Abstract
During the past 85 years of antibiotic use, we have learned a great deal about how these ‘miracle’ drugs work. We know the molecular structures and interactions of these drugs and their targets and the effects on the structure, physiology and replication of bacteria. Collectively, we know a great deal about these proximate mechanisms of action for virtually all antibiotics in current use. What we do not know is the ultimate mechanism of action; that is, how these drugs irreversibly terminate the ‘individuality’ of bacterial cells by removing barriers to the external world (cell envelopes) or by destroying their genetic identity (DNA). Antibiotics have many different ‘mechanisms of action’ that converge to irreversible lethal effects. In this Perspective, we consider what our knowledge of the proximate mechanisms of action of antibiotics and the pharmacodynamics of their interaction with bacteria tell us about the ultimate mechanisms by which these antibiotics kill bacteria.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ehrlich, P. Address in pathology, on chemiotherapy: delivered before the Seventeenth International Congress of Medicine. Br. Med. J. 2, 353–359 (1913).
Wright, G., Hung, D. & Helmann, J. How antibiotics kill bacteria: new models needed? Nat. Med. 19, 544–545 (2013).
Levin, B. R. et al. A numbers game: ribosome densities, bacterial growth, and antibiotic-mediated stasis and death. mBio 8, e02253-16 (2017).
Mayr, E. Cause and effect in biology. Science 134, 1501–1506 (1961).
Laland, K. N., Sterelny, K., Odling-Smee, J., Hoppitt, W. & Uller, T. Cause and effect in biology revisited: is Mayr’s proximate-ultimate dichotomy still useful? Science 334, 1512–1516 (2011).
Ariew, A. Ernst Mayr’s ‘ultimate/proximate’ distinction reconsidered and reconstructed. Biol. Philos. 18, 553–565 (2003).
Medawar, P. The Uniqueness of the Individual (Methuen, 1957).
Venkobachar, C. L. & Rao, A. Mechanism of disinfection: effect of chlorine on cell membrane functions. Water Res. 11, 727–729 (1997).
Virto, R., Manas, P., Alvarez, I., Condon, S. & Raso, J. Membrane damage and microbial inactivation by chlorine in the absence and presence of a chlorine-demanding substrate. Appl. Env. Microbiol. 71, 5022–5028 (2005).
Regoes, R. R. et al. Pharmacodynamic functions: a multiparameter approach to the design of antibiotic treatment regimens. Antimicrob. Agents Chemother. 48, 3670–3676 (2004).
Southam, C. & Ehrlich, J. Effects of extracts of western redcedar heartwood on certain wood-decaying fungi in culture. Phytopathology 33, 517–524 (1943).
Davies, J., Spiegelman, G. B. & Yim, G. The world of subinhibitory antibiotic concentrations. Curr. Opin. Microbiol. 9, 445–453 (2006).
Linares, J. F., Gustafsson, I., Baquero, F. & Martinez, J. L. Antibiotics as intermicrobial signaling agents instead of weapons. Proc. Natl Acad. Sci. USA 103, 19484–19489 (2006).
Calabrese, E. J. Hormesis: a fundamental concept in biology. Microb. Cell 1, 145–149 (2014).
Calabrese, E. J. et al. Biological stress response terminology: integrating the concepts of adaptive response and preconditioning stress within a hormetic dose-response framework. Toxicol. Appl. Pharmacol. 222, 122–128 (2007).
Udekwu, K. I. & Levin, B. R. Staphylococcus aureus in continuous culture: a tool for the rational design of antibiotic treatment protocols. PLoS ONE 7, e38866 (2012).
Bigger, J. W. Treatment of staphylococcal infections with penicillin. Lancet 244, 497–500 (1944).
Balaban, N. Q. et al. Definitions and guidelines for research on antibiotic persistence. Nat. Rev. Microbiol. 17, 460 (2019).
Bailey, E. M., Rybak, M. J. & Kaatz, G. W. Comparative effect of protein binding on the killing activities of teicoplanin and vancomycin. Antimicrob. Agents Chemother. 35, 1089–1092 (1991).
