Abstract
Background
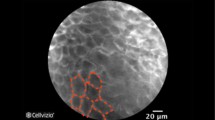
Confocal laser endomicroscopy (CLE) is a novel endoscopic adjunct that allows real-time in vivo histological examination of mucosal surfaces. By using intravenous or topical fluorescent agents, CLE highlights certain mucosal elements that facilitate an optical biopsy in real time. CLE technology has been used in different organ systems including the gastrointestinal tract. There has been numerous studies evaluating this technology in gastrointestinal endoscopy, our aim was to evaluate the safety, value, and efficacy of this technology in the gastrointestinal tract.
Methods
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Technology and Value Assessment Committee (TAVAC) performed a PubMed/Medline database search of clinical studies involving CLE in May of 2018. The literature search used combinations of the keywords: confocal laser endomicroscopy, pCLE, Cellvizio, in vivo microscopy, optical histology, advanced endoscopic imaging, and optical diagnosis. Bibliographies of key references were searched for relevant studies not covered by the PubMed search. Case reports and small case series were excluded. The manufacturer’s website was also used to identify key references. The United States Food and Drug Administration (U.S. FDA) Manufacturer And User facility and Device Experience (MAUDE) database was searched for reports regarding the device malfunction or injuries.
Results
The technology offers an excellent safety profile with rare adverse events related to the use of fluorescent agents. It has been shown to increase the detection of dysplastic Barrett’s esophagus, gastric intraepithelial neoplasia/early gastric cancer, and dysplasia associated with inflammatory bowel disease when compared to standard screening protocols. It also aids in the differentiation and classification of colorectal polyps, indeterminate biliary strictures, and pancreatic cystic lesions.
Conclusions
CLE has an excellent safety profile. CLE can increase the diagnostic accuracy in a number of gastrointestinal pathologies.


Similar content being viewed by others
References
Sakashita M, Inoue H, Kashida H, Tanaka J, Cho JY, Satodate H, Hidaka E, Yoshida T, Fukami N, Tamegai Y, Shiokawa A, Kudo S (2003) Virtual histology of colorectal lesions using laser-scanning confocal microscopy. Endoscopy 35:1033–1038. https://doi.org/10.1055/s-2003-44595
Goetz M, Watson A, Kiesslich R (2011) Confocal laser endomicroscopy in gastrointestinal diseases. J Biophoton 4:498–508. https://doi.org/10.1002/jbio.201100022
Wallace MB, Fockens P (2009) Probe-based confocal laser endomicroscopy. Gastroenterology 136:1509–1513. https://doi.org/10.1053/j.gastro.2009.03.034
Shahid MW, Crook JE, Meining A, Perchant A, Buchner A, Gomez V, Wallace MB (2011) Exploring the optimal fluorescein dose in probe-based confocal laser endomicroscopy for colonic imaging. J Interv Gastroenterol 1:166–171. https://doi.org/10.4161/jig.19953
Li Z, Zuo XL, Li CQ, Zhou CJ, Liu J, Goetz M, Kiesslich R, Wu KC, Fan DM, Li YQ (2013) In vivo molecular imaging of gastric cancer by targeting MG7 antigen with confocal laser endomicroscopy. Endoscopy 45:79–85. https://doi.org/10.1055/s-0032-1325762
Hsiung P-L, Hardy J, Friedland S, Soetikno R, Du CB, Wu AP, Sahbaie P, Crawford JM, Lowe AW, Contag CH, Wang TD (2008) Detection of colonic dysplasia in vivo using a targeted heptapeptide and confocal microendoscopy. Nat Med 14:454–458. https://doi.org/10.1038/nm1692
De Palma GD, Colavita I, Zambrano G, Giglio MC, Maione F, Luglio G, Sarnelli G, Rispo A, Schettino P, D’Armiento FP, De Palma FDE, D’Argenio V, Salvatore F (2017) Detection of colonic dysplasia in patients with ulcerative colitis using a targeted fluorescent peptide and confocal laser endomicroscopy: a pilot study. PLoS ONE 12:e0180509. https://doi.org/10.1371/journal.pone.0180509
Foersch S, Kiesslich R, Waldner MJ, Delaney P, Galle PR, Neurath MF, Goetz M (2010) Molecular imaging of VEGF in gastrointestinal cancer in vivo using confocal laser endomicroscopy. Gut 59:1046–1055. https://doi.org/10.1136/gut.2009.202986
