Abstract
Imrecoxib is a registered treatment for osteoarthritis pain symptoms in China. This study aims to assess the effect of imrecoxib on the pharmacodynamics and pharmacokinetics of warfarin. 12 healthy male volunteers with CYP2C9*3 AA and VKORC1 AA genotypes took a 5 mg dose of warfarin both alone and concomitantly with steady-state imrecoxib. Both warfarin alone and concomitantly with imrecoxib have safey and good tolerance across the trial. Following warfarin and imrecoxib co-administration, neither Cmax, AUC0-t and t1/2 of warfarin enantiomers nor AUC of international normalized ratio (INR) were markedly different from those of warfarin alone. The geometric mean ratios (GMRs) (warfarin + imrecoxib: warfarin alone) of INR(AUC) was 1 (0.99, 1.01). The GMRs of warfarin AUC0-∞ (90% confidence interval, CIs) for warfarin + imrecoxib: warfarin alone were 1.12 (1.08, 1.16) for R-warfarin and 1.13 (1.07, 1.18) for S- warfarin. The 90% CIs of the GMRs of AUC0-∞, Cmax and INR (AUC) were all within a 0.8–1.25 interval. The combination of warfarin and imrecoxib did not impact the pharmacodynamics and pharmacokinetics of single-dose warfarin; therefore, when treating a patient with imrecoxib and warfarin, it is not required to adjust the dosage of warfarin.
Similar content being viewed by others
Introduction
The incidence of Osteoarthritis (OA) is more than 50% in people over 60 years old in China1,2. OA has a serious impact on patients’ ability to function and leads to considerable societal costs3. The clinical characteristics of OA are related to the development of aches, discomfort, rigidity, cartilage degradation and bone remodeling1, OA’s treatment focuses on symptom control, and mainly aims to relieve joint swelling and ease pain. Selective cyclooxygenase (COX)-2 inhibitor are frequently prescribed to OA patients due to their inhibition of the inflammatory cascades and relief of the pain symptoms.
Imrecoxib, 4-(4-methylsulfonyl-phenyl)-1-propyl-3-(p-tolyl)-1H-pyrrol-2(5H)-one (Fig. 1), is a new and moderate selective COX-2 inhibitor4. It is currently registered in China for the symptomatic treatment of osteoarthritis and has been widely prescribed since its launch in 20115. It has been reported that the single-dose pharmacokinetics of imrecoxib were linear over the 30 to 200 mg dose range. The t1/2 of imrecoxib is 20 hours, tmax occurred at 2 hours following oral consumption. No accumulated effects were observed in plasma after administration of 200 mg imrecoxib, bid, for 11 consecutive days6. Imrecoxib is metabolized by hepatic isoenzyme CYP2C9, 2D6 and 3A4 enzymes, with rates of 62.5%, 21.1% and 16.4%, respectively. Following oral ingestion, the 4′-methyl group of imrecoxib is hydroxylized to the 4′-hydroxymethyl metabolite by CYP2C9, and further oxidized to 4′-carboxylic acid metabolite7. The main metabolites in urine are the hydroxymethyl and carboxy metabolites produced by the oxidation of phenylcyclomethyl, while the carboxylic acid metabolite is primarily excreted from feces8.
Warfarin is effective for preventing intravenous thromboembolism, cardiovascular and cerebrovascular infarction, and other thromboembolic disorders. It is a racemic mixture of two isomers, CYP2C9 enzyme metabolizes S-warfarin, and CYP1A2 and CYP3A4 are responsible for metabolism of R-warfarin9, which make it susceptible to interaction with numerous inhibitors and inducers of CYPs. This interaction might lead to either an inability to achieve the expected anticoagulant effects or an enhanced bleeding risk induced by excessive anticoagulation10. In a US retrospective prescription analysis, nonsteroidal anti-inflammatory drugs (NSAIDs) with warfarin was the most frequently occurring medication pair in drug-drug interactions (DDI) reports8, and 24% of warfarin recipients would be given NSAIDs treatment within two years8,11. NSAIDs impair the gastrointestinal mucosa and aggregation of platelets by inhibiting the COX-1 isozyme12,13, which significantly enhances the risks of hemorrhage in patients taking warfarin14,15,16,17. Specific inhibitors of COX-2 have been approved for OA therapy. COX-2 specific inhibitors do not cause severe bleeding and are thus considered potentially safe for warfarin-treated patients18. However, increasing evidences of myocardial infarction, as well as cardiovascular secondary action relate to COX-2 specific inhibitors, such as rofecoxib and valdecoxib, lead to their retreat from the market19,20. Therefore, a moderate COX-2 selective inhibitor with decreased bleeding risk than NSAIDs and reduced cardiovascular secondary action compared with COX-2 specific inhibitors, would be appropriate for management of OA.