Pages, J. M., James, C. E. & Winterhalter, M. The porin and the permeating antibiotic: a selective diffusion barrier in Gram-negative bacteria. Nat. Rev. Microbiol. 6, 893–903 (2008).
Nikaido, H. Multidrug efflux pumps of gram-negative bacteria. J. Bacteriol. 178, 5853–5859 (1996).
Poole, K. Efflux-mediated antimicrobial resistance. J. Antimicrob. Chemother. 56, 20–51 (2005).
Clarelli, F. et al. Drug-target binding quantitatively predicts optimal antibiotic dose levels. Preprint at bioRxiv https://doi.org/10.1101/369975 (2020).
Zhu, J. H. et al. Rifampicin can induce antibiotic tolerance in mycobacteria via paradoxical changes in rpoB transcription. Nat. Commun. 9, 4218 (2018).
Gabrielsson, J., Peletier, L. A. & Hjorth, S. In vivo potency revisited - keep the target in sight. Pharmacol. Ther. 184, 177–188 (2018).
Borisova, M., Gisin, J. & Mayer, C. Blocking peptidoglycan recycling in pseudomonas aeruginosa attenuates intrinsic resistance to fosfomycin. Microb. Drug Resist. 20, 231–237 (2014).
Miller, C. et al. SOS response induction by beta-lactams and bacterial defense against antibiotic lethality. Science 305, 1629–1631 (2004).
Jacoby, G. A. AmpC beta-lactamases. Clin. Microbiol. Rev. 22, 161–182 (2009).
Mainardi, J. L. et al. Novel mechanism of beta-lactam resistance due to bypass of DD-transpeptidation in Enterococcus faecium. J. Biol. Chem. 275, 16490–16496 (2000).
Flensburg, J. & Skold, O. Massive overproduction of dihydrofolate reductase in bacteria as a response to the use of trimethoprim. Eur. J. Biochem. 162, 473–476 (1987).
Piddock, L. J. & Walters, R. N. Bactericidal activities of five quinolones for Escherichia coli strains with mutations in genes encoding the SOS response or cell division. Antimicrob. Agents Chemother. 36, 819–825 (1992).
Kohanski, M. A., Dwyer, D. J., Hayete, B., Lawrence, C. A. & Collins, J. J. A common mechanism of cellular death induced by bactericidal antibiotics. Cell 130, 797–810 (2007).
Dorr, T., Lewis, K. & Vulic, M. SOS response induces persistence to fluoroquinolones in Escherichia coli. PLoS Genet. 5, e1000760 (2009).
Hong, Y., Zeng, J., Wang, X., Drlica, K. & Zhao, X. Post-stress bacterial cell death mediated by reactive oxygen species. Proc. Natl Acad. Sci. USA 116, 10064–10071 (2019).
McCall, I. C., Shah, N., Govindan, A., Baquero, F. & Levin, B. R. Antibiotic killing of diversely generated populations of nonreplicating bacteria. Antimicrob. Agents Chemother. 63, e02360-18 (2019).
Peeters, S. H. & de Jonge, M. I. For the greater good: programmed cell death in bacterial communities. Microbiol. Res. 207, 161–169 (2018).
Tuomanen, E., Cozens, R., Tosch, W., Zak, O. & Tomasz, A. The rate of killing of Escherichia coli by beta-lactam antibiotics is strictly proportional to the rate of bacterial growth. J. Gen. Microbiol. 132, 1297–1304 (1986).
Vogelman, B. & Craig, W. A. Kinetics of antimicrobial activity. J. Pediatr. 108, 835–840 (1986).
Russell, A. D. Mechanisms of antimicrobial action of antiseptics and disinfectants: an increasingly important area of investigation. J. Antimicrob. Chemother. 49, 597–599 (2002).
Maillard, J. Y. Bacterial target sites for biocide action. J. Appl. Microbiol. 92, 16S–27S (2002).
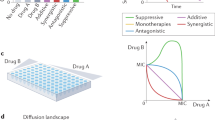
Eliopoulos, G. M. & Eliopoulos, C. T. Antibiotic combinations: should they be tested? Clin. Microbiol. Rev. 1, 139–156 (1988).