Goetz M, Ziebart A, Foersch S, Vieth M, Waldner MJ, Delaney P, Galle PR, Neurath MF, Kiesslich R (2010) In vivo molecular imaging of colorectal cancer with confocal endomicroscopy by targeting epidermal growth factor receptor. Gastroenterology 138:435–446. https://doi.org/10.1053/j.gastro.2009.10.032
Sturm MB, Piraka C, Elmunzer BJ, Kwon RS, Joshi BP, Appelman HD, Turgeon DK, Wang TD (2013) In vivo molecular imaging of Barrett’s esophagus with confocal laser endomicroscopy. Gastroenterology 145:56–58. https://doi.org/10.1053/j.gastro.2013.05.008
Nakai Y, Isayama H, Shinoura S, Iwashita T, Samarasena JB, Chang KJ, Koike K (2014) Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 26(Suppl 1):86–94. https://doi.org/10.1111/den.12152
Bhutani MS, Koduru P, Joshi V, Karstensen JG, Saftoiu A, Vilmann P, Giovannini M (2015) EUS-guided needle-based confocal laser endomicroscopy: a novel technique with emerging applications. Gastroenterol Hepatol 11:235–240
Tsujino T, Yan-Lin Huang J, Nakai Y, Samarasena JB, Lee JG, Chang KJ (2015) In vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy. Best Pract Res Clin Gastroenterol 29:601–610. https://doi.org/10.1016/j.bpg.2015.06.006
Wallace M, Lauwers G, Chen Y, Dekker E, Fockens P, Sharma P, Meining A (2011) Miami classification for probe-based confocal laser endomicroscopy. Endoscopy 43:882–891. https://doi.org/10.1055/s-0030-1256632
Chene G, Chauvy L, Buenerd A, Moret S, Nadaud B, Chabert P, Lamblin G (2017) Dynamic real-time in vivo confocal laser endomicroscopy of the fallopian tube during laparoscopy in the prevention of ovarian cancer. Eur J Obstet Gynecol Reprod Biol 216:18–23. https://doi.org/10.1016/j.ejogrb.2017.07.002
Trindade JRM, Figueiredo VR, Pêgo-Fernandes PM, Terra RM (2019) Probe-based confocal laser endomicroscopy of the airways: physiological and pathological characteristics of preneoplastic and neoplastic lesions. J Bras Pneumol Publ Off Soc Bras Pneumol Tisil 45:e20180103. https://doi.org/10.1590/1806-3713/e20180103
Oetter N, Knipfer C, Rohde M, von Wilmowsky C, Maier A, Brunner K, Adler W, Neukam F-W, Neumann H, Stelzle F (2016) Development and validation of a classification and scoring system for the diagnosis of oral squamous cell carcinomas through confocal laser endomicroscopy. J Transl Med 14:159. https://doi.org/10.1186/s12967-016-0919-4
Wu K, Liu J-J, Adams W, Sonn GA, Mach KE, Pan Y, Beck AH, Jensen KC, Liao JC (2011) Dynamic real-time microscopy of the urinary tract using confocal laser endomicroscopy. Urology 78:225–231. https://doi.org/10.1016/j.urology.2011.02.057
Polglase AL, McLaren WJ, Skinner SA, Kiesslich R, Neurath MF, Delaney PM (2005) A fluorescence confocal endomicroscope for in vivo microscopy of the upper- and the lower-GI tract. Gastrointest Endosc 62:686–695. https://doi.org/10.1016/j.gie.2005.05.021
Kiesslich R, Goetz M, Neurath MF (2008) Confocal laser endomicroscopy for gastrointestinal diseases. Gastrointest Endosc Clin N Am 18:451–466, viii. https://doi.org/10.1016/j.giec.2008.03.002
Yoshida S, Tanaka S, Hirata M, Mouri R, Kaneko I, Oka S, Yoshihara M, Chayama K (2007) Optical biopsy of GI lesions by reflectance-type laser-scanning confocal microscopy. Gastrointest Endosc 66:144–149. https://doi.org/10.1016/j.gie.2006.10.054
Hur C, Miller M, Kong CY, Dowling EC, Nattinger KJ, Dunn M, Feuer EJ (2013) Trends in esophageal adenocarcinoma incidence and mortality. Cancer 119:1149–1158. https://doi.org/10.1002/cncr.27834
Attwood SE, Morris CD (2001) Who defines Barrett’s oesophagus: endoscopist or pathologist? Eur J Gastroenterol Hepatol 13:97–99
Montgomery E, Goldblum JR, Greenson JK, Haber MM, Lamps LW, Lauwers GY, Lazenby AJ, Lewin DN, Robert ME, Washington K, Zahurak ML, Hart J (2001) Dysplasia as a predictive marker for invasive carcinoma in Barrett esophagus: a follow-up study based on 138 cases from a diagnostic variability study. Hum Pathol 32:379–388. https://doi.org/10.1053/hupa.2001.23511
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66:683–691. https://doi.org/10.1136/gutjnl-2015-310912
Colorectal cancer—Cancer Stat facts. In: SEER. https://seer.cancer.gov/statfacts/html/colorect.html. Accessed 1 Feb 2019
Levin TR, Corley DA, Jensen CD, Schottinger JE, Quinn VP, Zauber AG, Lee JK, Zhao WK, Udaltsova N, Ghai NR, Lee AT, Quesenberry CP, Fireman BH, Doubeni CA (2018) Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology 155:1383–1391.e5. https://doi.org/10.1053/j.gastro.2018.07.017
