Abstract
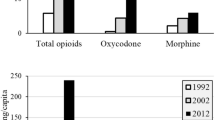
Naloxone is an opioid antagonist with high affinity for μ-opioid receptor, and for this reason it is used for the emergency treatment of opioid overdose. Originally, it was available only as an injectable product. However, for the ease of administration, intranasal (IN) formulations have also become available. These IN formulations contain preservatives and stabilizers such as benzalkonium chloride (BKC), benzyl alcohol (BA), and ethylenediaminetetraacetic acid (EDTA). Some of these ingredients are known to affect permeability of drugs. This study focuses on investigating the effect of formulation variables including choice of preservatives, stabilizer, and pH on the permeability and stability of naloxone IN formulations. The in vitro permeability of naloxone was evaluated employing EpiAirway™ tissue-mounted Ussing chambers. BKC was found to enhance the apparent permeability (Papp) of naloxone significantly (p < 0.05) at very low concentration, while BA caused similar enhancement at a much higher concentration. EDTA was found to decrease Papp of naloxone by lowering the pH, and thePapp of naloxone was found to decrease approximately 51-fold with the decrease in formulation pH from 6.0 to 4.0. The product stability was, however, found optimal only below pH 5.0. Thus, selection of formulation ingredients, buffering agent, and pH of IN formulation is a balancing act for achieving desired permeability and optimal stability to achieve reasonable shelf life of naloxone IN formulation.









Similar content being viewed by others
References
Overdose death rates. National Institute on Drug Abuse. Available from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed 16 Apr 2019.
Haddox JD. Opioids with abuse-deterrent properties: a regulatory and technological overview. J Opioid Manag. 2017;13(6):397–413.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharmacol Toxicol. 2017;58:143–59.
Lewis CR, Vo HT, Fishman M. Intranasal naloxone and related strategies for opioid overdose intervention by nonmedical personnel: a review. Subst Abus Rehabil. 2017;8:79–95. https://doi.org/10.2147/SAR.S101700.
Wolfe TR, Bernstone T. Intranasal drug delivery: an alternative to intravenous administration in selected emergency cases. J Emerg Nurs. 2004;30(2):141–7. https://doi.org/10.1016/j.jen.2004.01.006.
Robertson TM, Hendey GW, Stroh G, Shalit M. Intranasal naloxone is a viable alternative to intravenous naloxone for prehospital narcotic overdose. Prehosp Emerg Care. 2009;13(4):512–5. https://doi.org/10.1080/10903120903144866.
Merlin MA, Saybolt M, Kapitanyan R, Alter SM, Jeges J, Liu J, et al. Intranasal naloxone delivery is an alternative to intravenous naloxone for opioid overdoses. Am J Emerg Med. 2010;28(3):296–303. https://doi.org/10.1016/j.ajem.2008.12.009.
Press release: Indivior receives complete response letter from FDA not approving naloxone nasal spray new drug application for opioid overdose 2015. Available from: http://indivior.com/wp-content/uploads/2015/11/Nasal-Naloxone-Final-Release_1124151.pdf. Accessed 16 Apr 2019.
Press Release: Amphastar announces the receipt of a CRL for intranasal naloxone for the emergency treatment of opioid overdose 2017. Available from: http://ir.amphastar.com/static-files/19b13150-7ff8-4d3b-8e3f-452578083dbb. Accessed 16 Apr 2019.
Hertz S., Narcan nasal spray summary review for regulatory action US Food and Drug Administration. 2015. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/208411Orig1s000SumR.pdf. Accessed 16 Apr 2019.
Kerr D, Kelly AM, Dietze P, Jolley D, Barger B. Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction. 2009;104(12):2067–74.
McDonald R, Danielsson Glende Ø, Dale O, Strang J. International patent applications for non-injectable naloxone for opioid overdose reversal: exploratory search and retrieve analysis of the PatentScope database. Drug Alcohol Rev. 2018;37(2):205–15. https://doi.org/10.1111/dar.12571.
Adapt Pharma Inc. Narcan - naloxone hydrochloride spray In: Drugs@FDA: FDA approve drug products. Adapt Pharma Inc. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/208411lbl.pdf. Accessed 16 Apr 2019.
Keegan F, Bell RG, Crystal R, Weiss MB. Nasal drug products and methods of their use. US Patent. 2017;9,775,838.
Crystal R, Weiss MB. Nasal drug products and methods of their use. US Patent. 2015;9,211,253.
Sharma S, Kulkarni J, Pawar A. Permeation enhancers in the transmucosal delivery of macromolecules. Pharmazie. 2006;61(6):495–504.
Wyse J, DeHart MP. Intranasal naloxone compositions and methods of making and using same. US Patent. 2015;9,192,570.
Tylleskar I, Skulberg AK, Nilsen T, Skarra S, Jansook P, Dale O. Pharmacokinetics of a new, nasal formulation of naloxone. Eur J Clin Pharmacol. 2017;73(5):555–62. https://doi.org/10.1007/s00228-016-2191-1.