Chaudhry, W. N. et al. Synergy and order effects of antibiotics and phages in killing pseudomonas aeruginosa biofilms. PLoS ONE 12, e0168615 (2017).
Dickey, J. & Perrot, V. Adjunct phage treatment enhances the effectiveness of low antibiotic concentration against Staphylococcus aureus biofilms in vitro. PLoS ONE 14, e0209390 (2019).
Morrissey, I. Bactericidal index: a new way to assess quinolone bactericidal activity in vitro. J. Antimicrob. Chemother. 39, 713–717 (1997).
Gottardi, W., Klotz, S. & Nagl, M. Superior bactericidal activity of N-bromine compounds compared to their N-chlorine analogues can be reversed under protein load. J. Appl. Microbiol. 116, 1427–1437 (2014).
Barry, A. L. et al. Methods for determining bactericidal activity of antimicrobial agents, approved guideline (CLSI, 1999).
Yang, J. H., Bening, S. C. & Collins, J. J. Antibiotic efficacy-context matters. Curr. Opin. Microbiol. 39, 73–80 (2017).
Epand, R. M., Walker, C., Epand, R. F. & Magarvey, N. A. Molecular mechanisms of membrane targeting antibiotics. Biochim. Biophys. Acta 1858, 980–987 (2016).
Harrison, S. T. Bacterial cell disruption: a key unit operation in the recovery of intracellular products. Biotechnol. Adv. 9, 217–240 (1991).
Harrison, S. T., Dennis, J. S. & Chase, H. A. in Inhibition and Destruction of the Microbial Cell (ed. Hugo, W. B.) 95–105 (Academic, 1971).
Mosser, J. L. & Tomasz, A. Choline-containing teichoic acid as a structural component of pneumococcal cell wall and its role in sensitivity to lysis by an autolytic enzyme. J. Biol. Chem. 245, 287–298 (1970).
Garcia, P., Paz Gonzalez, M., Garcia, E., Garcia, J. L. & Lopez, R. The molecular characterization of the first autolytic lysozyme of Streptococcus pneumoniae reveals evolutionary mobile domains. Mol. Microbiol. 33, 128–138 (1999).
Rice, K. C. & Bayles, K. W. Molecular control of bacterial death and lysis. Microbiol. Mol. Biol. Rev. 72, 85–109 (2008).
Kitano, K. & Tomasz, A. Triggering of autolytic cell wall degradation in Escherichia coli by beta-lactam antibiotics. Antimicrob. Agents Chemother. 16, 838–848 (1979).
Shin, J. H. et al. Structural basis of peptidoglycan endopeptidase regulation. Proc. Natl Acad. Sci. USA 117, 11692–11702 (2020).
Wecke, J., Perego, M. & Fischer, W. D-Alanine deprivation of Bacillus subtilis teichoic acids is without effect on cell growth and morphology but affects the autolytic activity. Microb. Drug Resist. 2, 123–129 (1996).
Silhavy, T. J., Kahne, D. & Walker, S. The bacterial cell envelope. Cold Spring Harb. Perspect. Biol. 2, a000414 (2010).
Flores-Kim, J., Dobihal, G. S., Fenton, A., Rudner, D. Z. & Bernhardt, T. G. A switch in surface polymer biogenesis triggers growth-phase-dependent and antibiotic-induced bacteriolysis. eLife 8, e44912 (2019).
Bittner, L. M., Arends, J. & Narberhaus, F. When, how and why? Regulated proteolysis by the essential FtsH protease in Escherichia coli. Biol. Chem. 398, 625–635 (2017).
Parsons, J. B., Yao, J., Jackson, P., Frank, M. & Rock, C. O. Phosphatidylglycerol homeostasis in glycerol-phosphate auxotrophs of Staphylococcus aureus. BMC Microbiol. 13, 260 (2013).
May, K. L. & Silhavy, T. J. Erratum for May and Silhavy, “The Escherichia coli phospholipase PldA regulates outer membrane homeostasis via lipid signaling”. mBio 9, e00718-18 (2018).
Yao, Z., Kahne, D. & Kishony, R. Distinct single-cell morphological dynamics under beta-lactam antibiotics. Mol. Cell 48, 705–712 (2012).