Sillars-Hardebol AH, Carvalho B, van Engeland M, Fijneman RJA, Meijer GA (2012) The adenoma hunt in colorectal cancer screening: defining the target. J Pathol 226:1–6. https://doi.org/10.1002/path.3012
Shussman N, Wexner SD (2014) Colorectal polyps and polyposis syndromes. Gastroenterol Rep 2:1–15. https://doi.org/10.1093/gastro/got041
Gao Y-D, Qu Y-W, Liu H-F (2018) Comparison of diagnostic efficacy between CLE, tissue sampling, and CLE combined with tissue sampling for undetermined pancreaticobiliary strictures: a meta-analysis. Scand J Gastroenterol. https://doi.org/10.1080/00365521.2018.1448435
Storm AC, Lee LS (2016) Is seeing really believing? Probe-based confocal laser endomicroscopy in the evaluation of pancreaticobiliary disease. J Clin Gastroenterol 50:359–365. https://doi.org/10.1097/MCG.0000000000000505
Liu Y, Lu Y, Sun B, Zhang W-M, Zhang Z-Z, He Y-P, Yang X-J (2016) Probe-based confocal laser endomicroscopy for the diagnosis of undetermined biliary stenoses: a meta-analysis. Clin Res Hepatol Gastroenterol 40:666–673. https://doi.org/10.1016/j.clinre.2016.05.007
Ştefănescu D, Pereira SP, Keane M, Săftoiu A (2015) Needle-based confocal laser endomicroscopy in pancreatic cystic tumors assessment. Rom J Morphol Embryol Rev Roum Morphol Embryol 56:1263–1268
Shaheen NJ, Falk GW, Iyer PG, Gerson LB, American College of Gastroenterology (2016) ACG clinical guideline: diagnosis and management of Barrett’s esophagus. Am J Gastroenterol 111:30–50; quiz 51. https://doi.org/10.1038/ajg.2015.322
Abrams JA, Kapel RC, Lindberg GM, Saboorian MH, Genta RM, Neugut AI, Lightdale CJ (2009) Adherence to biopsy guidelines for Barrett’s esophagus surveillance in the community setting in the United States. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 7:736–742; quiz 710. https://doi.org/10.1016/j.cgh.2008.12.027
ASGE Technology Committee, Thosani N, Abu Dayyeh BK, Sharma P, Aslanian HR, Enestvedt BK, Komanduri S, Manfredi M, Navaneethan U, Maple JT, Pannala R, Parsi MA, Smith ZL, Sullivan SA, Banerjee S (2016) ASGE Technology Committee systematic review and meta-analysis assessing the ASGE Preservation and Incorporation of Valuable Endoscopic Innovations thresholds for adopting real-time imaging-assisted endoscopic targeted biopsy during endoscopic surveillance of Barrett’s esophagus. Gastrointest Endosc 83:684–698.e7. https://doi.org/10.1016/j.gie.2016.01.007
Kiesslich R, Gossner L, Goetz M, Dahlmann A, Vieth M, Stolte M, Hoffman A, Jung M, Nafe B, Galle PR, Neurath MF (2006) In vivo histology of Barrett’s esophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 4:979–987. https://doi.org/10.1016/j.cgh.2006.05.010
Wu J, Pan Y-M, Wang T-T, Hu B (2014) Confocal laser endomicroscopy for detection of neoplasia in Barrett’s esophagus: a meta-analysis. Dis Esophagus Off J Int Soc Dis Esophagus 27:248–254. https://doi.org/10.1111/dote.12085
Shah T, Lippman R, Kohli D, Mutha P, Solomon S, Zfass A (2018) Accuracy of probe-based confocal laser endomicroscopy (pCLE) compared to random biopsies during endoscopic surveillance of Barrett’s esophagus. Endosc Int Open 6:E414–E420. https://doi.org/10.1055/s-0043-124868
Li W-B, Zuo X-L, Li C-Q, Zuo F, Gu X-M, Yu T, Chu C-L, Zhang T-G, Li Y-Q (2011) Diagnostic value of confocal laser endomicroscopy for gastric superficial cancerous lesions. Gut 60:299–306. https://doi.org/10.1136/gut.2010.223586
Jeon SR, Cho WY, Jin SY, Cheon YK, Choi SR, Cho JY (2011) Optical biopsies by confocal endomicroscopy prevent additive endoscopic biopsies before endoscopic submucosal dissection in gastric epithelial neoplasias: a prospective, comparative study. Gastrointest Endosc 74:772–780. https://doi.org/10.1016/j.gie.2011.05.005
Bok GH, Jeon SR, Cho JY, Cho J-H, Lee WC, Jin SY, Choi IH, Kim HG, Lee TH, Park EJ (2013) The accuracy of probe-based confocal endomicroscopy versus conventional endoscopic biopsies for the diagnosis of superficial gastric neoplasia (with videos). Gastrointest Endosc 77:899–908. https://doi.org/10.1016/j.gie.2013.01.018
Li Z, Zuo X-L, Yu T, Gu X-M, Zhou C-J, Li C-Q, Ji R, Li Y-Q (2014) Confocal laser endomicroscopy for in vivo detection of gastric intestinal metaplasia: a randomized controlled trial. Endoscopy 46:282–290. https://doi.org/10.1055/s-0033-1359215