Clinical trials have demonstrated that imrecoxib shows 50% inhibitory concentration (IC50) of COX-1 and COX-2 isozymes by 115 ± 28 nmol/L and 18 ± 4 nmol/L, respectively5. The selective index (IC50, COX-1/COX2) was 6.39, which was between that of meloxicam and celecoxib21. From a clinical perspective, whilst the lack of pharmacokinetic and pharmacodynamics effects on warfarin are important in terms of dose adjustment etc, the risk of bleeding due to GI irritation is still significant with NSAIDs (including a drug of relative COX-2 specificity) plus warfarin, particularly in the elderly. In addition, both S-warfarin, the more potent enantiomer of warfarin, and imrecoxib are metabolised by the CYP2C9 enzyme8,22. However, whether co-administration of imrecoxib and warfarin would result in DDI was not investigated. In this study, we evaluated the potential DDI of imrecoxib and warfarin by comparing the pharmacodynamic and pharmacokinetic parameters of warfarin with and without co-administration of imreocxib in healthy male volunteers. We also tested the safety and tolerability of study drugs across the trial23.
Methods
Ethics
Current study was conducted in conformity to the Declaration of Helsinki (as revised in Brazil, 2013)24, Good Clinical Practice (GCP) guidelines of China Food and Drug Administration (CFDA)25 and the technical guidelines for clinical pharmacokinetic study of chemical drugs26. CFDA (no. 2011S00434) and the independent ethics committee (Tongji Medical College, Huazhong University of Science and Technology, no. (2014)185] reviewed and approved this study protocol. Written informed consent was required for every volunteer before any study procedures27.
Subjects
Twelve subjects were enrolled in this study. The inclusion requirements were (i) male; (ii) BMI ranged from 19 to 24 kg ⁄m2,26; (iii) aged between 18 to 40; (iv) qualified for complete health examination, including vital signs, electrocardiograms, routine blood test, urinalysis, biochemistry laboratory parameters, chest X-ray, liver and renal function tests are normal or not clinical significantly abnormal. (v) a condition of normal coagulation function (prothrombin time - PT, INR and fibrinogen) and negative serological test (HBsAg, HCV and HIV antibodies); (vi) voluntary signing of informed consent forms27.
As we previous reported27, subject would be excluded if he met these criterions: (i) hypersensitivity or allergy to the study drugs; (ii) any diseases or unstable medical history that may disturb the safety or the in vivo process of the study drugs, including cardiovascular, hepatic, renal, gastrointestinal, endocrine or immune system. (iii) a history of any bleeding disorders. (iv) diseases of nervous system or muscle diseases, that might affect subjects compliance; (v) alcohol or coffee addiction; (vi) participated in another clinical trial or blood donation in previous 2 months; (vii) took any drug treatment within 2 weeks.
Study design
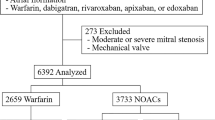
Current study is phase I clinical trial, which was designed as open-labeled and fixed-sequence, and all the information/data were collected from a single center. This study contained two phases (Fig. 2). In phase one, the volunteers received a 5 mg dose of warfarin alone at 8:00 a.m. on day 1. In the other phase, they orally took imrecoxib to steady-state (200 mg imrecoxib at 8:00 a.m. on day 8, and a 100 mg dose q.12 hours from day 8 to 10, 6 times in total), followed by a 5 mg dosage of warfarin co-administered at 8:00 a.m. on day 10. The volunteers were hospitalized on day-1 (the day before the study), 10 hours of fasting was required before administration27. Subjects should avoid any activities involved in risks of haemorrhage9. Blood samples (4 mL each) for analysis of pharmacokinetic parameters were obtained 60 minutes before dose of warfarin and 0.5, 1, 2, 3, 4, 5, 6, 8, 12, 24, 36, 48, 72, 96, 120 and 144 hours after dosing. The pharmacodynamics properties of warfarin were expressed by INR and detected by PT before and after 6, 12, 24, 36, 48, 72, 96, 120, 144 hours of warfarin dose27,28.
Analytic methods
A stable LC-MS/MS method was established for detecting S- and R-warfarin plasma concentrations. The chromatographic separation was carried out on an LC system (Shimadzu LC-20AD, Tokyo, Japan) using water and acetonitrile, and AB QTRAP 4000 system (AB Sciex, Foster City, CA, USA) in positive electrospray ion mode was hired for quantification29,30,31. Warfarin-d5 was used as the internal standard. Liquid-liquid extraction with 3 mL dichloromethane: diethyl ether: (2:3, v/v) was employed for 200 μL human plasma. Good linearity was obtained between 5.00–1000 ng/ml for each enantiomer32. The inter- and intra- precision (CVs% for 10, 100 and 800 ng/ml) were ≤5.2% for R-warfarin and ≤5.0% for S-warfarin, respectively. Inaccuracy for R-warfarin was between −6.4% to +4.2%, and ranged from −5.9% to +5.1% for S-warfarin. The mean absolute recovery was ≥87.3% (CVs <6.0%)27,33.
