding metal stent (SEMS) as a bridge to surgery in left-sided malignant colonic obstruction: an 8-year review. Surg Endosc 31(5):2255–2262. https://doi.org/10.1007/s00464-016-5227-9
Tung KL, Cheung HY, Ng LW, Chung CC, Li MK (2013) Endo-laparoscopic approach versus conventional open surgery in the treatment of obstructing left-sided colon cancer: long-term follow-up of a randomized trial. Asian J Endosc Surg 6(2):78–81. https://doi.org/10.1111/ases.12030
van Hooft JE, Fockens P, Marinelli AW, Timmer R, van Berkel AM, Bossuyt PM, Bemelman WA (2008) Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy 40(3):184–191. https://doi.org/10.1055/s-2007-995426
Amelung FJ, Borg FT, Consten EC, Siersema PD, Draaisma WA (2016) Deviating colostomy construction versus stent placement as bridge to surgery for malignant leftsided colonic obstruction. Eur Surg Res 57:15–16. https://doi.org/10.1159/446131
Amelung FJ, Borstlap WAA, Consten ECJ, Veld JV, van Halsema EE, Bemelman WA, Siersema PD, Ter Borg F, van Hooft JE, Tanis PJ (2019) Propensity score-matched analysis of oncological outcome between stent as bridge to surgery and emergency resection in patients with malignant left-sided colonic obstruction. Br J Surg 106(8):1075–1086. https://doi.org/10.1002/bjs.11172
Veld JV, Amelung FJ, Borstlap WAA, van Halsema EE, Consten ECJ, Siersema PD, ter Borg F, van der Zaag ES, de Wilt JHW, Fockens P, Bemelman WA, van Hooft JE, Tanis PJ, Group ftDSR (2020) Comparison of decompressing stoma vs stent as a bridge to surgery for left-sided obstructive colon cancer. JAMA Surg 155(3):206–215. https://doi.org/10.1001/jamasurg.2019.5466
Chung TS, Lim SB, Sohn DK, Hong CW, Han KS, Choi HS, Jeong SY (2008) Feasibility of single-stage laparoscopic resection after placement of a self-expandable metallic stent for obstructive left colorectal cancer. World J Surg 32(10):2275–2280. https://doi.org/10.1007/s00268-008-9695-5
Kim JS, Hur H, Min BS, Sohn SK, Cho CH, Kim NK (2009) Oncologic outcomes of self-expanding metallic stent insertion as a bridge to surgery in the management of left-sided colon cancer obstruction: comparison with nonobstructing elective surgery. World J Surg 33(6):1281–1286. https://doi.org/10.1007/s00268-009-0007-5
Kim JH, Kwon KA, Lee JJ, Lee W-S, Baek J-H, Kim YJ, Chung J-W, Kim KO, Park DK, Kim JH (2014) Surgical failure after colonic stenting as a bridge to surgery. World J Gastroenterol 20(33):11826–11834. https://doi.org/10.3748/wjg.v20.i33.11826
Kim MK, Kye BH, Lee IK, Oh ST, Ahn CH, Lee YS, Lee SC, Kang WK (2017) Outcome of bridge to surgery stenting for obstructive left colon cancer. ANZ J Surg 87(12):E245–e250. https://doi.org/10.1111/ans.13525
Kang SI, Oh HK, Yoo JS, Ahn S, Kim MH, Kim MJ, Son IT, Kim DW, Kang SB, Park YS, Yoon CJ, Shin R, Heo SC, Lee IT, Youk EG, Kim MJ, Chang TY, Park SC, Sohn DK, Oh JH, Park JW, Ryoo SB, Jeong SY, Park KJ (2018) Oncologic outcomes of preoperative stent insertion first versus immediate surgery for obstructing left-sided colorectal cancer. Surg Oncol 27(2):216–224. https://doi.org/10.1016/j.suronc.2018.04.002
Mainar A, Tejero E, Maynar M, Ferral H, Castaneda-Zuniga W (1996) Colorectal obstruction: treatment with metallic stents. Radiology 198(3):761–764. https://doi.org/10.1148/radiology.198.3.8628867
Turegano-Fuentes F, Echenagusia-Belda A, Simo-Muerza G, Camunez F, Munoz-Jimenez F, Del Valle Hernandez E, Quintans-Rodriguez A (1998) Transanal self-expanding metal stents as an alternative to palliative colostomy in selected patients with malignant obstruction of the left colon. Br J Surg 85(2):232–235. https://doi.org/10.1046/j.1365-2168.1998.00565.x
Alcantara M, Serra-Aracil X, Falco J, Mora L, Bombardo J, Navarro S (2011) Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg 35(8):1904–1910. https://doi.org/10.1007/s00268-011-1139-y
Flor-Lorente B, Báguena G, Frasson M, García-Granero A, Cervantes A, Sanchiz V, Peña A, Espí A, Esclapez P, García-Granero E (2017) Self-expanding metallic stent as a bridge to surgery in the treatment of left colon cancer obstruction: cost-benefit analysis and oncologic results. Cir Esp 95(3):143–151. https://doi.org/10.1016/j.ciresp.2016.12.014
Ballestero Perez A, Garcia Perez JC, Muriel A, Die Trill J, Lobo E (2018) The long-term recurrence rate and survival of obstructive left-sided colon cancer patients: a stent as a bridge to surgery. Rev Esp Enferm Dig 110(11):718–725. https://doi.org/10.17235/reed.2018.5077/2017