Lim LG, Yeoh KG, Srivastava S, Chan YH, Teh M, Ho KY (2013) Comparison of probe-based confocal endomicroscopy with virtual chromoendoscopy and white-light endoscopy for diagnosis of gastric intestinal metaplasia. Surg Endosc 27:4649–4655. https://doi.org/10.1007/s00464-013-3098-x
Horiguchi N, Tahara T, Yamada H, Yoshida D, Okubo M, Nagasaka M, Nakagawa Y, Shibata T, Tsukamoto T, Kuroda M, Ohmiya N (2018) In vivo diagnosis of early-stage gastric cancer found after Helicobacter pylori eradication using probe-based confocal laser endomicroscopy. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 30:219–227. https://doi.org/10.1111/den.12926
Guo Y-T, Li Y-Q, Yu T, Zhang T-G, Zhang J-N, Liu H, Liu F-G, Xie X-J, Zhu Q, Zhao Y-A (2008) Diagnosis of gastric intestinal metaplasia with confocal laser endomicroscopy in vivo: a prospective study. Endoscopy 40:547–553
Kitabatake S, Niwa Y, Miyahara R, Ohashi A, Matsuura T, Iguchi Y, Shimoyama Y, Nagasaka T, Maeda O, Ando T, Ohmiya N, Itoh A, Hirooka Y, Goto H (2006) Confocal endomicroscopy for the diagnosis of gastric cancer in vivo. Endoscopy 38:1110–1114. https://doi.org/10.1055/s-2006-944855
Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA, American College of Gastroenterology (2013) ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 108:656–676; quiz 677. https://doi.org/10.1038/ajg.2013.79
He X, Wu K, Ogino S, Giovannucci EL, Chan AT, Song M (2018) Association between risk factors for colorectal cancer and risk of serrated polyps and conventional adenomas. Gastroenterology 155:355–373.e18. https://doi.org/10.1053/j.gastro.2018.04.019
Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ (2017) Colorectal cancer screening: recommendations for physicians and patients from the U.S. Multi-society Task Force on Colorectal Cancer. Gastroenterology 153:307–323. https://doi.org/10.1053/j.gastro.2017.05.013
Carballal S, Maisterra S, López-Serrano A, Gimeno-García AZ, Vera MI, Marín-Garbriel JC, Díaz-Tasende J, Márquez L, Álvarez MA, Hernández L, De Castro L, Gordillo J, Puig I, Vega P, Bustamante-Balén M, Acevedo J, Peñas B, López-Cerón M, Ricart E, Cuatrecasas M, Jimeno M, Pellisé M, EndoCAR group of the Spanish Gastroenterological Association and Spanish Digestive Endoscopy Society (2018) Real-life chromoendoscopy for neoplasia detection and characterisation in long-standing IBD. Gut 67:70–78. https://doi.org/10.1136/gutjnl-2016-312332
Brugge WR, Lewandrowski K, Lee-Lewandrowski E, Centeno BA, Szydlo T, Regan S, del Castillo CF, Warshaw AL (2004) Diagnosis of pancreatic cystic neoplasms: a Report of the Cooperative Pancreatic Cyst Study. Gastroenterology 126:1330–1336
de Jong K, Poley J-W, van Hooft JE, Visser M, Bruno MJ, Fockens P (2011) Endoscopic ultrasound-guided fine-needle aspiration of pancreatic cystic lesions provides inadequate material for cytology and laboratory analysis: initial results from a prospective study. Endoscopy 43:585–590. https://doi.org/10.1055/s-0030-1256440
Sharma P, Brill J, Canto M, DeMarco D, Fennerty B, Gupta N, Laine L, Lieberman D, Lightdale C, Montgomery E, Odze R, Tokar J, Kochman M (2015) White Paper AGA: Advanced Imaging in Barrett’s Esophagus. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 13:2209–2218. https://doi.org/10.1016/j.cgh.2015.09.017
Vennalaganti PR, Kaul V, Wang KK, Falk GW, Shaheen NJ, Infantolino A, Johnson DA, Eisen G, Gerson LB, Smith MS, Iyer PG, Lightdale CJ, Schnoll-Sussman F, Gupta N, Gross SA, Abrams J, Haber GB, Chuttani R, Pleskow DK, Kothari S, Goldblum JR, Zhang Y, Sharma P (2018) Increased detection of Barrett’s esophagus-associated neoplasia using wide-area trans-epithelial sampling: a multicenter, prospective, randomized trial. Gastrointest Endosc 87:348–355. https://doi.org/10.1016/j.gie.2017.07.039
Wallace MB, Meining A, Canto MI, Fockens P, Miehlke S, Roesch T, Lightdale CJ, Pohl H, Carr-Locke D, Löhr M, Coron E, Filoche B, Giovannini M, Moreau J, Schmidt C, Kiesslich R (2010) The safety of intravenous fluorescein for confocal laser endomicroscopy in the gastrointestinal tract. Aliment Pharmacol Ther 31:548–552. https://doi.org/10.1111/j.1365-2036.2009.04207.x
