Abstract
Background and Aims
Dyspepsia is frequently encountered by primary care providers (PCP) and gastroenterologists (GI). While esophagogastroduodenoscopy (EGD) may be useful, current guidelines suggest a proton pump inhibitor (PPI) trial and H. pylori (HP) test-and-treat before EGD for low-risk patients. This study aimed to evaluate pre-EGD management and endoscopic outcomes in this population.
Methods
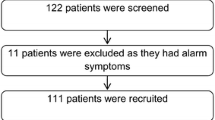
This was a retrospective cohort study of low-risk dyspepsia patients (age ≤55, no alarm features) undergoing EGD at an ambulatory endoscopy center from January 2011 to March 2012. Adherences to initial management guidelines (PPI trial and HP test-and-treat strategy before EGD) were compared between PCP and GI. Endoscopic and pathologic outcomes were assessed for all patients. Statistical analyses were performed using Chi-squared test (categorical variables) and Student’s t test (continuous variables). This study received IRB approval (2011P001715).
Results
A total of 309 low-risk patients underwent EGD for dyspepsia. Only 202 (65.4 %) had HP testing, and 220 (71.2 %) were trialed on any dose/length PPI pre-EGD, with no differences between PCP and GI. PPI exposure was similar between groups for all dose/duration except for trials ≥8 weeks of any dose (46.9 % GI vs 34.3 % PCP, p = 0.03) and high dose (32 % GI vs 18.7 % PCP, p = 0.01). Overall, only 178 (57.6 %) patients had both HP testing and any PPI exposure pre-EGD (56.6 % GI vs 59 % PCP, p = 0.73). Significant pathology was rare, with gastritis (46.6 %) and HP (17.2 %) being most common. No malignancy was found.
Conclusions
A significant proportion of low-risk dyspepsia patients did not receive any PPI trial or HP testing before EGD. Within this population, significant finding on EGD was rare, supporting the current noninvasive initial management guidelines for dyspepsia.


Similar content being viewed by others
References
Piessevaux H, De Winter B, Louis E, et al. Dyspeptic symptoms in the general population: a factor and cluster analysis of symptom groupings. Neurogastroenterol Motil. 2009;21:378–388.
Shaib Y, El-Serag HB. The prevalence and risk factors of functional dyspepsia in a multiethnic population in the United States. Am J Gastroenterol. 2004;99:2210–2216.
Russo M, Wei J, Thiny M, et al. Digestive and liver diseases statistics, 2004. Gastroenterology. 2004;126:1448–1453.
Tack J, Talley N, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479.
Fransen GAJ, Janssen MJR, Muris JWM, et al. Meta-analysis: the diagnostic value of alarm symptoms for upper gastrointestinal malignancy. Aliment Pharmacol Ther. 2004;20:1045–1052.
Wai C, Yeoh K, Ho K, et al. Diagnostic yield of upper endoscopy in Asian patients presenting with dyspepsia. Gastrointest Endosc. 2002;56:548–551.
Vakil N, Moayyedi P, Fennerty M, et al. Limited value of alarm features in the diagnosis of upper gastrointestinal malignancy: systematic review and meta-analysis. Gastroenterology. 2006;131:390–401.
Ikenberry S, Harrison M, Lichtenstein D, the ASGE Standards of Practice Committee. The role of endoscopy in dyspepsia. Gastrointest Endosc. 2007;66:1071–1075.
Talley NJ. American Gastroenterological Association medical position statement: evaluation of dyspepsia. Gastroenterology. 2005;129:1753–1755.
Talley NJ, Vakil N, Practice Parameters Committee of the American College of Gastroenterology. Guidelines for the management of dyspepsia. Am J Gastroenterol. 2005;100:2324–2337.
Salo M, Collin P, Kyronpalo S, et al. Age, symptoms and upper gastrointestinal malignancy in primary care endoscopy. Scand J Gastroenterol. 2008;43:122–127.
Bai Y, Li ZS, Zou DW, et al. Alarm features and age for predicting upper gastrointestinal malignancy in Chinese patients with dyspepsia with high background prevalence of Helicobacter pylori infection and upper gastrointestinal malignancy: an endoscopic database review of 102,665 patients from 1996 to 2006. Gut. 2010;59:722–728.
Bowrey DJ, Griffin SM, Wayman J, et al. Use of alarm symptoms to select dyspeptics for endoscopy causes patients with curable esophagogastric cancer to be overlooked. Surg Endosc. 2006;20:1725–1728.
Choi J, Kim SG, Im JP, et al. Long-term clinical outcomes of endoscopic resection for early gastric cancer. Surg Endosc. 2015;29:1223–1230.
Kavic SM, Basson MD. Complications of endoscopy. Am J Surg. 2001;181:319–332.
Lacy BE, Weiser KT, Kennedy AT, et al. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38:170–177.
Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975–2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
Mahadeva S, Goh K-L. Epidemiology of functional dyspepsia: a global perspective. World J Gastroenterol. 2006;12:2661–2666.
Charles RJ, Cooper GS, Wong RC, et al. Effectiveness of open-access endoscopy in routine primary-care practice. Gastrointest Endosc. 2003;57:183–186.
Wang WH, Huang JQ, Zheng GF, et al. Effects of proton-pump inhibitors on functional dyspepsia: a meta-analysis of randomized placebo-controlled trials. Clin Gastroenterol Hepatol. 2007;5:178–185.
Hirota WK, Zuckerman MJ, Adler DG, et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570–580.
Miwa H, Ghoshal UC, Gonlachanvit S, et al. Asian consensus report on functional dyspepsia. J Neurogastroenterol Motil. 2012;18:150–168.
Author contributions
J.P.F. and W.W.C. contributed to study conception and design. J.P.F., A.M.T., and W.W.C. contributed to data acquisition, analysis and interpretation, manuscript drafting, and critical revisions for intellectual content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not report any conflict of interests and have no financial disclosures relevant to the subjects of the manuscript.
Rights and permissions
About this article
Cite this article
Fiorenza, J.P., Tinianow, A.M. & Chan, W.W. The Initial Management and Endoscopic Outcomes of Dyspepsia in a Low-Risk Patient Population. Dig Dis Sci 61, 2942–2948 (2016). https://doi.org/10.1007/s10620-016-4051-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4051-3