Abstract
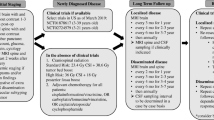
Pediatric brain tumors are the leading cause of childhood cancer mortality with medulloblastoma (MB) representing the most frequent malignant tumor. Although standardization of therapy resulted in a 2-fold reduction in mortality in patients with MB by 2002, it became clear that further improvements in clinical outcome would require a deeper understanding of the biology of MB. Employing the four main molecular MB subgroups (Wnt, Shh, Group 3 and Group 4), a restratification into clinicogenomic risk categories quantified an unacceptable survival for the high-risk group, urging researchers to focus their efforts towards acquiring a greater biological understanding of these children. Advancing in parallel with the molecular characterization and understanding of pediatric MB is the clinicogenomic correlations giving rise to recommendations for neurosurgical care. While unique observations that distinct radiological patterns can be identified to inform the MB molecular subgroup preoperatively, current neurosurgical practice remains maximal safe surgical resection followed by risk-adapted provision of adjuvant therapy in the context of a clinical trial.


Similar content being viewed by others
References
Ellison, D. W., et al. (2011). Medulloblastoma: clinicopathological correlates of SHH, WNT, and non-SHH/WNT molecular subgroups. Acta Neuropathologica, 121(3), 381–396.
Bailey, P., Cushings H. (1925). Medulloblastoma cerebelli:a common type of midcerebellar glioma of childhood. Archives of Neurology and Psychiatry, 14, 192–224.
Polkinghorn, W. R., & Tarbell, N. J. (2007). Medulloblastoma: tumorigenesis, current clinical paradigm, and efforts to improve risk stratification. Nature Clinical Practice. Oncology, 4(5), 295–304.
Ellison, D. (2002). Classifying the medulloblastoma: insights from morphology and molecular genetics. Neuropathology and Applied Neurobiology, 28(4), 257–282.
Packer, R. J. (2007). Craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. Current Neurology and Neuroscience Reports, 7(2), 130–132.
Packer, R. J., Sutton, L. N., Atkins, T. E., Radcliffe, J., Bunin, G. R., D’Angio, G., Siegel, K. R., & Schut, L. (1989). A prospective study of cognitive function in children receiving whole-brain radiotherapy and chemotherapy: 2-year results. Journal of Neurosurgery, 70(5), 707–713.
Bull, K. S., et al. (2014). Child-related characteristics predicting subsequent health-related quality of life in 8- to 14-year-old children with and without cerebellar tumors: a prospective longitudinal study. Neurooncol Pract, 1(3), 114–122.
Ellison, D. W. (2010). Childhood medulloblastoma: novel approaches to the classification of a heterogeneous disease. Acta Neuropathologica, 120(3), 305–316.
Ris, M. D., Packer, R., Goldwein, J., Jones-Wallace, D., & Boyett, J. M. (2001). Intellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: a Children’s Cancer Group study. Journal of Clinical Oncology, 19(15), 3470–3476.
Palmer, S. L., et al. (2003). Predicting intellectual outcome among children treated with 35-40 Gy craniospinal irradiation for medulloblastoma. Neuropsychology, 17(4), 548–555.
Palmer, S. L., et al. (2001). Patterns of intellectual development among survivors of pediatric medulloblastoma: a longitudinal analysis. Journal of Clinical Oncology, 19(8), 2302–2308.
Mulhern, R. K., Merchant, T. E., Gajjar, A., Reddick, W. E., & Kun, L. E. (2004). Late neurocognitive sequelae in survivors of brain tumours in childhood. The Lancet Oncology, 5(7), 399–408.
Yoo, H. J., Kim, H., Park, H. J., Kim, D. S., Ra, Y. S., & Shin, H. Y. (2016). Neurocognitive function and health-related quality of life in pediatric Korean survivors of medulloblastoma. Journal of Korean Medical Science, 31(11), 1726–1734.
Golub, T. R., et al. (1999). Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Science, 286(5439), 531–537.
Pomeroy, S. L., et al. (2002). Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature, 415(6870), 436–442.
Thompson, M. C., Fuller, C., Hogg, T. L., Dalton, J., Finkelstein, D., Lau, C. C., Chintagumpala, M., Adesina, A., Ashley, D. M., Kellie, S. J., Taylor, M. D., Curran, T., Gajjar, A., & Gilbertson, R. J. (2006). Genomics identifies medulloblastoma subgroups that are enriched for specific genetic alterations. Journal of Clinical Oncology, 24(12), 1924–1931.