Thomanek, N. et al. Intricate crosstalk between lipopolysaccharide, phospholipid and fatty acid metabolism in Escherichia coli modulates proteolysis of LpxC. Front. Microbiol. 9, 3285 (2018).
Bernadsky, G., Beveridge, T. J. & Clarke, A. J. Analysis of the sodium dodecyl sulfate-stable peptidoglycan autolysins of select gram-negative pathogens by using renaturing polyacrylamide gel electrophoresis. J. Bacteriol. 176, 5225–5232 (1994).
van Heijenoort, J. Peptidoglycan hydrolases of Escherichia coli. Microbiol. Mol. Biol. Rev. 75, 636–663 (2011).
Vollmer, W., Joris, B., Charlier, P. & Foster, S. Bacterial peptidoglycan (murein) hydrolases. FEMS Microbiol. Rev. 32, 259–286 (2008).
Busse, H. J., Wostmann, C. & Bakker, E. P. The bactericidal action of streptomycin: membrane permeabilization caused by the insertion of mistranslated proteins into the cytoplasmic membrane of Escherichia coli and subsequent caging of the antibiotic inside the cells due to degradation of these proteins. J. Gen. Microbiol. 138, 551–561 (1992).
Kohanski, M. A., Dwyer, D. J., Wierzbowski, J., Cottarel, G. & Collins, J. J. Mistranslation of membrane proteins and two-component system activation trigger antibiotic-mediated cell death. Cell 135, 679–690 (2008).
Akiyama, Y. Quality control of cytoplasmic membrane proteins in Escherichia coli. J. Biochem. 146, 449–454 (2009).
Moreno-Cinos, C. et al. ClpP protease, a promising antimicrobial target. Int. J. Mol. Sci. 20, 2232 (2019).
Brotz-Oesterhelt, H. et al. Dysregulation of bacterial proteolytic machinery by a new class of antibiotics. Nat. Med. 11, 1082–1087 (2005).
Nystrom, T. Not quite dead enough: on bacterial life, culturability, senescence, and death. Arch. Microbiol. 176, 159–164 (2001).
Ezraty, B., Gennaris, A., Barras, F. & Collet, J. F. Oxidative stress, protein damage and repair in bacteria. Nat. Rev. Microbiol. 15, 385–396 (2017).
Ganesan, A. K. & Smith, K. C. Requirement for protein synthesis in rec-dependent repair of deoxyribonucleic acid in Escherichia coli after ultraviolet or X irradiation. J. Bacteriol. 111, 575–585 (1972).
Drlica, K., Malik, M., Kerns, R. J. & Zhao, X. Quinolone-mediated bacterial death. Antimicrob. Agents Chemother. 52, 385–392 (2008).
Dwyer, D. J., Kohanski, M. A., Hayete, B. & Collins, J. J. Gyrase inhibitors induce an oxidative damage cellular death pathway in Escherichia coli. Mol. Syst. Biol. 3, 91 (2007).
Singleton, M. R., Dillingham, M. S., Gaudier, M., Kowalczykowski, S. C. & Wigley, D. B. Crystal structure of RecBCD enzyme reveals a machine for processing DNA breaks. Nature 432, 187–193 (2004).
Foti, J. J., Devadoss, B., Winkler, J. A., Collins, J. J. & Walker, G. C. Oxidation of the guanine nucleotide pool underlies cell death by bactericidal antibiotics. Science 336, 315–319 (2012).
Song, L. Y. et al. Exploring synergy between classic mutagens and antibiotics to examine mechanisms of synergy and antibiotic action. Antimicrob. Agents Chemother. 60, 1515–1520 (2015).
Ocampo, P. S. et al. Antagonism between bacteriostatic and bactericidal antibiotics is prevalent. Antimicrob. Agents Chemother. 58, 4573–4582 (2014).
Kouzminova, E. A. & Kuzminov, A. Chromosomal fragmentation in dUTPase-deficient mutants of Escherichia coli and its recombinational repair. Mol. Microbiol. 51, 1279–1295 (2004).