McDonald R, Lorch U, Woodward J, Bosse B, Dooner H, Mundin G, et al. Pharmacokinetics of concentrated naloxone nasal spray for opioid overdose reversal: phase I healthy volunteer study. Addiction. 2018;113(3):484–93. https://doi.org/10.1111/add.14033.
Mundin G, McDonald R, Smith K, Harris S, Strang J. Pharmacokinetics of concentrated naloxone nasal spray over first 30 minutes post-dosing: analysis of suitability for opioid overdose reversal. Addiction. 2017;112(9):1647–52. https://doi.org/10.1111/add.13849.
Wheatley M, Dent J, Wheeldon E, Smith P. Nasal drug delivery: an in vitro characterization of transepithelial electrical properties and fluxes in the presence or absence of enhancers. J Control Release. 1988;8(2):167–77.
Bechgaard E, Gizurarson S, Jørgensen L, Larsen R. The viability of isolated rabbit nasal mucosa in the Ussing chamber, and the permeability of insulin across the membrane. Int J Pharm. 1992;87(1–3):125–32.
Chemuturi NV, Hayden P, Klausner M, Donovan MD. Comparison of human tracheal/bronchial epithelial cell culture and bovine nasal respiratory explants for nasal drug transport studies. J Pharm Sci. 2005;94(9):1976–85.
Leonard AK, Sileno AP, MacEvilly C, Foerder CA, Quay SC, Costantino HR. Development of a novel high-concentration galantamine formulation suitable for intranasal delivery. J Pharm Sci. 2005;94(8):1736–46. https://doi.org/10.1002/jps.20389.
Van Breemen RB, Li Y. Caco-2 cell permeability assays to measure drug absorption. Expert Opin Drug Metab Toxicol. 2005;1(2):175–85.
Hispira, Inc. Naloxone hydrochloride- naloxone hydrochloride injection, solution. In: FDA Label Search Available from: https://www.accessdata.fda.gov/spl/data/a91e6c30-fb00-4ae0-be36-ccd1f2363e15/a91e6c30-fb00-4ae0-be36-ccd1f2363e15.xml. Accessed 16 Apr 2019.
Mylan Institutional LLC. Naloxone hydrochloride- naloxone hydrochloride injection, solution. In: FDA Label Search. Available from: https://www.accessdata.fda.gov/spl/data/69401599-0f6a-4055-9dde-0e57d66afe93/69401599-0f6a-4055-9dde-0e57d66afe93.xml. Accessed 16 Apr 2019.
Marttin E, Verhoef J, Romeijn S, Zwart P, Merkus F. Acute histopathological effects of benzalkonium chloride and absorption enhancers on rat nasal epithelium in vivo. Int J Pharm. 1996;141(1–2):151–60.
Fabrizio B, Giulia BA, Fabio S, Paola R, Gaia C. In vitro permeation of desmopressin across rabbit nasal mucosa from liquid nasal sprays: the enhancing effect of potassium sorbate. Eur J Pharm Sci. 2009;37(1):36–42.
Cho E, Gwak H, Chun I. Formulation and evaluation of ondansetron nasal delivery systems. Int J Pharm. 2008;349(1):101–7.
Tomita M, Hayashi M, Awazu S. Comparison of absorption-enhancing effect between sodium caprate and disodium ethylenediaminetetraacetate in Caco-2 cells. Biol Pharm Bull. 1994;17(5):753–5.
Tomita M, Hayashi M, Awazu S. Absorption-enhancing mechanism of EDTA, caprate, and decanoylcarnitine in Caco-2 cells. J Pharm Sci. 1996;85(6):608–11. https://doi.org/10.1021/js9504604.
Grassin-Delyle S, Buenestado A, Naline E, Faisy C, Blouquit-Laye S, Couderc L-J, et al. Intranasal drug delivery: an efficient and non-invasive route for systemic administration: focus on opioids. Pharmacol Ther. 2012;134(3):366–79.
England RJ, Homer JJ, Knight LC, Ell SR. Nasal pH measurement: a reliable and repeatable parameter. Clin Otolaryngol Allied Sci. 1999;24(1):67–8.
Cho DY, Hwang PH, Illek B, Fischer H. Acid and base secretion in freshly excised nasal tissue from cystic fibrosis patients with ΔF508 mutation. Int Forum Allergy Rhinol. 2011;1(2):123–7. https://doi.org/10.1002/alr.20028.
Washington N, Steele R, Jackson S, Bush D, Mason J, Gill D, et al. Determination of baseline human nasal pH and the effect of intranasally administered buffers. Int J Pharm. 2000;198(2):139–46.
Inactive ingredient database U.S. Food and Drug Administration. 2018. Available from: https://www.accessdata.fda.gov/scripts/cder/iig/index.cfm. Accessed 16 Apr 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
This manuscript reflects the views of the authors and should not be construed to represent FDA’s views or policies.
Additional information
Guest Editors: Heather Boyce, Steve R. Byrn, and Stephen W. Hoag
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hsu, HJ., Yang, Y., Pavuluri, V. et al. Effect of Formulation Variables on the Nasal Permeability and Stability of Naloxone Intranasal Formulations. AAPS PharmSciTech 20, 232 (2019). https://doi.org/10.1208/s12249-019-1452-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-019-1452-6