Kool, M., Koster, J., Bunt, J., Hasselt, N. E., Lakeman, A., van Sluis, P., Troost, D., Meeteren, N. S., Caron, H. N., Cloos, J., Mrsić, A., Ylstra, B., Grajkowska, W., Hartmann, W., Pietsch, T., Ellison, D., Clifford, S. C., & Versteeg, R. (2008). Integrated genomics identifies five medulloblastoma subtypes with distinct genetic profiles, pathway signatures and clinicopathological features. PLoS One, 3(8), e3088.
Northcott, P. A., Korshunov, A., Witt, H., Hielscher, T., Eberhart, C. G., Mack, S., Bouffet, E., Clifford, S. C., Hawkins, C. E., French, P., Rutka, J. T., Pfister, S., & Taylor, M. D. (2011). Medulloblastoma comprises four distinct molecular variants. Journal of Clinical Oncology, 29(11), 1408–1414.
Cho, Y. J., Tsherniak, A., Tamayo, P., Santagata, S., Ligon, A., Greulich, H., Berhoukim, R., Amani, V., Goumnerova, L., Eberhart, C. G., Lau, C. C., Olson, J. M., Gilbertson, R. J., Gajjar, A., Delattre, O., Kool, M., Ligon, K., Meyerson, M., Mesirov, J. P., & Pomeroy, S. L. (2011). Integrative genomic analysis of medulloblastoma identifies a molecular subgroup that drives poor clinical outcome. Journal of Clinical Oncology, 29(11), 1424–1430.
Taylor, M. D., Northcott, P. A., Korshunov, A., Remke, M., Cho, Y. J., Clifford, S. C., Eberhart, C. G., Parsons, D. W., Rutkowski, S., Gajjar, A., Ellison, D. W., Lichter, P., Gilbertson, R. J., Pomeroy, S. L., Kool, M., & Pfister, S. M. (2012). Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathologica, 123(4), 465–472.
Kool, M., Korshunov, A., Remke, M., Jones, D. T., Schlanstein, M., Northcott, P. A., Cho, Y. J., Koster, J., Schouten-van Meeteren, A., van Vuurden, D., Clifford, S. C., Pietsch, T., von Bueren, A., Rutkowski, S., McCabe, M., Collins, V. P., Bäcklund, M. L., Haberler, C., Bourdeaut, F., Delattre, O., Doz, F., Ellison, D. W., Gilbertson, R. J., Pomeroy, S. L., Taylor, M. D., Lichter, P., & Pfister, S. M. (2012). Molecular subgroups of medulloblastoma: an international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, group 3, and group 4 medulloblastomas. Acta Neuropathologica, 123(4), 473–484.
Clifford, S. C., Lusher, M. E., Lindsey, J. C., Langdon, J. A., Gilbertson, R. J., Straughton, D., & Ellison, D. W. (2006). Wnt/wingless pathway activation and chromosome 6 loss characterize a distinct molecular sub-group of medulloblastomas associated with a favorable prognosis. Cell Cycle, 5(22), 2666–2670.
Ellison, D. W., et al. (2005). Beta-catenin status predicts a favorable outcome in childhood medulloblastoma: the United Kingdom Children’s Cancer Study Group Brain Tumour Committee. Journal of Clinical Oncology, 23(31), 7951–7957.
Louis, D. N., Perry, A., Reifenberger, G., von Deimling, A., Figarella-Branger, D., Cavenee, W. K., Ohgaki, H., Wiestler, O. D., Kleihues, P., & Ellison, D. W. (2016). The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathologica, 131(6), 803–820.
Ramaswamy, V., Remke M, Bouffet E., Bailey S., Clifford SC., et al. (2016). Risk stratification of childhood medulloblastoma in the molecular era: the current consensus. Acta Neuropathologica, 131(6), 821–31.
Johnston, D. L., et al. (2018). Survival following tumor recurrence in children with medulloblastoma. Journal of Pediatric Hematology/Oncology.