Le, L. A. T. et al. Nutritional conditions and oxygen concentration affect spontaneous occurrence of homologous recombination events but not spontaneous mutagenesis in Escherichia coli. Genes Genet. Syst. 95, 85–93 (2020).
Bayles, K. W. Bacterial programmed cell death: making sense of a paradox. Nat. Rev. Microbiol. 12, 63–69 (2014).
Li, G. W., Burkhardt, D., Gross, C. & Weissman, J. S. Quantifying absolute protein synthesis rates reveals principles underlying allocation of cellular resources. Cell 157, 624–635 (2014).
Quan, S., Skovgaard, O., McLaughlin, R. E., Buurman, E. T. & Squires, C. L. Markerless Escherichia coli rrn deletion strains for genetic determination of ribosomal binding sites. G3 5, 2555–2557 (2015).
Imlay, J. A., Chin, S. M. & Linn, S. Toxic D. N. A. damage by hydrogen peroxide through the Fenton reaction in vivo and in vitro. Science 240, 640–642 (1988).
Ezraty, B. et al. Fe-S cluster biosynthesis controls uptake of aminoglycosides in a ROS-less death pathway. Science 340, 1583–1587 (2013).
Liu, Y. & Imlay, J. A. Cell death from antibiotics without the involvement of reactive oxygen species. Science 339, 1210–1213 (2013).
Keren, I., Wu, Y., Inocencio, J., Mulcahy, L. R. & Lewis, K. Killing by bactericidal antibiotics does not depend on reactive oxygen species. Science 339, 1213–1216 (2013).
Dwyer, D. J. et al. Antibiotics induce redox-related physiological alterations as part of their lethality. Proc. Natl Acad. Sci. USA 111, E2100–E2109 (2014).
Dwyer, D. J., Collins, J. J. & Walker, G. C. Unraveling the physiological complexities of antibiotic lethality. Annu. Rev. Pharmacol. Toxicol. 55, 313–332 (2015).
Davis, B. D. Mechanism of bactericidal action of aminoglycosides. Microbiol. Rev. 51, 341–350 (1987).
Nakamura, Y., Ikeda, M., Nishigaki, R. & Umemura, K. Kinetics of bactericidal activity of aminoglycosides during dynamic dilution. J. Pharmacobiodyn. 8, 695–700 (1985).
Nagel, R. & Chan, A. Mistranslation and genetic variability: the effect of streptomycin. Mutat. Res. 601, 162–170 (2006).
Ying, L., Zhu, H., Shoji, S. & Fredrick, K. Roles of specific aminoglycoside-ribosome interactions in the inhibition of translation. RNA 25, 247–254 (2019).
Gonzalez-Zorn, B. et al. armA and aminoglycoside resistance in Escherichia coli. Emerg. Infect. Dis. 11, 954–956 (2005).
Haugan, M. S., Lobner-Olesen, A. & Frimodt-Moller, N. Comparative activity of ceftriaxone, ciprofloxacin, and gentamicin as a function of bacterial growth rate probed by escherichia coli chromosome replication in the mouse peritonitis model. Antimicrob. Agents Chemother. 63, e02133-18 (2019).
Taber, H. W., Mueller, J. P., Miller, P. F. & Arrow, A. S. Bacterial uptake of aminoglycoside antibiotics. Microbiol. Rev. 51, 439–457 (1987).
Ramirez, M. S. & Tolmasky, M. E. Aminoglycoside modifying enzymes. Drug Resist. Updat. 13, 151–171 (2010).
Peterson, A. A., Hancock, R. E. & McGroarty, E. J. Binding of polycationic antibiotics and polyamines to lipopolysaccharides of Pseudomonas aeruginosa. J. Bacteriol. 164, 1256–1261 (1985).
Kadurugamuwa, J. L., Clarke, A. J. & Beveridge, T. J. Surface action of gentamicin on Pseudomonas aeruginosa. J. Bacteriol. 175, 5798–5805 (1993).
Dubin, D. T., Hancock, R. & Davis, B. D. The sequence of some effects of streptomycin in Escherichia Coli. Biochim. Biophys. Acta 74, 476–489 (1963).