Pharmacokinetics and pharmacodynamics analysis
As our previous studies reported27, pharmacokinetic analysis was performed base on plasma concentrations of warfarin enantiomers at each time-point by hiring Drug and Statistics Software version 3.1.5. The measurement outcomes contained area under the profile (AUC0-t), the terminal half-life (t1/2), maximum plasma concentration observed (Cmax), time of maximum concentration (Tmax). AUC from 0 to infinity (AUC0-∞). Parameters of pharmacodynamic were estimated from the INR data on each period. PT (INR) was measured with the use of prothrombin complex assay (STA-R, SPA 50 Reagent, Diagnostica stago)34. Maximum INR (INRmax) and baseline INR (INRbaseline) were determined by PTtest divide PTnormal. The linear/logarithmic trapezoidal method was used for calculation of area under INR-time profile (AUC0–144h, INR)28.
Safety evaluations
The safety assessments were conducted on account of clinical examinations, such as evaluation of general subject appearance, vital signs and routine hematology and biochemistry assays35, together with adverse events evaluation (AEs), conducted at screening, pretreatment, post-treatment (day 7) and end of trial (day 16). Signs and symptoms relate to study drugs, such as nausea, diarrhea, vomiting, headache and dizziness, were observed and documented by the study physicians36. AEs were defined as mild, moderate or severe37. Determination of causal relationship between AEs and study drugs followed the criterions announced by the World Health Organization27.
Statistical methods
EpiData 3.0 software was used for data entry and management, statistical analysis was conducted on SAS 9.3 software programming (SAS Institute Inc., Cary, NC). The statistical significance was accepted with two-sided p < 0.0538. Pharmacokinetic and pharmacodynamic analyses were based on the subjects who finished trial without great program violation which have a major impact on pharmacokinetic and pharmacodynamic parameters. Descriptive statistics such as mean, median, range, and standard deviation were calculated for observed variables.
Log-transformation of pharmacodynamic parameters INRmax and INR(AUC) were applied. Comparing the difference between warfarin treatment and combination treatment for Tmax, logINRmax and logINR (AUC) used the F test in ANOVA analysis. The GMR and 90%CIs were calculated by back-transforming for AUC0-∞, AUC0–144h, Cmax, INRmax, Tmax and INR(AUC). The 90% CIs felled within the acceptance range of 0.80–1.25 suggest a lack of drugs interaction28.
Results
Study population
12 healthy volunteers with CYP2C9*3 AA and VKORC1 homozygous AA genotypes were enrolled. Table 1 shows the demographic characteristics, PT and INR value of the volunteers. No striking differences (p > 0.05) in age, height, weight, PT or INR were observed. Both prothrombin time and INR levels were within normal limits. Since the polymorphisms of CYP2C9 and VKORC1 account for 35–40% anticoagulant efficiency of warfarin, we tested these genotypes of the volunteers. There is no volunteer dropped out from the trial. No volunteers dropped out from the trial.
Safety and tolerability
Both warfarin alone and concomitantly with imrecoxib have safey and good tolerance in healthy volunteers across the trial. Neither severe AEs nor accidental bleeding events occurred during the trial. All the data or information of physical examination, vital signs, laboratory test results or 12-lead ECG were not meaningful altered compare to before administration. In period 1, one subject had transient elevated direct bilirubin (9.6 μmol/L, upper limit of normal = 6.8 μmol/L) on day 7, which met the definition of grade 1 AEs (>ULN — 1.5 × ULN in direct bilirubin). However, the subject did not have any associated signs or symptoms and the level of direct bilirubin stayed normal on day 16 (period 2). Therefore, the investigator considered it to be unrelated to study drugs. In period 2, one subject was observed to be experiencing mild abdominal/upper abdominal discomfort on Day 8 after the first dose of imrecoxib, which continued for about 1.5 hours and disappeared without medical treatment. This event was regarded as possibly related to the drugs. No volunteer dropped out from the trial due to adverse experiences.
Pharmacokinetics
The pharmacokinetic parameters and pharmacokinetic curves of warfarin enantiomer both warfarin alone and concomitantly with imrecoxib are listed below (Table 2, Fig. 3). Concomitant administration of imrecoxib and warfarin did not change the median Tmax value of R- and S-warfarin 0.8 (0.5~2.0) hours compared to 1.0 (0.5~3.0) hours with administration of warfarin alone (P > 0.300). The t1⁄2 of R–warfarin for recipients of warfarin alone and recipients of co-administration of imrecoxib and warfarin were 64.08 ± 15.97 hours and 59.02 ± 9.39 hours, respectively (P > 0.1). In the absence and presence of imrecoxib, the t1⁄2 for S-warfarin were 57.00 ± 15.27 hours and 51.63 ± 7.59 hours respectively (P > 0.1). Receiving imrecoxib did not change Vz/F of R-warfarin, however, a decrease of 16% was observed for Vz/F of S-warfarin, the mean Vz/F slightly decreased from 12.65 ± 2.55 to 10.61 ± 1.89 (P = 0.01 for co-administration of imrecoxib versus warfarin alone treatment). As summarized in Table 3, compare imrecoxib and warfarin in combination to warfarin alone, the GMR of R-warfarin AUC0–144h and Cmax were 1.14 and 1.06, respectively, and the 90% CIs ranged from 0.93–1.13 and 0.98–1.15, both of which were within 0.8–1.25. For the S-warfarin enantiomer, the GMR of Cmax and AUC0-t were 1.03 and 1.14, and the corresponding 90% CI were 0.93–1.13 and 1.09–1.20. All 90% CIs were in the range of 0.80–1.25. These results suggest that the pharmacokinetic profiles of S- and R-warfarin were not significantly impacted by co-administration of imrecoxib.