Johnston, D. L., Keene, D., Kostova, M., Lafay-Cousin, L., Fryer, C., Scheinemann, K., Carret, A. S., Fleming, A., Percy, V., Afzal, S., Wilson, B., Bowes, L., Zelcer, S., Mpofu, C., Silva, M., Larouche, V., Brossard, J., Strother, D., & Bouffet, E. (2015). Survival of children with medulloblastoma in Canada diagnosed between 1990 and 2009 inclusive. Journal of Neuro-Oncology, 124(2), 247–253.
Koschmann, C., et al. (2016). Survival after relapse of medulloblastoma. Journal of Pediatric Hematology/Oncology, 38(4), 269–273.
Sabel, M., Fleischhack, G., Tippelt, S., Gustafsson, G., Doz, F., Kortmann, R., Massimino, M., Navajas, A., von Hoff, K., Rutkowski, S., Warmuth-Metz, M., Clifford, S. C., Pietsch, T., Pizer, B., Lannering, B., & SIOP-E Brain Tumour Group. (2016). Relapse patterns and outcome after relapse in standard risk medulloblastoma: a report from the HIT-SIOP-PNET4 study. Journal of Neuro-Oncology, 129(3), 515–524.
Bowers, D. C., Gargan, L., Weprin, B. E., Mulne, A. F., Elterman, R. D., Munoz, L., Giller, C. A., & Winick, N. J. (2007). Impact of site of tumor recurrence upon survival for children with recurrent or progressive medulloblastoma. Journal of Neurosurgery, 107(1 Suppl), 5–10.
Perreault, S., Lober, R. M., Carret, A. S., Zhang, G., Hershon, L., Décarie, J. C., Yeom, K., Vogel, H., Fisher, P. G., & Partap, S. (2013). Relapse patterns in pediatric embryonal central nervous system tumors. Journal of Neuro-Oncology, 115(2), 209–215.
Cavalli, F. M. G., Remke, M., Rampasek, L., Peacock, J., Shih, D. J. H., Luu, B., Garzia, L., Torchia, J., Nor, C., Morrissy, A. S., Agnihotri, S., Thompson, Y. Y., Kuzan-Fischer, C. M., Farooq, H., Isaev, K., Daniels, C., Cho, B. K., Kim, S. K., Wang, K. C., Lee, J. Y., Grajkowska, W. A., Perek-Polnik, M., Vasiljevic, A., Faure-Conter, C., Jouvet, A., Giannini, C., Nageswara Rao, A. A., Li, K. K. W., Ng, H. K., Eberhart, C. G., Pollack, I. F., Hamilton, R. L., Gillespie, G. Y., Olson, J. M., Leary, S., Weiss, W. A., Lach, B., Chambless, L. B., Thompson, R. C., Cooper, M. K., Vibhakar, R., Hauser, P., van Veelen, M., Kros, J. M., French, P. J., Ra, Y. S., Kumabe, T., López-Aguilar, E., Zitterbart, K., Sterba, J., Finocchiaro, G., Massimino, M., van Meir, E., Osuka, S., Shofuda, T., Klekner, A., Zollo, M., Leonard, J. R., Rubin, J. B., Jabado, N., Albrecht, S., Mora, J., van Meter, T., Jung, S., Moore, A. S., Hallahan, A. R., Chan, J. A., Tirapelli, D. P. C., Carlotti, C. G., Fouladi, M., Pimentel, J., Faria, C. C., Saad, A. G., Massimi, L., Liau, L. M., Wheeler, H., Nakamura, H., Elbabaa, S. K., Perezpeña-Diazconti, M., Chico Ponce de León, F., Robinson, S., Zapotocky, M., Lassaletta, A., Huang, A., Hawkins, C. E., Tabori, U., Bouffet, E., Bartels, U., Dirks, P. B., Rutka, J. T., Bader, G. D., Reimand, J., Goldenberg, A., Ramaswamy, V., & Taylor, M. D. (2017). Intertumoral heterogeneity within medulloblastoma subgroups. Cancer Cell, 31(6), 737–754 e6.