MAUDE: Manufacturer and User Facility Device Experience. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/search.cfm. Accessed 26 Jan 2019
Nakai Y, Iwashita T, Park DH, Samarasena JB, Lee JG, Chang KJ (2015) Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc 81:1204–1214. https://doi.org/10.1016/j.gie.2014.10.025
Konda VJ, Meining A, Jamil LH, Giovannini M, Chang KJ, Hwang JH, Wallace MB, Siddiqui UD, Aslanian HR, Lo SK, Saunders MD, Hart J, Waxman I (2012) Mo1204 an international, multi-center trial on needle-based confocal laser endomicroscopy (nCLE): results from the In Vivo CLE Study in the Pancreas With Endosonography of Cystic Tumors (INSPECT). Gastroenterology 142:S-620. https://doi.org/10.1016/S0016-5085(12)62384-1
Huang JY, Samarasena JB, Nakai Y, Iwashita T, Chang KC (2014) Complication rates of combined endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) with needle-based confocal laser-induced endomicroscopy (nCLE) and through-the-needle (TTN) cystoscopy in pancreatic cysts. Am J Gastroenterol 109:S100
Richardson C, Colavita P, Dunst C, Bagnato J, Billing P, Birkenhagen K, Buckley F, Buitrago W, Burnette J, Leggett P, McCollister H, Stewart K, Wang T, Zfass A, Severson P (2018) Real-time diagnosis of Barrett’s esophagus: a prospective, multicenter study comparing confocal laser endomicroscopy with conventional histology for the identification of intestinal metaplasia in new users. Surg Endosc. https://doi.org/10.1007/s00464-018-6420-9
Caillol F, Godat S, Poizat F, Auttret A, Pesenti C, Bories E, Ratone JP, Giovannini M (2017) Probe confocal laser endomicroscopy in the therapeutic endoscopic management of Barrett’s dysplasia. Ann Gastroenterol 30:295–301. https://doi.org/10.20524/aog.2017.0138
Dunbar KB, Okolo P, Montgomery E, Canto MI (2009) Confocal laser endomicroscopy in Barrett’s esophagus and endoscopically in apparent Barrett’s neoplasia: a prospective, randomized, double-blind, controlled, crossover trial. Gastrointest Endosc 70:645–654. https://doi.org/10.1016/j.gie.2009.02.009
Canto MI, Anandasabapathy S, Brugge W, Falk GW, Dunbar KB, Zhang Z, Woods K, Almario JA, Schell U, Goldblum J, Maitra A, Montgomery E, Kiesslich R, Confocal Endomicroscopy for Barrett’s Esophagus or Confocal Endomicroscopy for Barrett’s Esophagus (CEBE) Trial Group (2014) In vivo endomicroscopy improves detection of Barrett’s esophagus-related neoplasia: a multicenter international randomized controlled trial (with video). Gastrointest Endosc 79:211–221. https://doi.org/10.1016/j.gie.2013.09.020
Sharma P, Meining AR, Coron E, Lightdale CJ, Wolfsen HC, Bansal A, Bajbouj M, Galmiche J-P, Abrams JA, Rastogi A, Gupta N, Michalek JE, Lauwers GY, Wallace MB (2011) Real-time increased detection of neoplastic tissue in Barrett’s esophagus with probe-based confocal laser endomicroscopy: final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest Endosc 74:465–472. https://doi.org/10.1016/j.gie.2011.04.004
Xiong Y-Q, Ma S-J, Zhou J-H, Zhong X-S, Chen Q (2016) A meta-analysis of confocal laser endomicroscopy for the detection of neoplasia in patients with Barrett’s esophagus. J Gastroenterol Hepatol 31:1102–1110. https://doi.org/10.1111/jgh.13267
Gaddam S, Mathur SC, Singh M, Arora J, Wani SB, Gupta N, Overhiser A, Rastogi A, Singh V, Desai N, Hall SB, Bansal A, Sharma P (2011) Novel probe-based confocal laser endomicroscopy criteria and interobserver agreement for the detection of dysplasia in Barrett’s esophagus. Am J Gastroenterol 106:1961–1969. https://doi.org/10.1038/ajg.2011.294
Trovato C, Sonzogni A, Ravizza D, Fiori G, Tamayo D, De Roberto G, de Leone A, De Lisi S, Crosta C (2013) Confocal laser endomicroscopy for in vivo diagnosis of Barrett’s oesophagus and associated neoplasia: a pilot study conducted in a single Italian centre. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver 45:396–402. https://doi.org/10.1016/j.dld.2012.12.016
Jayasekera C, Taylor ACF, Desmond PV, Macrae F, Williams R (2012) Added value of narrow band imaging and confocal laser endomicroscopy in detecting Barrett’s esophagus neoplasia. Endoscopy 44:1089–1095. https://doi.org/10.1055/s-0032-1325734
Bertani H, Frazzoni M, Dabizzi E, Pigò F, Losi L, Manno M, Manta R, Bassotti G, Conigliaro R (2013) Improved detection of incident dysplasia by probe-based confocal laser endomicroscopy in a Barrett’s esophagus surveillance program. Dig Dis Sci 58:188–193. https://doi.org/10.1007/s10620-012-2332-z