Pharmacodynamics
The mean INR-time profiles of warfarin alone or concomitant with imrecoxib are shown in Fig. 4. The median Tmax (time to maximum observed effect) value for warfarin alone and co-administration of warfarin with imrecoxib were 15.10 hours and 14.45 hours, respectively. Although co-administration of warfarin and imrecoxib caused a small, transient decrease in INR value at 12 hours, mean INR values over time were similar between these two groups. The geometric mean ratio of pharmacodynamic parameters (INRmax, Tmax, INR (AUC), 90% CI, imrecoxib plus warfarin versus warfarin alone) were 0.94 (0.90–0.98), 0.96 (0.92–0.99) and 1.00 (0.99–1.01), respectively. The corresponding 90% CIs for each of these values were entirely within 0.8–1.25 (Table 4). A log transformation was applied for INRmax and INR(AUC). There was no significant difference for log INRmax, logINR(AUC) and Tmax during concurrent imrecoxib treatment compared with warfarin alone treatment (Table 5).
Discussion
This study revealed the pharmacodynamics and pharmacokinetics of warfarin would not be altered by concomitant administration of imrecoxib with the clinically recommended dosage. As an innovative and mild selective COX-2 inhibitor, imrecoxib can probably be prescribed to patients with cardiovascular disease and stable long-term warfarin therapy4. Several studies indicated an increasing INR value of healthy volunteers and accidental bleeding in patients stable on warfarin therapy after dosing celecoxib, which with similar therapeutic efficacy and side effects to imrecoxib39,40,41,42,43. Monitoring the INR of long-term warfarin recipients is required to optimize effective dosage because of a large inter-individual variation and narrow therapeutic window44. S-warfarin is metabolized by CYP2C9 enzyme8,22,45, as well as imrecoxib. S-warfarin directly inhibits vitamin K-dependent coagulation factors46, and accounts for 85% anticoagulant activity of warfarin22. Competition of the CYP2C9 metabolic enzyme may occur when patients receive warfarin and imrecoxib, which prevents S-warfarin from being metabolized to S-7-hydroxywarfarin, resulting in an increase of plasma concentration and anticoagulant effects of S-warfarin. Both warfarin (99%) and imrecoxib (96%) are highly protein bound in plasma. Imrecoxib may competitively displace warfarin from the protein-binding sites, enhancing blood concentration of free warfarin and increasing bleeding risks. Thus, we speculated that imrecoxib and warfarin may interact.
Inconsistent with our speculation, the results indicated the pharmacokinetic profiles of warfarin enantiomers were not significantly changed by co-administration of imrecoxib. Comparing co-administered warfarin and imrecoxib with warfarin alone, for S-warfarin, the outer bound of 90% CIs of AUC0–144h increased to 20% (Table 3), but AUC0–144h and AUC0-∞ were not significantly changed (Table 2), and the GMRs for and 90% CIs for AUC0-∞, AUC0–144h and Cmax were all within 0.80–1.25 (Table 3). PT were expressed by an INR value in this study. Monitoring of PT is required for individualized dosage adjustments in clinical warfarin use. There were no meaningful disparities in Tmax, logINR (AUC) and logINRmax observed between two treatments. Although the mean INR at 12 hour, near the Tmax, was significantly reduced when dosed with imrecoxib, the GMR and 90% CI of INR AUC0–144 h for warfarin + imrecoxib: warfarin only were near identical, 1 (0.99, 1.01) (Table 4), and no significant difference in logINRmax was observed (Table 5). These results suggested imrecoxib would not alter the pharmacokinetics parameters and anticoagulation activity of warfarin, but greater caution should be taken in the wider applicability of the results.
