Abstract
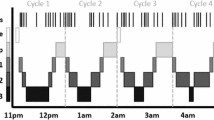
Too much noise disturbs sleep, as well known. The number of persons affected by community noise is estimated to be huge. This paper summarizes the recommendation by WHO (1999) and the following international documents, and introduce new data and debate. First, we should choose noise descriptors to study and to regulate noise-induced sleeplessness taking account of (1) whether we want to focus on continuous noise or intermittent noise, and (2) whether we want to focus on noise prediction or ecological measurement. L Aeq (A-weighted sound equivalent level) at sleep period well predicts sleep disturbance in general. Since intermittent noise is more likely to disturb sleep than continuous noise, even if their L Aeq is the same, L Amax and L AE are also used. Second, we should determine sleep descriptors such as EEG, actigraphy, and questionnaires. The descriptors should be chosen, in consideration of burdens to subjects and time-scale that should be matched with noise assessment. Based on the dose–response relationship between community noise and sleep disturbance, WHO (1999) recommended that indoor sound level should be L Aeq of 35 dB or below for the general population from the aspect of health sciences. WHO Regional Office for Europe (2004), however, proposed much more strict guidelines, taking the recent studies on community noise and cardiovascular diseases in the general population. Most of the data were, however, cross-sectionally obtained, and causality cannot be determined. As a result, intensive debate emerged whether or not the reported effects are meaningful and all the effects are impermissible, reflecting the difference between European view of health and US pragmatic position. On the other hand, effects of ultra-low-frequency sound from wind turbine plants on sleep and health seem negligible, although audible noise from wind turbine can disturb sleep among residents. Individual difference in sensitivity to noise and effects of daytime noise on night/shift-workers should be further investigated. If they can be clarified, this should be systematically reflected to the exposure assessment.
Similar content being viewed by others
References
WHO. Guidelines for community noise. Geneva: WHO; 1999.
Stansfeld SA, Matheson MP. Noise pollution: non-auditory effects on health. Br Med Bull. 2003;68:243–57.
WHO Regional Office for Europe. Night Noise Guidelines for Europe. WHO Regional Office for Europe, Copenhagen. 2009. http://www.euro.who.int/__data/assets/pdf_file/0017/43316/E92845.pdf. Accessed 1 June 2016.
Working Group on Health and Socio-Economic Aspects, EU. Position paper on dose-effect relationships for night time noise. EU, Brussels. 2004. http://www.moa.gov.cy/moa/environment/environment.nsf/77543A500D533CA4C2257991003D8793/$file/Dose-Effect%20Relationships%20for%20Night%20Time%20Noise.pdf. Accessed 1 June 2016.
Pearsons KS, Barber DS, Tabachnick BG. Analyses of the predictability of noise-induced sleep disturbance. USAF Report HSD-TR-89-029. 1989.
Kempen EEMM, Kruize H, Boshuizen HC, Ameling CB, Staatsen BAM, Hollander AEM. The association between noise exposure and blood pressure and ischemic heart disease: a meta-analysis. Environ Health Perspect. 2002;110:307–17.
WHO Regional Office for Europe, European Centre for Environment and Health. WHO Technical Meeting on Sleep and Health. WHO Regional Office for Europe, Bonn. 2004. http://www.euro.who.int/__data/assets/pdf_file/0008/114101/E84683.pdf. Accessed 1 June 2016.
Knopper LD, Ollson CA. Health effects and wind turbines: a review of the literature. Environ Health. 2011;10:78–87.
Schmidt GH, Klokker M. Health effects related to wind turbine noise exposure: a systematic review. PLoS ONE. 2014;9(12):e114183. doi:10.1371/journal.pone.0114183.
Kishikawa H, Matsui T, Uchiyama I, Miyakawa M, Hiramatsu K, Stansfeld SA. Noise sensitivity and subjective health: questionnaire study conducted along trunk roads in Kusatsu. Japan. Noise Health. 2009;11(43):111–7.
Kageyama T, Yano T, Kuwano S, Sueoka S. Exposure-response relationship of wind turbine noise with self-reported symptoms of sleep and health problems: a nationwide socioacoustic survey in Japan. Noise Health. 2016;18:53–61.
Griefahn B. Models to determine critical loads for nocturnal noise. Proc. of the 6th International Congress on Noise as Public Health Problem, 1993; 367–72.
Kuno K, Hayashi A, Ikegaya K, Mishina Y. Some aspects of sound exposure during sleep in daily life. J Acoustic Soc Jpn. 1981;37:141–9.