Bajbouj M, Vieth M, Rösch T, Miehlke S, Becker V, Anders M, Pohl H, Madisch A, Schuster T, Schmid RM, Meining A (2010) Probe-based confocal laser endomicroscopy compared with standard four-quadrant biopsy for evaluation of neoplasia in Barrett’s esophagus. Endoscopy 42:435–440. https://doi.org/10.1055/s-0029-1244194
Wallace MB, Sharma P, Lightdale C, Wolfsen H, Coron E, Buchner A, Bajbouj M, Bansal A, Rastogi A, Abrams J, Crook JE, Meining A (2010) Preliminary accuracy and interobserver agreement for the detection of intraepithelial neoplasia in Barrett’s esophagus with probe-based confocal laser endomicroscopy. Gastrointest Endosc 72:19–24. https://doi.org/10.1016/j.gie.2010.01.053
Gong S, Xue H-B, Ge Z-Z, Dai J, Li X-B, Zhao Y-J, Zhang Y, Gao Y-J, Song Y (2015) Value of magnifying endoscopy with narrow-band imaging and confocal laser endomicroscopy in detecting gastric cancerous lesions. Medicine (Baltim) 94:e1930s. https://doi.org/10.1097/MD.0000000000001930
Li Z, Yu T, Zuo X-L, Gu X-M, Zhou C-J, Ji R, Li C-Q, Wang P, Zhang T-G, Ho K-Y, Li Y-Q (2010) Confocal laser endomicroscopy for in vivo diagnosis of gastric intraepithelial neoplasia: a feasibility study. Gastrointest Endosc 72:1146–1153. https://doi.org/10.1016/j.gie.2010.08.031
Bai T, Zhang L, Sharma S, Jiang YD, Xia J, Wang H, Qian W, Song J, Hou XH (2017) Diagnostic performance of confocal laser endomicroscopy for atrophy and gastric intestinal metaplasia: a meta-analysis. J Dig Dis 18:273–282. https://doi.org/10.1111/1751-2980.12470
Buchner AM, Shahid MW, Heckman MG, Krishna M, Ghabril M, Hasan M, Crook JE, Gomez V, Raimondo M, Woodward T, Wolfsen HC, Wallace MB (2010) Comparison of probe-based confocal laser endomicroscopy with virtual chromoendoscopy for classification of colon polyps. Gastroenterology 138:834–842. https://doi.org/10.1053/j.gastro.2009.10.053
Shahid MW, Buchner AM, Heckman MG, Krishna M, Raimondo M, Woodward T, Wallace MB (2012) Diagnostic accuracy of probe-based confocal laser endomicroscopy and narrow band imaging for small colorectal polyps: a feasibility study. Am J Gastroenterol 107:231–239. https://doi.org/10.1038/ajg.2011.376
Vennelaganti S, Vennalaganti P, Mathur S, Singh S, Jamal M, Kanakadandi V, Rai T, Hall M, Gupta N, Nutalapati V, Alsop B, Hornung B, Sharma P (2017) Validation of probe-based confocal laser endomicroscopy (pCLE) criteria for diagnosing colon polyp histology. J Clin Gastroenterol. https://doi.org/10.1097/MCG.0000000000000927
Belderbos TDG, van Oijen MGH, Moons LMG, Siersema PD (2017) Implementation of real-time probe-based confocal laser endomicroscopy (pCLE) for differentiation of colorectal polyps during routine colonoscopy. Endosc Int Open 5:E1104–E1110. https://doi.org/10.1055/s-0043-117948
André B, Vercauteren T, Buchner AM, Krishna M, Ayache N, Wallace MB (2012) Software for automated classification of probe-based confocal laser endomicroscopy videos of colorectal polyps. World J Gastroenterol 18:5560–5569. https://doi.org/10.3748/wjg.v18.i39.5560
Shahid MW, Buchner AM, Raimondo M, Woodward TA, Krishna M, Wallace MB (2012) Accuracy of real-time vs. blinded offline diagnosis of neoplastic colorectal polyps using probe-based confocal laser endomicroscopy: a pilot study. Endoscopy 44:343–348. https://doi.org/10.1055/s-0031-1291589
De Palma GD, Staibano S, Siciliano S, Persico M, Masone S, Maione F, Siano M, Mascolo M, Esposito D, Salvatori F, Persico G (2010) In vivo characterisation of superficial colorectal neoplastic lesions with high-resolution probe-based confocal laser endomicroscopy in combination with video-mosaicing: a feasibility study to enhance routine endoscopy. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver 42:791–797. https://doi.org/10.1016/j.dld.2010.03.009
Hurlstone DP, Baraza W, Brown S, Thomson M, Tiffin N, Cross SS (2008) In vivo real-time confocal laser scanning endomicroscopic colonoscopy for the detection and characterization of colorectal neoplasia. Br J Surg 95:636–645. https://doi.org/10.1002/bjs.5988
Rasmussen DN, Karstensen JG, Riis LB, Brynskov J, Vilmann P (2015) Confocal laser endomicroscopy in inflammatory bowel disease—a systematic review. J Crohns Colitis 9:1152–1159. https://doi.org/10.1093/ecco-jcc/jjv131