It has been widely agreed that the anticoagulant efficiency of warfarin is highly related to genetic polymorphisms. Among these genes, CYP2C9 and VKORC1 are responsible for 30% to 40% of the warfarin efficiency differentiation47,48,49,50,51. People with these polymorphisms show a significant difference in warfarin pharmacodynamic and pharmacokinetic profiles compared to wildtype subjects. For a better evaluation, all volunteers enrolled in this study were CYP2C9*3 AA genotype and VKORC1 (G-1639A) with homozygous AA genotype. Several studies have reported the frequency of CYP2C9 *3 AA and AC genotypes were 95% and 5%, respectively, and mutation frequency of VKORC1–1639 AG and AA were 7.4% and 92.6% in the Han-Chinese population52,53,54,55,56,57. Warfarin-induced hemorrhage associated with age58. Significant reduction in clearance of warfarin with age was also reported59. Healthy volunteers aged from 18 to 45 years old are recommended by guideline26. However, in a large Japanese reports analysis, the reporting odds ratio of hemorrhagic events associated warfarin in patients age 40–49 significantly lower than those aged ≤40 or those aged ≥5060. In addition, many studies focusing on age and warfarin’s efficiency divided the volunteers’ age into young and elderly groups. The age range of these groups was 18–40 and 65–90 respectively. Therefore, we enrolled the volunteers between 18 and 40 years old to rule out the influence of age on warfarin.
A loading dose of 200 mg imrecoxib was chosen, then subsequently taking 5 continuous 100 mg doses of imrecoxib in order, to guarantee imrecoxib reaches its steady-state concentration prior to warfarin dose in this study. Clinically recommended dosage is 5 mg for warfarin and 100 mg for imrecoxib. The dosage of warfarin used in some studies was 25 mg61,62,63. We used 5 mg warfarin in both periods, to ensure adequate plasma drug levels close to common clinic levels while avoiding exposing participants to unnecessary bleeding risks caused by excessive use of warfarin. Consistent with our study, the existence of an interaction between warfarin (5 mg/d) and celecoxib was evaluated in a study with 24 healthy volunteers64,65,66, and 7.5 mg warfarin was used to examine potential drug interactions with celecoxib in healthy volunteer studies28,67.
In conclusion, this study revealed that co-administration of imrecoxib did not affect the pharmacokinetic parameters or anticoagulant properties of warfarin. Thus, we concluded that adjusting dosage is not necessary when administering imrecoxib concomitantly with warfarin. However, we only conducted a single dose study of warfarin, so the possibility that a higher dosage or multiple doses of warfarin would alter its pharmacokinetic or pharmacodynamic profiles during co-administration with imrecoxib could not be excluded, though the clinical relevance would be doubtful.
References
Chinese academy of rheumatology. Diagnostic guidelines for osteoarthritis (protocol). Chinese Journal of Rheumatology, 702–704 (2003).
Chinese academy of rheumatology. Diagnostic guidelines for osteoarthritis Chinese Journal of Rheumatology, 793–795 (2007).
Bannuru, R. R. et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Annals of internal medicine 162, 46–54, https://doi.org/10.7326/M14-1231 (2015).
Zuo, C. Z. et al. Effect of Fluconazole on the Pharmacokinetic Properties of Imrecoxib, a Novel NSAID: A Single-center, Open-label, Self-controlled Study in Healthy Chinese Male Volunteers. Clinical therapeutics 40, 1347–1356, https://doi.org/10.1016/j.clinthera.2018.06.009 (2018).
Feng, Z., Chu, F., Guo, Z. & Sun, P. Synthesis and anti-inflammatory activity of the major metabolites of imrecoxib. Bioorganic & medicinal chemistry letters 19, 2270–2272, https://doi.org/10.1016/j.bmcl.2009.02.090 (2009).
Guo, Z. Discovery of Imrecoxib. Chinese Journal of New Drugs 21(3) (2012).
Xu, H. et al. Metabolism and excretion of imrecoxib in rat. Xenobiotica; the fate of foreign compounds in biological systems 36, 441–455, https://doi.org/10.1080/00498250600595524 (2006).
Malone, D. C. et al. Assessment of potential drug-drug interactions with a prescription claims database. American journal of health-system pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists 62, 1983–1991, https://doi.org/10.2146/ajhp040567 (2005).
Krishna, R. et al. Lack of a meaningful effect of anacetrapib on the pharmacokinetics and pharmacodynamics of warfarin in healthy subjects. British journal of clinical pharmacology 74, 116–124, https://doi.org/10.1111/j.1365-2125.2012.04171.x (2012).
Schwartz, J. I. et al. The effect of rofecoxib on the pharmacodynamics and pharmcokinetics of warfarin. Clinical pharmacology and therapeutics 68, 626–636, https://doi.org/10.1067/mcp.2000.112244 (2000).
Gagne, J. J., Maio, V. & Rabinowitz, C. Prevalence and predictors of potential drug-drug interactions in Regione Emilia-Romagna, Italy. Journal of clinical pharmacy and therapeutics 33, 141–151, https://doi.org/10.1111/j.1365-2710.2007.00891.x (2008).
Schafer, A. I. Effects of nonsteroidal antiinflammatory drugs on platelet function and systemic hemostasis. Journal of clinical pharmacology 35, 209–219 (1995).
Langman, M. J. et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet 343, 1075–1078 (1994).