Ji, X. et al. Alarmone Ap4A is elevated by aminoglycoside antibiotics and enhances their bactericidal activity. Proc. Natl Acad. Sci. USA 116, 9578–9585 (2019).
Bryan, L. E. & Kwan, S. Roles of ribosomal binding, membrane potential, and electron transport in bacterial uptake of streptomycin and gentamicin. Antimicrob. Agents Chemother. 23, 835–845 (1983).
Hooper, D. C. Mechanisms of action of antimicrobials: focus on fluoroquinolones. Clin. Infect. Dis. 32, S9–S15 (2001).
Phillips, I., Culebras, E., Moreno, F. & Baquero, F. Induction of the SOS response by new 4-quinolones. J. Antimicrob. Chemother. 20, 631–638 (1987).
Mustaev, A. et al. Fluoroquinolone-gyrase-DNA complexes: two modes of drug binding. J. Biol. Chem. 289, 12300–12312 (2014).
Smirnova, G. V. & Oktyabrsky, O. N. Relationship between Escherichia coli growth rate and bacterial susceptibility to ciprofloxacin. FEMS Microbiol. Lett. 365 (2018).
Nakamura, Y. & Yura, T. Effects of rifampicin on synthesis and functional activity of DNA-dependent RNA polymerase in Escherichia coli. Mol. Gen. Genet. 145, 227–237 (1976).
Gumbo, T. et al. Concentration-dependent Mycobacterium tuberculosis killing and prevention of resistance by rifampin. Antimicrob. Agents Chemother. 51, 3781–3788 (2007).
Zhang, Z. et al. Could high-concentration rifampicin kill rifampicin-resistant M. tuberculosis? Rifampicin MIC test in rifampicin-resistant isolates from patients with osteoarticular tuberculosis. J. Orthop. Surg. Res. 9, 124 (2014).
Burmann, B. M. et al. A NusE:NusG complex links transcription and translation. Science 328, 501–504 (2010).
Proshkin, S., Rahmouni, A. R., Mironov, A. & Nudler, E. Cooperation between translating ribosomes and RNA polymerase in transcription elongation. Science 328, 504–508 (2010).
Amitai, S., Yassin, Y. & Engelberg-Kulka, H. MazF-mediated cell death in Escherichia coli: a point of no return. J. Bacteriol. 186, 8295–8300 (2004).
Amitai, S., Kolodkin-Gal, I., Hananya-Meltabashi, M., Sacher, A. & Engelberg-Kulka, H. Escherichia coli MazF leads to the simultaneous selective synthesis of both “death proteins” and “survival proteins”. PLoS Genet. 5, e1000390 (2009).
Saito, K. et al. Rifamycin action on RNA polymerase in antibiotic-tolerant Mycobacterium tuberculosis results in differentially detectable populations. Proc. Natl Acad. Sci. USA 114, E4832–E4840 (2017).
Kannan, K., Vazquez-Laslop, N. & Mankin, A. S. Selective protein synthesis by ribosomes with a drug-obstructed exit tunnel. Cell 151, 508–520 (2012).
Mosaei, H. & Zenkin, N. Inhibition of RNA polymerase by rifampicin and rifamycin-like molecules. EcoSal Plus https://doi.org/10.1128/ecosalplus.ESP-0017-2019 (2020).
Tipper, D. J. & Strominger, J. L. Mechanism of action of penicillins: a proposal based on their structural similarity to acyl-D-alanyl-D-alanine. Proc. Natl Acad. Sci. USA 54, 1133–1141 (1965).
Chung, H. S. et al. Rapid beta-lactam-induced lysis requires successful assembly of the cell division machinery. Proc. Natl Acad. Sci. USA 106, 21872–21877 (2009).
Lee, A. J. et al. Robust, linear correlations between growth rates and beta-lactam-mediated lysis rates. Proc. Natl Acad. Sci. USA 115, 4069–4074 (2018).
Tomasz, A. The mechanism of the irreversible antimicrobial effects of penicillins: how the beta-lactam antibiotics kill and lyse bacteria. Annu. Rev. Microbiol. 33, 113–137 (1979).