Lord R, Burr NE, Mohammed N, Subramanian V (2018) Colonic lesion characterization in inflammatory bowel disease: A systematic review and meta-analysis. World J Gastroenterol 24:1167–1180. https://doi.org/10.3748/wjg.v24.i10.1167
Hundorfean G, Chiriac MT, Mihai S, Hartmann A, Mudter J, Neurath MF (2017) Development and validation of a confocal laser endomicroscopy-based score for in vivo assessment of mucosal healing in ulcerative colitis patients. Inflamm Bowel Dis 24:35–44. https://doi.org/10.1093/ibd/izx012
Tontini GE, Mudter J, Vieth M, Günther C, Milani V, Atreya R, Rath T, Nägel A, Hatem G, Sturniolo GC, Vecchi M, Neurath MF, Galle PR, Buda A, Neumann H (2017) Prediction of clinical outcomes in Crohn’s disease by using confocal laser endomicroscopy: results from a prospective multicenter study. Gastrointest Endosc. https://doi.org/10.1016/j.gie.2017.10.033
Ohmiya N, Horiguchi N, Tahara T, Nagasaka M, Nakagawa Y, Shibata T, Tsukamoto T, Kuroda M (2017) In vivo characterization of abnormalities in small-bowel diseases using probe-based confocal laser endomicroscopy. Endosc Int Open 5:E547–E558. https://doi.org/10.1055/s-0043-106184
Meining A, Chen YK, Pleskow D, Stevens P, Shah RJ, Chuttani R, Michalek J, Slivka A (2011) Direct visualization of indeterminate pancreaticobiliary strictures with probe-based confocal laser endomicroscopy: a multicenter experience. Gastrointest Endosc 74:961–968. https://doi.org/10.1016/j.gie.2011.05.009
Giovannini M, Bories E, Monges G, Pesenti C, Caillol F, Delpero JR (2011) Results of a phase I-II study on intraductal confocal microscopy (IDCM) in patients with common bile duct (CBD) stenosis. Surg Endosc 25:2247–2253. https://doi.org/10.1007/s00464-010-1542-8
Löhr J-M, Lönnebro R, Stigliano S, Haas SL, Swahn F, Enochsson L, Noel R, Segersvärd R, Del Chiaro M, Verbeke CS, Arnelo U (2015) Outcome of probe-based confocal laser endomicroscopy (pCLE) during endoscopic retrograde cholangiopancreatography: a single-center prospective study in 45 patients. United Eur Gastroenterol J 3:551–560. https://doi.org/10.1177/2050640615579806
Slivka A, Gan I, Jamidar P, Costamagna G, Cesaro P, Giovannini M, Caillol F, Kahaleh M (2015) Validation of the diagnostic accuracy of probe-based confocal laser endomicroscopy for the characterization of indeterminate biliary strictures: results of a prospective multicenter international study. Gastrointest Endosc 81:282–290. https://doi.org/10.1016/j.gie.2014.10.009
Yang JF, Sharaiha RZ, Francis G, Karia K, Kistler CA, Laique SN, Hasan R, Gaidhane M, Tyberg A, Kahaleh M, Kowalski TE, Loren DE, Siddiqui A (2016) Diagnostic accuracy of directed cholangioscopic biopsies and confocal laser endomicroscopy in cytology-negative indeterminate bile duct stricture: a multicenter comparison trial. Minerva Gastroenterol Dietol 62:227–233
Meining A, Shah RJ, Slivka A, Pleskow D, Chuttani R, Stevens PD, Becker V, Chen YK (2012) Classification of probe-based confocal laser endomicroscopy findings in pancreaticobiliary strictures. Endoscopy 44:251–257. https://doi.org/10.1055/s-0031-1291545
Talreja JP, Turner BG, Gress FG, Ho S, Sarkaria S, Paddu N, Natov N, Bharmal S, Gaidhane M, Sethi A, Kahaleh M (2014) Pre- and post-training session evaluation for interobserver agreement and diagnostic accuracy of probe-based confocal laser endomicroscopy for biliary strictures. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 26:577–580. https://doi.org/10.1111/den.12214
Caillol F, Filoche B, Gaidhane M, Kahaleh M (2013) Refined probe-based confocal laser endomicroscopy classification for biliary strictures: the Paris Classification. Dig Dis Sci 58:1784–1789. https://doi.org/10.1007/s10620-012-2533-5
Taunk P, Singh S, Lichtenstein D, Joshi V, Gold J, Sharma A (2017) Improved classification of indeterminate biliary strictures by probe-based confocal laser endomicroscopy using the Paris Criteria following biliary stenting. J Gastroenterol Hepatol 32:1778–1783. https://doi.org/10.1111/jgh.13782
Heif M, Yen RD, Shah RJ (2013) ERCP with probe-based confocal laser endomicroscopy for the evaluation of dominant biliary stenoses in primary sclerosing cholangitis patients. Dig Dis Sci 58:2068–2074. https://doi.org/10.1007/s10620-013-2608-y