Jonsson, A. K., Spigset, O., Jacobsson, I. & Hagg, S. Cerebral haemorrhage induced by warfarin - the influence of drug-drug interactions. Pharmacoepidemiology and drug safety 16, 309–315, https://doi.org/10.1002/pds.1291 (2007).
Diana, F. J., Veronich, K. & Kapoor, A. L. Binding of nonsteroidal anti-inflammatory agents and their effect on binding of racemic warfarin and its enantiomers to human serum albumin. Journal of pharmaceutical sciences 78, 195–199 (1989).
van Dijk, K. N. et al. Potential interaction between acenocoumarol and diclofenac, naproxen and ibuprofen and role of CYP2C9 genotype. Thrombosis and haemostasis 91, 95–101, https://doi.org/10.1160/TH03-05-0325 (2004).
Delaney, J. A., Opatrny, L., Brophy, J. M. & Suissa, S. Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. CMAJ: Canadian Medical Association journal=journal de l’Association medicale canadienne 177, 347–351, https://doi.org/10.1503/cmaj.070186 (2007).
Geba, G. P. et al. Efficacy of rofecoxib, celecoxib, and acetaminophen in osteoarthritis of the knee: a randomized trial. Jama 287, 64–71 (2002).
Dogne, J. M., Supuran, C. T. & Pratico, D. Adverse cardiovascular effects of the coxibs. Journal of medicinal chemistry 48, 2251–2257, https://doi.org/10.1021/jm0402059 (2005).
Solomon, D. H. Selective cyclooxygenase 2 inhibitors and cardiovascular events. Arthritis and rheumatism 52, 1968–1978, https://doi.org/10.1002/art.21132 (2005).
Tacconelli, S., Capone, M. L. & Patrignani, P. Clinical pharmacology of novel selective COX-2 inhibitors. Current pharmaceutical design 10, 589–601 (2004).
Jaffer, A. & Bragg, L. Practical tips for warfarin dosing and monitoring. Cleveland Clinic journal of medicine 70, 361–371 (2003).
European Medicines Agency. ICH Topic E 6 (R1): Guideline for Good Clinical Practice. Note for guidance on good clinical practice, http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002874.pdf (last accessed on 30 October 2010).
World Medical Association Declaration of Helsinki – ethical principles for medical research involving human subjects, http://www.wma.net/en/30publications/10policies/b3/index.html (last accessed on Octorber 2013).
China Food and Drug Administration Good clinical practice guideline, http://www.sda.gov.cn/WS01/CL0053/24473.html (last accessed on 30 October 2010).
Administration, C. F. a. D. Technical Guidelines for Clinical Pharmacokinetic Study of Chemical Drugs, http://samr.cfda.gov.cn/WS01/CL1616/83420.html (2005).
Liu, Y. et al. Safety, tolerability, pharmacokinetics and pharmacodynamics of recombinant human parathyroid hormone after single- and multiple-dose subcutaneous administration in healthy Chinese volunteers. Basic & clinical pharmacology & toxicology 110, 154–161, https://doi.org/10.1111/j.1742-7843.2011.00768.x (2012).
Frymoyer, A. et al. Effect of single-dose rifampin on the pharmacokinetics of warfarin in healthy volunteers. Clinical pharmacology and therapeutics 88, 540–547, https://doi.org/10.1038/clpt.2010.142 (2010).
Li, S. et al. The strategy for establishment of the multiple reaction monitoring based characteristic chemical profile of triterpenes in Alismatis rhizoma using two combined tandem mass spectrometers. Journal of chromatography. A 1524, 121–134, https://doi.org/10.1016/j.chroma.2017.09.057 (2017).
Zhou, Y. et al. Pharmacokinetics and tolerability of minodronic acid tablets in healthy Chinese subjects and food and age effects on the pharmacokinetics. Clinical therapeutics 37, 869–876, https://doi.org/10.1016/j.clinthera.2015.01.015 (2015).
Tinsley, J., Robinson, N. & Davies, K. E. Safety, tolerability, and pharmacokinetics of SMT C1100, a 2-arylbenzoxazole utrophin modulator, following single- and multiple-dose administration to healthy male adult volunteers. Journal of clinical pharmacology 55, 698–707, https://doi.org/10.1002/jcph.468 (2015).
Yang, L., Meng, X., Yu, X. & Kuang, H. Simultaneous determination of anemoside B4, phellodendrine, berberine, palmatine, obakunone, esculin, esculetin in rat plasma by UPLC-ESI-MS/MS and its application to a comparative pharmacokinetic study in normal and ulcerative colitis rats. Journal of pharmaceutical and biomedical analysis 134, 43–52, https://doi.org/10.1016/j.jpba.2016.11.021 (2017).
Li, C. Y. et al. Pharmacokinetic profiles of hydroxysafflor yellow A following intravenous administration of its pure preparations in healthy Chinese volunteers. Journal of ethnopharmacology 162, 225–230, https://doi.org/10.1016/j.jep.2014.12.068 (2015).