Ramaswamy, V., Remke, M., Bouffet, E., Faria, C. C., Perreault, S., Cho, Y. J., Shih, D. J., Luu, B., Dubuc, A. M., Northcott, P. A., Schüller, U., Gururangan, S., McLendon, R., Bigner, D., Fouladi, M., Ligon, K. L., Pomeroy, S. L., Dunn, S., Triscott, J., Jabado, N., Fontebasso, A., Jones, D. T., Kool, M., Karajannis, M. A., Gardner, S. L., Zagzag, D., Nunes, S., Pimentel, J., Mora, J., Lipp, E., Walter, A. W., Ryzhova, M., Zheludkova, O., Kumirova, E., Alshami, J., Croul, S. E., Rutka, J. T., Hawkins, C., Tabori, U., Codispoti, K. E., Packer, R. J., Pfister, S. M., Korshunov, A., & Taylor, M. D. (2013). Recurrence patterns across medulloblastoma subgroups: an integrated clinical and molecular analysis. The Lancet Oncology, 14(12), 1200–1207.
Packer, R. J., Zhou, T., Holmes, E., Vezina, G., & Gajjar, A. (2013). Survival and secondary tumors in children with medulloblastoma receiving radiotherapy and adjuvant chemotherapy: results of Children’s Oncology Group trial A9961. Neuro-Oncology, 15(1), 97–103.
Kameda-Smith, M. M., Wang, A., Abdulhadi, N., Voth, R., Sergeant, A., Maharaj, A., Bakhshinyan, D., Adile, A. A., Pai, A. M., Ajani, O., Yarascavitch, B., Alyman, M. C., Duckworth, J., Samaan, M. C., Farrokhyar, F., Singh, S. K., Fleming, A., & Pediatric Brain Tumour Study Group. (2019). Salvage therapy for childhood medulloblastoma: a single center experience. The Canadian Journal of Neurological Sciences, 46(4), 403–414.
Robinson, G. W., et al. (2018). Risk-adapted therapy for young children with medulloblastoma (SJYC07): therapeutic and molecular outcomes from a multicentre, phase 2 trial. The Lancet Oncology, 19(6), 768–784.
Lafay-Cousin, L., Bouffet, E., Onar-Thomas, A., Billups, C. A., Hawkins, C., Eberhart, C., Horbinski, C., Robinson, G. W., Strother, D. R., Heier, L., Souweidane, M. M., Fouladi, M., Gajjar, A., & Children Oncology Group. (2017). ACNS1221: A phase II study for the treatment of non metastatic desmoplastic medulloblastoma in children less than 4 years of age-a report of the Children Oncology Group. Journal of Clinical Oncology,35(15_suppl), 10505–10505.
ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Identifier: NCT03434262, SJDWAN: St. Jude Children's Research Hospital Phase 1 study evaluating molecularly-driven doublet therapies for children and young adults with recurrent brain tumours. Available from: https://clinicaltrials.gov/ct2/show/NCT03434262?term;SJDAWN&draw;2&rank;1. Accessed 31 Oct 2019.
Perreault, S., Ramaswamy, V., Achrol, A. S., Chao, K., Liu, T. T., Shih, D., Remke, M., Schubert, S., Bouffet, E., Fisher, P. G., Partap, S., Vogel, H., Taylor, M. D., Cho, Y. J., & Yeom, K. W. (2014). MRI surrogates for molecular subgroups of medulloblastoma. AJNR. American Journal of Neuroradiology, 35(7), 1263–1269.
Mata-Mbemba, D., Zapotocky, M., Laughlin, S., Taylor, M. D., Ramaswamy, V., & Raybaud, C. (2018). MRI characteristics of primary tumors and metastatic lesions in molecular subgroups of pediatric medulloblastoma: a single-center study. AJNR. American Journal of Neuroradiology, 39(5), 949–955.
Lastowska, M., et al. (2018). Medulloblastoma with transitional features between group 3 and group 4 is associated with good prognosis. Journal of Neuro-Oncology, 138(2), 231–240.
Bonner, E. R., et al. (2018). Liquid biopsy for pediatric central nervous system tumors. NPJ Precis Oncol, 2, 29.
Phoenix, T. N., et al. (2016). Medulloblastoma genotype dictates blood brain barrier phenotype. Cancer Cell, 29(4), 508–522.
Moxon-Emre, I., Bouffet, E., Taylor, M. D., Laperriere, N., Scantlebury, N., Law, N., Spiegler, B. J., Malkin, D., Janzen, L., & Mabbott, D. (2014). Impact of craniospinal dose, boost volume, and neurologic complications on intellectual outcome in patients with medulloblastoma. Journal of Clinical Oncology, 32(17), 1760–1768.