Kageyama T, Kabuto M. Individual sound exposure level during sleep in relation to road traffic noise in the Greater Tokyo Metropolitan area. Noise Control Eng Jpn. 1992;16(5):42–6.
Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73.
American Academy of Sleep Medicine. The international classification of sleep disorders, diagnostic and coding manual. 2nd ed. NY: Westchester; 2005.
Vallet M, Gagneux JM, Blanchet V, Favre B, Labiale G. Long term sleep disturbance due to traffic noise. J Sound Vibr. 1983;90:173–91.
Thiessen GJ, Lapointe AC. Effect of continuous traffic noise on percentage of deep sleep, waking, and sleep latency. J Acoustic Soc Am. 1983;73:225–9.
Eberhardt JL, Akselsson KR. The disturbance by road traffic noise of the sleep of young male adults as recorded in home. J Sound Vibration. 1987;114:417–34.
Eberhardt JL, Stråle LO, Berlin MH. The influence of continuous and intermittent traffic noise on sleep. J Sound Vibration. 1987;116:445–64.
Griefahn B. A critical load for nocturnal high-density road traffic noise. Am J Ind Med. 1986;9:261–9.
Rosenthal L, Bishop C, Helmus T, Krstevska S, Roehrs T, Roth T. Auditory awakening thresholds in sleepy and alert individuals. Sleep. 1996;19:290–5.
Prasher D. Is there evidence that environmental noise is immunotoxic? Noise Health. 2009;11(44):151–5.
Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15:461–9.
Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92.
Horne JA, Pankhurst FL, Reyner LA, Hume K, Diamond ID. A field of sleep disturbance: effects of aircraft noise and other factors on 5742 night of actimetrically monitored sleep in a large subject sample. Sleep. 1994;17:146–59.
Miedema HME, Passchier-Vermeer W, Vos H. Elements for a position paper on night-time transportation noise and sleep disturbance. Delft: TNO Inro; 2003. p. 2002–59.
Graham JM, Janssen SA, Vos H, Miedema HM. Habitual traffic noise at home reduces cardiac parasympathetic tone during sleep. Int J Psychophysiol. 2009;72:179–86.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5.
Kaku J, Kabuto M, Kageyama T, Kuno K, Kuwano S, Namba S, Seoka H, Tachibana H, Yamamoto Y, Yamashita M, Kamigawara K. Standardization of social survey method in Japan. Proceedings of Inter-Noise 2004; 2004.
Kageyama T, Kabuto M, Nitta H, Kurokawa Y, Taira K, Suzuki S, Takemoto T. A population study on risk factors for insomnia among adult Japanese women: a possible effect of road traffic volume. Sleep. 1997;20:963–71.
Sasazawa Y, Kawada T, Kiryu Y, Suzuki S. The relationship between traffic noise and insomnia among adult Japanese women. J Sound Vibr. 2004;277:547–57.
Öhrström E, Skånberg A. Sleep disturbance by road traffic noise—a laboratory study on number of noise events. J Sound Vibr. 1987;116:445–64.
Ohrstrom E. (1993) Effects of low levels from road traffic noise during night—a laboratory study on number of events, maximum noise levels and noise sensitivity. M. Vallet (Eds.): Proc. the 6th International Congress on Noise as Public Health Problem 359-66. INRETS, France.
Fidell S, Pearsons K, Tabachnick BG, Howe R. Effects on sleep disturbance of changes in aircraft noise near three airports. J Acoust Soc Am. 2000;107(5 Pt 1):2535–47.
Passcheir-Vermeer W, Vos H, Steenbekkers JHM, Van der Ploeg FD, Groothuis-Oudshoorn K. Sleep disturbance and aircraft noise exposure: Exposure-effect relationships. TNO Inro Report No. 2002.027; 2002.
Passcheir-Vermeer W. (2003) Night-time noise events and awakening. TNO Inro Report No. 2003-32.
Basner M, Samel A, Isermann U. Aircraft noise effects on sleep: application of the results of a large polysomnographic field study. J Acoust Soc Am. 2006;119:2772–84.
Hong J, Lim C, Kim J, Lee S. Assessment of sleep disturbance on night-time railway noise from field survey. Inter-Noise 2006.
Hume KI, Brinl M, Basner M. Effects of environmental noise on sleep. Noise Health. 2012;14(61):297–302.
Babisch W, Ising H, Kruppa B, Wiens D. (1992) Verkehrslärm und Herzinfarkt, Ergebnisse zweier Fall-Kontroll-Studien in Berlin. WaBoLu-Hefte 2/92. Berlin: Institut für Wasser-, Boden- und Lufthygiene, Umweltbundesamt.