Karlsson, M. et al. Plasma fibrinogen level, bleeding, and transfusion after on-pump coronary artery bypass grafting surgery: a prospective observational study. Transfusion 48, 2152–2158, https://doi.org/10.1111/j.1537-2995.2008.01827.x (2008).
Scott, G. et al. Lack of effect of omeprazole or of an aluminium hydroxide/magnesium hydroxide antacid on the pharmacokinetics of lumiracoxib. Clinical pharmacokinetics 43, 341–348, https://doi.org/10.2165/00003088-200443050-00006 (2004).
Zhao, L. et al. Safety, tolerability and pharmacokinetics of phenoprolamine hydrochloride floating sustained-release tablets in healthy Chinese subjects. International journal of pharmaceutics 377, 99–104, https://doi.org/10.1016/j.ijpharm.2009.05.010 (2009).
Liu, Y. et al. Bioequivalence and pharmacokinetic evaluation of two formulations of glimepiride 2 mg: a single-dose, randomized-sequence, open-label, two-way crossover study in healthy Chinese male volunteers. Clinical therapeutics 32, 986–995, https://doi.org/10.1016/j.clinthera.2010.04.016 (2010).
Stockis, A., van Lier, J. J., Cawello, W., Kumke, T. & Eckhardt, K. Lack of effect of lacosamide on the pharmacokinetic and pharmacodynamic profiles of warfarin. Epilepsia 54, 1161–1166, https://doi.org/10.1111/epi.12192 (2013).
Gao, G. M. et al. The Efficacy of Imrecoxib and Celecoxib in Axial Spondyloarthritis and Their Influence on Serum Dickopff-Related Protein 1 (DKK-1) Levels. Medical science monitor: international medical journal of experimental and clinical research 23, 2985–2992 (2017).
Linder, J. D., Monkemuller, K. E., Davis, J. V. & Wilcox, C. M. Cyclooxygenase-2 inhibitor celecoxib: a possible cause of gastropathy and hypoprothrombinemia. Southern medical journal 93, 930–932 (2000).
Stading, J. A., Skrabal, M. Z. & Faulkner, M. A. Seven cases of interaction between warfarin and cyclooxygenase-2 inhibitors. American journal of health-system pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists 58, 2076–2080 (2001).
Haase, K. K., Rojas-Fernandez, C. H., Lane, L. & Frank, D. A. Potential interaction between celecoxib and warfarin. The Annals of pharmacotherapy 34, 666–667, https://doi.org/10.1345/aph.19324 (2000).
Mersfelder, T. L. & Stewart, L. R. Warfarin and celecoxib interaction. The Annals of pharmacotherapy 34, 325–327, https://doi.org/10.1345/aph.19246 (2000).
Ansell, J. et al. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126, 204S–233S, https://doi.org/10.1378/chest.126.3_suppl.204S (2004).
Gaikwad, T. et al. Influence of CYP2C9 and VKORC1 gene polymorphisms on warfarin dosage, over anticoagulation and other adverse outcomes in Indian population. European journal of pharmacology 710, 80–84, https://doi.org/10.1016/j.ejphar.2013.04.006 (2013).
Wu, S. et al. Warfarin and vitamin K epoxide reductase: a molecular accounting for observed inhibition. Blood 132, 647–657, https://doi.org/10.1182/blood-2018-01-830901 (2018).
Veenstra, D. L. et al. Association of Vitamin K epoxide reductase complex 1 (VKORC1) variants with warfarin dose in a Hong Kong Chinese patient population. Pharmacogenetics and genomics 15, 687–691 (2005).
Carlquist, J. F. et al. Genotypes of the cytochrome p450 isoform, CYP2C9, and the vitamin K epoxide reductase complex subunit 1 conjointly determine stable warfarin dose: a prospective study. Journal of thrombosis and thrombolysis 22, 191–197, https://doi.org/10.1007/s11239-006-9030-7 (2006).
Wadelius, M. et al. The largest prospective warfarin-treated cohort supports genetic forecasting. Blood 113, 784–792, https://doi.org/10.1182/blood-2008-04-149070 (2009).
Bodin, L. et al. Cytochrome P450 2C9 (CYP2C9) and vitamin K epoxide reductase (VKORC1) genotypes as determinants of acenocoumarol sensitivity. Blood 106, 135–140, https://doi.org/10.1182/blood-2005-01-0341 (2005).
Vecsler, M. et al. Combined genetic profiles of components and regulators of the vitamin K-dependent gamma-carboxylation system affect individual sensitivity to warfarin. Thrombosis and haemostasis 95, 205–211, https://doi.org/10.1160/TH05-06-0446 (2006).
Liang, R. et al. Impact of CYP2C9*3, VKORC1-1639, CYP4F2rs2108622 genetic polymorphism and clinical factors on warfarin maintenance dose in Han-Chinese patients. Journal of thrombosis and thrombolysis 34, 120–125, https://doi.org/10.1007/s11239-012-0725-7 (2012).