Cho, H., Uehara, T. & Bernhardt, T. G. Beta-lactam antibiotics induce a lethal malfunctioning of the bacterial cell wall synthesis machinery. Cell 159, 1300–1311 (2014).
Mercier, R., Kawai, Y. & Errington, J. Excess membrane synthesis drives a primitive mode of cell proliferation. Cell 152, 997–1007 (2013).
Koonin, E. V. & Mulkidjanian, A. Y. Evolution of cell division: from shear mechanics to complex molecular machineries. Cell 152, 942–944 (2013).
Booth, S. & Lewis, R. J. Structural basis for the coordination of cell division with the synthesis of the bacterial cell envelope. Protein Sci. 28, 2042–2054 (2019).
Minato, Y. et al. Mutual potentiation drives synergy between trimethoprim and sulfamethoxazole. Nat. Commun. 9, 1003 (2018).
Van Bambeke, F., Van Laethem, Y., Courvalin, P. & Tulkens, P. M. Glycopeptide antibiotics: from conventional molecules to new derivatives. Drugs 64, 913–936 (2004).
Joukhadar, C., Pillai, S., Wennersten, C., Moellering, R. C. Jr. & Eliopoulos, G. M. Lack of bactericidal antagonism or synergism in vitro between oxacillin and vancomycin against methicillin-susceptible strains of Staphylococcus aureus. Antimicrob. Agents Chemother. 54, 773–777 (2010).
Cui, L. et al. Novel mechanism of antibiotic resistance originating in vancomycin-intermediate Staphylococcus aureus. Antimicrob. Agents Chemother. 50, 428–438 (2006).
Larsson, A. J., Walker, K. J., Raddatz, J. K. & Rotschafer, J. C. The concentration-independent effect of monoexponential and biexponential decay in vancomycin concentrations on the killing of Staphylococcus aureus under aerobic and anaerobic conditions. J. Antimicrob. Chemother. 38, 589–597 (1996).
Ladjouzi, R. et al. Analysis of the tolerance of pathogenic enterococci and Staphylococcus aureus to cell wall active antibiotics. J. Antimicrob. Chemother. 68, 2083–2091 (2013).
Amyes, S. G. Bactericidal activity of trimethoprim alone and in combination with sulfamethoxazole on susceptible and resistant Escherichia coli K-12. Antimicrob. Agents Chemother. 21, 288–293 (1982).
Then, R. & Angehrn, P. Nature of the bacterial action of sulfonamides and trimethoprim, alone and in combination. J. Infect. Dis. 128, 498–501 (1973).
Ahmad, S. I., Kirk, S. H. & Eisenstark, A. Thymine metabolism and thymineless death in prokaryotes and eukaryotes. Annu. Rev. Microbiol. 52, 591–625 (1998).
Khan, S. R. & Kuzminov, A. Thymineless death in Escherichia coli is unaffected by chromosomal replication complexity. J. Bacteriol. 201, e00797-18 (2019).
Cambau, E. et al. Jacques F. Acar (1931–2020). Clin. Microbiol. Infect. 26, 1261–1263 (2020).
Acknowledgements
The authors are grateful to their awesome wives, Ros and Adriana, for putting up with them during this period of COVID-19 quarantine and supporting their playing fun games such as reviewing the literature and writing this Perspective. They thank I. McCall for a careful reading of this manuscript, and J. Rodríguez-Beltrán for discussion about some critical concepts. This research was funded by grants from the U.S. National Institutes of General Medical Science (GM091875-17 and 1R35 GM136407-01) to B.R.L and from the Regional Government of Madrid (InGeMICS- B2017/BMD-3691) and the Ramón Areces Foundation to the F.B. laboratory. The authors dedicate this Perspective to the memory of J. Acar137, with whom they would have loved to have discussed the question of how antibiotics kill; from those conversations with Jacques, the authors know they would have had much more to tell you about the answer.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Microbiology thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baquero, F., Levin, B.R. Proximate and ultimate causes of the bactericidal action of antibiotics. Nat Rev Microbiol 19, 123–132 (2021). https://doi.org/10.1038/s41579-020-00443-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41579-020-00443-1