Lara-Romero C, Vilches A, Caunedo-Alvarez A, Hergueta-Delgado P, Lavin-Castejon I, Andrade-Bellido R, Alcain-Martinez G (2019) Better recurrence-free survival after stent bridge to surgery compared to emergency surgery for obstructive left-sided colonic cancer in patients with stage III status of the American Joint Committee on Cancer (AJCC): a bicentric retrospective study. Int J Color Dis 34(7):1241–1250. https://doi.org/10.1007/s00384-019-03318-x
Frago R, Kreisler E, Biondo S, Salazar R, Dominguez J, Escalante E (2010) Outcomes in the management of obstructive unresectable stage IV colorectal cancer. Eur J Surg Oncol 36(12):1187–1194. https://doi.org/10.1016/j.ejso.2010.09.005
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99(4):469–476. https://doi.org/10.1002/bjs.8689
Liang TW, Sun Y, Wei YC, Yang DX (2014) Palliative treatment of malignant colorectal obstruction caused by advanced malignancy: a self-expanding metallic stent or surgery? A system review and meta-analysis. Surg Today 44(1):22–33. https://doi.org/10.1007/s00595-013-0665-7
Takahashi H, Okabayashi K, Tsuruta M, Hasegawa H, Yahagi M, Kitagawa Y (2015) Self-expanding metallic stents versus surgical intervention as palliative therapy for obstructive colorectal cancer: a meta-analysis. World J Surg 39(8):2037–2044. https://doi.org/10.1007/s00268-015-3068-7
Ihn MH, Lee SM, Son IT, Park JT, Oh HK, Kim DW, Kang SB (2015) Cultural adaptation and validation of the Korean version of the EORTC QLQ-CR29 in patients with colorectal cancer. Support Care Cancer 23(12):3493–3501. https://doi.org/10.1007/s00520-015-2710-0
Sagar J (2011, 2011) Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev (11):Cd007378. https://doi.org/10.1002/14651858.CD007378.pub2
Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L (2017) Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol 2017:2863272–2863211. https://doi.org/10.1155/2017/2863272
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ (2007) Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 246(1):24–30. https://doi.org/10.1097/01.sla.0000261124.72687.72
Amelung FJ, Burghgraef TA, Tanis PJ, van Hooft JE, Ter Borg F, Siersema PD, Bemelman WA, Consten ECJ (2018) Critical appraisal of oncological safety of stent as bridge to surgery in left-sided obstructing colon cancer; a systematic review and meta-analysis. Crit Rev Oncol Hematol 131:66–75. https://doi.org/10.1016/j.critrevonc.2018.08.003
Balciscueta I, Balciscueta Z, Uribe N, García-Granero E (2020) Long-term outcomes of stent-related perforation in malignant colon obstruction: a systematic review and meta-analysis. Int J Color Dis 35(8):1439–1451. https://doi.org/10.1007/s00384-020-03664-1
Avlund TH, Erichsen R, Ravn S, Ciplys Z, Andersen JC, Laurberg S, Iversen LH (2018) The prognostic impact of bowel perforation following self-expanding metal stent as a bridge to surgery in colorectal cancer obstruction. Surg Endosc 32(1):328–336. https://doi.org/10.1007/s00464-017-5680-0
Small AJ, Coelho-Prabhu N, Baron TH (2010) Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 71(3):560–572. https://doi.org/10.1016/j.gie.2009.10.012
Lim TZ, Chan DKH, Tan KK (2018) Endoscopic stenting should be advocated in patients with stage IV colorectal cancer presenting with acute obstruction. J Gastrointest Oncol 9(5):785–790. https://doi.org/10.21037/jgo.2018.06.03
Maruthachalam K, Lash GE, Shenton BK, Horgan AF (2007) Tumour cell dissemination following endoscopic stent insertion. Br J Surg 94(9):1151–1154. https://doi.org/10.1002/bjs.5790
Author information
Authors and Affiliations
Contributions
Vernicia Neo Shu Qi: literature search, data collection, analysis and interpretation, drafting the article, critical revision of article, and final approval.
Sneha Rajiv Jain: literature search, data collection, analysis and interpretation, drafting the article, critical revision of article, and final approval.
Yeo Jun Wei: literature search, data collection, analysis, and interpretation.
Ng Cheng Han: study conception, literature search, methodology, critical revision of article, and final approval.
Tiffany Gan Rui Xuan: data collection, drafting the article, and critical revision of article.
Emile Tan: critical revision of article and final approval.
Chong Choon Seng: study conception, methodology, data interpretation, critical revision of article, and final approval.
All authors have contributed to and agreed on the content of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neo, V.S.Q., Jain, S.R., Yeo, J.W. et al. Controversies of colonic stenting in obstructive left colorectal cancer: a critical analysis with meta-analysis and meta-regression. Int J Colorectal Dis 36, 689–700 (2021). https://doi.org/10.1007/s00384-021-03834-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03834-9