Li, S. et al. Warfarin dosage response related pharmacogenetics in Chinese population. PloS one 10, e0116463, https://doi.org/10.1371/journal.pone.0116463 (2015).
Yang, L., Ge, W., Yu, F. & Zhu, H. Impact of VKORC1 gene polymorphism on interindividual and interethnic warfarin dosage requirement–a systematic review and meta analysis. Thrombosis research 125, e159–166, https://doi.org/10.1016/j.thromres.2009.10.017 (2010).
Singh, O., Sandanaraj, E., Subramanian, K., Lee, L. H. & Chowbay, B. Influence of CYP4F2 rs2108622 (V433M) on warfarin dose requirement in Asian patients. Drug metabolism and pharmacokinetics 26, 130–136 (2011).
Miao, L., Yang, J., Huang, C. & Shen, Z. Contribution of age, body weight, and CYP2C9 and VKORC1 genotype to the anticoagulant response to warfarin: proposal for a new dosing regimen in Chinese patients. European journal of clinical pharmacology 63, 1135–1141, https://doi.org/10.1007/s00228-007-0381-6 (2007).
Wang, T. L. et al. Genetic factors contribute to patient-specific warfarin dose for Han Chinese. Clinica chimica acta; international journal of clinical chemistry 396, 76–79, https://doi.org/10.1016/j.cca.2008.07.005 (2008).
Shepherd, A. M., Hewick, D. S., Moreland, T. A. & Stevenson, I. H. Age as a determinant of sensitivity to warfarin. British journal of clinical pharmacology 4, 315–320, https://doi.org/10.1111/j.1365-2125.1977.tb00719.x (1977).
Jensen, B. P., Chin, P. K., Roberts, R. L. & Begg, E. J. Influence of adult age on the total and free clearance and protein binding of (R)- and (S)-warfarin. British journal of clinical pharmacology 74, 797–805, https://doi.org/10.1111/j.1365-2125.2012.04259.x (2012).
Abe, J. et al. Evaluation of Dabigatran- and Warfarin-Associated Hemorrhagic Events Using the FDA-Adverse Event Reporting System Database Stratified by Age. International journal of medical sciences 12, 312–321, https://doi.org/10.7150/ijms.10703 (2015).
Ragueneau-Majlessi, I., Levy, R. H. & Meyerhoff, C. Lack of effect of repeated administration of levetiracetam on the pharmacodynamic and pharmacokinetic profiles of warfarin. Epilepsy research 47, 55–63 (2001).
Oberwittler, H. et al. Significant pharmacokinetic and pharmacodynamic interaction of warfarin with the NO-independent sGC activator HMR1766. Journal of clinical pharmacology 47, 70–77, https://doi.org/10.1177/0091270006294540 (2007).
Yin, O. Q. et al. Effects of nilotinib on single-dose warfarin pharmacokinetics and pharmacodynamics: a randomized, single-blind, two-period crossover study in healthy subjects. Clinical drug investigation 31, 169–179, https://doi.org/10.2165/11538700-000000000-00000 (2011).
Schaefer, M. G., Plowman, B. K., Morreale, A. P. & Egan, M. Interaction of rofecoxib and celecoxib with warfarin. American journal of health-system pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists 60, 1319–1323 (2003).
Searle, G. D. Celecoxib package insert. Skokie, IL (2002 Jun).
Gong, L. et al. Celecoxib pathways: pharmacokinetics and pharmacodynamics. Pharmacogenetics and genomics 22, 310–318, https://doi.org/10.1097/FPC.0b013e32834f94cb (2012).
Washington, C., Hou, S. Y., Hughes, N. C., Campanella, C. & Berner, B. Ciprofloxacin prolonged-release tablets do not affect warfarin pharmacokinetics and pharmacodynamics. Journal of clinical pharmacology 47, 1320–1326, https://doi.org/10.1177/0091270007305504 (2007).
Acknowledgements
This work was supported by National Natural Science Foundation of China (81874326, 81503161), Chinese Medicine Research Progect of Health Commission of Hubei Province (ZY2019Z004); National Key R&D Program of China (2017YFC0909900) and Jiangsu Heng Rui Medicine Co. Ltd, Jiangsu, China. Thank Dr. Dafang Zhong’s group for completing sample analyzed. Thank you to all the volunteers participating in this trial.
Author information
Authors and Affiliations
Contributions
Yani Liu, Rui Zhang, Yu Zhang and Shaojun Shi conceived and designed the study. Yani Liu, Zhongfang Li, Jiali Zhou, Tingyu Yang, Chunxiao Yang, Xixi Huang and Shaojun Shi conducted trial. All authors wrote, corrected and read the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Y., Zhang, R., Li, Z. et al. Lack of effect of Imrecoxib, an innovative and moderate COX-2 inhibitor, on pharmacokinetics and pharmacodynamics of warfarin in healthy volunteers. Sci Rep 9, 15774 (2019). https://doi.org/10.1038/s41598-019-51755-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51755-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.