Babisch W, Ising H, Kruppa B, Wiens D. The incidence of myocardial infarction and its relation to road traffic noise—the Berlin case-control studies. Environ Int. 1994;20:469–74.
Babisch W, Ising H, Gallacher JEJ, Sweetnam PM, Elwood PC. Traffic noise and cardiovascular risk: the Caerphilly and Speedwell studies, third phase—10 years followup. Arch Environ Health. 1999;54:210–6.
Babisch W, Ising H, Gallacher JEJ. Health status as a potential effect modifier of the relation between noise annoyance and incidence of ischaemic heart disease. Occup Environ Med. 2003;60:739–45.
Babisch W, Beule B, Schust M, Stark H. Traffic noise and myocardial infarction. Results from the NaRoMI Study (Noise and Risk of Myocardial Infarction). In: Jong Rd, Houtgast T, Franssen EAM, Hofman W, editors. ICBEN 2003. Proceedings of the 8th International Congress on Noise as a Public Health Problem, Rotterdam, ISBN 90-807990-1-7. Schiedam: Foundation ICBEN 2003, 96–101; 2003.
Babisch W. The NaRoMI-Study: Executive summary—traffic noise. In: Federal Environmental Agency (Umweltbundesamt), editor. Chronic noise as a risk factor for myocardial infarction, The NaRoMI study (major technical report). WaBoLu-Hefte 02/04. Berlin: Umweltbundesamt. pp. I-1 to I-59; 2004.
Babisch W, Beule B, Schust M, Kersten N, Ising H. Traffic noise and risk of myocardial infarction. Epidemiology. 2005;16:33–40.
Lercher P, Widmann U, Kofler W (2000) Transportation noise and bold pressure: the importance of midifying factors. In Cassereau D (eds.) Internoise; Nice.
Dratva J, Phuleria HC, Foraster M, Graspoz JM, Leidel D, Künzli N, Liu LJ, Pons M, Zemp E, Gerbase MW, Schindler C. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect. 2011;120:50–5.
Tachibana H, Yano H, Fukushima A, Sueoka S. Nationwide field measurements of wind turbine noise in Japan. Noise Control Eng J. 2014;62:90–101.
Schmidt GH, Klokker M. Health effects related to wind turbine noise exposure: a systematic review. PLoS One. 2014;9(12):e114183. doi:10.1371/journal.pone.0114183.
Pedersen E, Waye KP. Perception and annoyance due to wind turbine noise—a dose-response relationship. J Acoust Soc Am. 2004;116:3460–70.
Shepherd D, McBride D, Welch D, Dirks KM, Hill EM. Evaluating the impact of wind turbine noise on health-related quality of life. Noise Health. 2011;13(54):333–9.
Bakker RH, Pedersen E, van den Berg GP, Stewart RE, Lok W, Bouma J. Impact of wind turbine sound on annoyance, self-reported sleep disturbance and psychological distress. Sci Total Environ. 2012;425:42–51.
Pedersen E. Health aspects associated with wind turbine noise—results from three field studies. Noise Control Eng J. 2011;59:47–53.
Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet. 2007;369:946–55. doi:10.1016/s0140-6736(07)60159-7.
Herbert S, Carrier J. Sleep complaints in elderly tinnitus patients: a controlled study. Ear Hear. 2007;28:649–55.
Åkerstedt T, Kenneth PWJ. Sleep loss and fatigue in shiftwork and shiftwork disorder. Sleep Med Clin. 2009;4:257–71.
Kageyama T, Kobayashi T, Nishikido N, Kawashima M. Sound environment during sleep periods of shift workers: management of sound level in apartment houses for hospital nurses. Proceedings of 2000 Meeting/Institute of Noise Control Engineering Japan. 2000; 197–200.
Perron S, Tétreault LF, King N, Plante C, Smargiassi A. Review of the effect of noise on sleep disturbance in adults. Noise Health. 2012;14(57):58–67.
Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi-airport retrospective study. Br Med J. 2013;347:f5561.
Halonen JI, Hansell AL, Gulliver J, Morley D, Blangiardo M, Fecht D, Toledano MB, Beevers SD, Anderson HR, Kelly FJ, Tonne C. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur Heart J. 2015;36:2653–61.
Evrard AS, Bouaoun L, Champelovier P, Lambert J, Laumon B. Does exposure to aircraft noise increase the mortality from cardiovascular disease in the population living in the vicinity of airports? Results of an ecological study in France. Noise Health. 2015;17(78):328–36.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kageyama, T. Adverse effects of community noise as a public health issue. Sleep Biol. Rhythms 14, 223–229 (2016). https://doi.org/10.1007/s41105-016-0069-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-016-0069-3