Abstract
Background
The differences between perihilar cholangiocarcinoma (PHCC) and distal cholangiocarcinoma (DCC) regarding recurrence and the factors that affect recurrence after surgery are unclear. This study aims to investigate the differences in recurrence patterns between patients with PHCC and those with DCC after surgical resection with curative intent. It also investigates the risk factors associated with recurrence and survival thereafter.
Patients and Methods
The postoperative courses of 366 patients with extrahepatic cholangiocarcinomas (EHCCs), including 236 with PHCC and 130 with DCC, who underwent surgical resections were investigated retrospectively.
Results
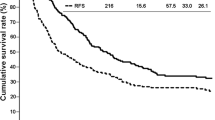
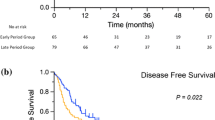
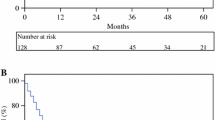
During follow-up, tumors recurred in 143 (60.6%) patients with PHCC and in 72 (55.4%) patients with DCC. Overall survival (OS) after surgery, recurrence-free survival (RFS), and OS after recurrence were similar for the patients with PHCC and those with DCC. The cumulative probability of recurrence declined 3 years after surgery in the patients with PHCC and those with DCC. A multivariable analysis determined that, among the patients with PHCC and those with DCC, regional lymph node metastasis was a significant risk factor associated with RFS. Ten patients with PHCC and eight patients with DCC with two or fewer sites of recurrence in a single organ underwent resections. A multivariable analysis determined that recurrent tumor resection was an independent prognostic factor associated with OS after recurrence in the patients with PHCC and those with DCC.
Conclusions
Postoperative survival did not differ between the patients with PHCC and those with DCC. Frequent surveillances for recurrence are needed for 3 years after surgical resection of EHCCs. In selected patients, surgery for recurrent EHCCs might be associated with improved outcomes.


Similar content being viewed by others
References
Amin MB, Edge S, Greene F, et al. AJCC Cancer staging manual 8th edition. 8th ed. New York: Springer; 2016.
Komaya K, Ebata T, Yokoyama Y, et al. Recurrence after curative-intent resection of perihilar cholangiocarcinoma: analysis of a large cohort with a close postoperative follow-up approach. Surgery. 2018;163(4):732–8.
Groot Koerkamp B, Wiggers JK, Allen PJ, et al. Recurrence rate and pattern of perihilar cholangiocarcinoma after curative intent resection. J Am Coll Surg. 2015;221(6):1041–9.
Kim YS, Hwang IG, Park SE, et al. Role of adjuvant therapy after R0 resection for patients with distal cholangiocarcinoma. Cancer Chemother Pharmacol. 2016;77(5):979–85.
Komaya K, Ebata T, Shirai K, et al. Recurrence after resection with curative intent for distal cholangiocarcinoma. Br J Surg. 2017;104(4):426–33.
Nakanishi Y, Tsuchikawa T, Okamura K, et al. Clinicopathological features and prognosis of advanced biliary carcinoma centered in the cystic duct. HPB (Oxford). 2018;20(1):28–33.
Sakata J, Wakai T, Matsuda Y, et al. Comparison of number versus ratio of positive lymph nodes in the assessment of lymph node status in extrahepatic cholangiocarcinoma. Ann Surg Oncol. 2016;23(1):225–34.
Kobayashi A, Miwa S, Nakata T, Miyagawa S. Disease recurrence patterns after R0 resection of hilar cholangiocarcinoma. Br J Surg. 2010;97(1):56–64.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Hepatobiliary Cancers Version 4.2019. NCCN. org. https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf. Accessed 20 Dec 2019.
Kobayashi S, Konishi M, Kato Y, et al. Surgical outcomes of multicentric adenocarcinomas of the biliary tract. Jpn J Clin Oncol. 2011;41(9):1079–85.
Shinohara K, Shimoyama Y, Ebata T, et al. Clinicopathologic study on metachronous double cholangiocarcinomas of perihilar and subsequent distal bile duct origin. Surgery. 2017;162(1):84–93.
Primrose JN, Fox RP, Palmer DH, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019;20(5):663–673.
Takahashi Y, Ebata T, Yokoyama Y, et al. Surgery for recurrent biliary tract cancer: a single-center experience with 74 consecutive resections. Ann Surg. 2015;262(1):121–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have no conflicts of interest or funding to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakanishi, Y., Okamura, K., Tsuchikawa, T. et al. Time to Recurrence After Surgical Resection and Survival After Recurrence Among Patients with Perihilar and Distal Cholangiocarcinomas. Ann Surg Oncol 27, 4171–4180 (2020). https://doi.org/10.1245/s10434-020-08534-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08534-2