Konda VJA, Meining A, Jamil LH, Giovannini M, Hwang JH, Wallace MB, Chang KJ, Siddiqui UD, Hart J, Lo SK, Saunders MD, Aslanian HR, Wroblewski K, Waxman I (2013) A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy 45:1006–1013. https://doi.org/10.1055/s-0033-1344714
Napoléon B, Lemaistre A-I, Pujol B, Caillol F, Lucidarme D, Bourdariat R, Morellon-Mialhe B, Fumex F, Lefort C, Lepilliez V, Palazzo L, Monges G, Filoche B, Giovannini M (2015) A novel approach to the diagnosis of pancreatic serous cystadenoma: needle-based confocal laser endomicroscopy. Endoscopy 47:26–32. https://doi.org/10.1055/s-0034-1390693
Krishna SG, Swanson B, Hart PA, El-Dika S, Walker JP, McCarthy ST, Malli A, Shah ZK, Conwell DL (2016) Validation of diagnostic characteristics of needle based confocal laser endomicroscopy in differentiation of pancreatic cystic lesions. Endosc Int Open 4:E1124–E1135. https://doi.org/10.1055/s-0042-116491
Krishna SG, Brugge WR, Dewitt JM, Kongkam P, Napoleon B, Robles-Medranda C, Tan D, El-Dika S, McCarthy S, Walker J, Dillhoff ME, Manilchuk A, Schmidt C, Swanson B, Shah ZK, Hart PA, Conwell DL (2017) Needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cystic lesions: an international external interobserver and intraobserver study (with videos). Gastrointest Endosc 86:644–654.e2. https://doi.org/10.1016/j.gie.2017.03.002
Karstensen JG, Cârţână T, Constantinescu C, Dumitrașcu S, Kovacevic B, Klausen P, Hassan H, Klausen TW, Bertani H, Bhutani MS, Săftoiu A, Vilmann P (2018) Endoscopic ultrasound guided needle-based confocal laser endomicroscopy in solid pancreatic masses—a prospective validation study. Endosc Int Open 6:E78–E85. https://doi.org/10.1055/s-0043-121987
Kiesslich R, Goetz M, Lammersdorf K, Schneider C, Burg J, Stolte M, Vieth M, Nafe B, Galle PR, Neurath MF (2007) Chromoscopy-guided endomicroscopy increases the diagnostic yield of intraepithelial neoplasia in ulcerative colitis. Gastroenterology 132:874–882. https://doi.org/10.1053/j.gastro.2007.01.048
Buchner AM, Gomez V, Heckman MG, Shahid MW, Achem S, Gill KR, Jamil LH, Laith J, Kahaleh M, Lo SK, Picco M, Riegert-Johnson D, Raimondo M, Sciemeca D, Wolfsen H, Woodward T, Wallace MB (2011) The learning curve of in vivo probe-based confocal laser endomicroscopy for prediction of colorectal neoplasia. Gastrointest Endosc 73:556–560. https://doi.org/10.1016/j.gie.2011.01.002
Kuiper T, Kiesslich R, Ponsioen C, Fockens P, Dekker E (2012) The learning curve, accuracy, and interobserver agreement of endoscope-based confocal laser endomicroscopy for the differentiation of colorectal lesions. Gastrointest Endosc 75:1211–1217. https://doi.org/10.1016/j.gie.2012.01.040
Acknowledgements
The authors would like to thank Dr. Richard Satava and Dr. Peter Denk (SAGES Technology and Value Assessment Committee); Dr. Eric Pauli, Dr. Ryan Juza and Dr. Tripp Buckley (SAGES Flexible Endoscopy Committee) and Dr. Leena Khaitan and Dr. Yadnik Pandya (SAGES Foregut Task Force) for their help in coordinating this review and providing valuable feedback and guidance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Mazen R. Al-Mansour: Education Honoraria and general payments from Intuitive Surgical, Inc. Antonio Caycedo-Marulanda: Teaching Honoraria from ConMed, Inc., Medtronic, Inc., and Applied Medical, Inc. Brian R. Davis: Teaching Honoraria for Intuitive Surgical, Inc.; general payments from Endogastric Solutions and Mallinckrodt. Abdulrahim Alawashez: no disclosures. Salvatore Docimo: consulting and general payments from Boston Scientific, Inc. Corporation, W. L. Gore and Associates, Inc., Gore, Intuitive Surgical, Inc. Alia Qureshi: general payments from Intuitive Surgical, Inc. and Ethicon Endosurgical. Shawn Tsuda: Consulting, Education Honoraria, research support, and general payments from Allergan, Inc., Intuitive Surgical, Inc., Endo Pharmaceuticals, Inc., and Covidien LP.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Al-Mansour, M.R., Caycedo-Marulanda, A., Davis, B.R. et al. SAGES TAVAC safety and efficacy analysis confocal laser endomicroscopy. Surg Endosc 35, 2091–2103 (2021). https://doi.org/10.1007/s00464-020-07607-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07607-3