ClinicalTrials.gov, A study assessing the feasibility of a surgery and chemotherapy-only in children with Wnt positive medulloblastoma. 2018, ethesda (MD): National Library of Medicine (US).
ClinicalTrials.gov, Reduced craniospinal radiation therapy and chemotherapy in treating younger patients with newly diagnosed WNT-driven medulloblastoma. 2018, National Library of Medicine (US): Bethesda (MD).
ClinicalTrials.gov, A clinical and molecular risk-directed therapy for newly diagnosed medulloblastoma. 2013: Bethesda (MD): National Library of Medicine (US).
ClinicalTrials.gov, International Society of Paediatric Oncology (SIOP) PNET 5 Medulloblastoma. 2014, ethesda (MD): National Library of Medicine (US).
Kameda-Smith, M. M., et al. (2013). Time to diagnosis of paediatric posterior fossa tumours: an 11-year west of Scotland experience 2000-2011. British Journal of Neurosurgery, 27(3), 364–369.
Sergeant, A., et al. (2017). Analysis of surgical and MRI factors associated with cerebellar mutism. Journal of Neuro-Oncology, 133(3), 539–552.
Gottardo, N. G., Hansford, J. R., McGlade, J., Alvaro, F., Ashley, D. M., Bailey, S., Baker, D. L., Bourdeaut, F., Cho, Y. J., Clay, M., Clifford, S. C., Cohn, R. J., Cole, C. H., Dallas, P. B., Downie, P., Doz, F., Ellison, D. W., Endersby, R., Fisher, P. G., Hassall, T., Heath, J. A., Hii, H. L., Jones, D. T., Junckerstorff, R., Kellie, S., Kool, M., Kotecha, R. S., Lichter, P., Laughton, S. J., Lee, S., McCowage, G., Northcott, P. A., Olson, J. M., Packer, R. J., Pfister, S. M., Pietsch, T., Pizer, B., Pomeroy, S. L., Remke, M., Robinson, G. W., Rutkowski, S., Schoep, T., Shelat, A. A., Stewart, C. F., Sullivan, M., Taylor, M. D., Wainwright, B., Walwyn, T., Weiss, W. A., Williamson, D., & Gajjar, A. (2014). Medulloblastoma down under 2013: a report from the third annual meeting of the International Medulloblastoma Working Group. Acta Neuropathologica, 127(2), 189–201.
ClinicalTrials.gov, A dose exploration study with MK-8628 in participants with selected advanced solid tumors (MK-8628-006). 2018, Bethesda (MD): National Library of Medicine (US).
ClinicalTrials.gov, A dose-finding study of MK-8628, a small molecule inhibitor of the bromodomain and extra-terminal (BET) proteins, in adults with selected advanced solid tumors (MK-8628-003). 2018, National Library of Medicine (US). Bethesda (MD).
Graff, J. N., Higano, C. S., Hahn, N. M., Taylor, M. H., Zhang, B., Zhou, X., Venkatakrishnan, K., Leonard, E. J., & Sarantopoulos, J. (2016). Open-label, multicenter, phase 1 study of alisertib (MLN8237), an aurora a kinase inhibitor, with docetaxel in patients with solid tumors. Cancer, 122(16), 2524–2533.
Schoffski, P., et al. (2011). Phase I, open-label, multicentre, dose-escalation, pharmacokinetic and pharmacodynamic trial of the oral aurora kinase inhibitor PF-03814735 in advanced solid tumours. European Journal of Cancer, 47(15), 2256–2264.
Seymour, J. F., et al. (2014). A phase 2 study of MK-0457 in patients with BCR-ABL T315I mutant chronic myelogenous leukemia and Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood Cancer Journal, 4, e238.
Bouffet, E. (2019). Management of high-risk medulloblastoma. Neurochirurgie.
Thompson, E. M., et al. (2016). Prognostic value of medulloblastoma extent of resection after accounting for molecular subgroup: a retrospective integrated clinical and molecular analysis. The Lancet Oncology.
Acknowledgments
I would like to acknowledge all of the children, families, and international society of researchers who have helped advance the understanding of pediatric MB.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kameda-Smith, M.M. Pediatric medulloblastoma in the molecular era: what are the surgical implications?. Cancer Metastasis Rev 39, 235–243 (2020). https://doi.org/10.1007/s10555-020-09865-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-020-09865-y