Abstract
Alzheimer’s disease (AD) is a serious public health issue, and a treatment for the disease has been elusive. Evolutionary approaches to medicine may contribute to understanding why humans are vulnerable to AD and how to best approach research into clinical interventions. Since AD generally manifests late in life, it is often thought to be invisible to natural selection; however, an examination into APOE, the only unequivocal risk gene for AD, reveals that AD may, in fact, be subject to selection. Given this, antagonistic pleiotropy and environmental mismatch are explored as possibilities for our vulnerability to AD. In addition, the amyloid-β (Aβ) plaques and paired helical filament tau (PHFtau) neurofibrillary tangles that characterize AD are considered from the perspective of evolution. These disease hallmarks are generally thought to promote neurodegeneration in AD, but may in fact be harmless by-products of a pathological process such as oxidative stress, or even beneficial adaptations to protect the brain from actual harmful processes. The spread of misfolded Aβ and synaptic propagation of PHFtau is considered, as are comparative perspectives on AD-like patterns in nonhuman species. The implications of evolutionary thinking for clinical practice and research are evaluated, especially with regard to the caution that must be taken when directly targeting tau and amyloid, as many drug trials have recently attempted.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Thies W, Bleiler L (2013) Alzheimer’s disease facts and figures. Alzheimer’s Dement 9(2):208–245
Brookmeyer R, Johnson E, Zeigler-Graham K, Arrighi HM (2007) Forecasting the global burden of Alzheimer’s disease. Alzheimer’s Dement 3(3):186–191
Kalaria RN, Maestre GE, Arizaga R, Friedland RP, Galasko D, Hall K, Luchsinger JA, Ogunniyi A, Perry EK, Potocnik F, Prince M, Stewart R, Wilmo A, Zhang Z-X, Antuono P (2008) Alzheimer’s disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet 7(9):812–826
Keller MC, Miller G (2006) Resolving the paradox of common, harmful, heritable metal disorders: Which evolutionary model works best? Behav Brain Sci 29:385–452
Charlesworth B (1996) Evolution of senescence: Alzheimer’s disease and evolution. Curr Biol 6(1):20–22. doi:10.1016/S0960-9822(02)00411-6
Stearns SC, Nesse RM, Govindaraju DR, Ellison PT (2010) Evolutionary perspectives on health and medicine. Proc Natl Acad Sci 107(suppl 1):1691–1695. doi:10.1073/pnas.0914475107
Saunders AM, Strittmatter WJ, Schmechel D, George-Hyslop PHS, Pericak-Vance MA, Joo SH, Rosi BL, Gusella JF, Crapper-MacLachan DR, Alberts MJ et al (1993) Association of apolipoprotein E allele epsilon 4 with late-onset familial and sporadic Alzheimer’s disease. Neurology 43:1467–1472
Corder EH, Saunders AM, Strittmatter WJ, Schmechel D, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261(5123):921–923
Katzel LI, Fleg JL, Paidi M, Ragoobarsingh N, Goldberg AP (1993) ApoE4 polymorphism increases the risk for exercise-induced silent myocardial ischemia in older men. Atertio Thromb Vasc Biol 13:1495–1500
Song Y, Stampfer MJ, Liu S (2004) Meta-analysis: apolipoprotein E genotypes and risk for coronary heart disease. Ann Intern Med 141(2):137–147. doi:10.7326/0003-4819-141-2-200407200-00013
Ghebremedhin E, Schultz C, Braak E, Braak H (1998) High frequency of apolipoprotein E epsilon 4 allele in young individuals with very mild Alzheimer’s disease-related neurofibrillary changes. Exp Neurol 153:152–155
Nicoll JA, Roberts GW, Graham DI (1995) Apolipoprotein e epsilon 4 allele is associated with deposition of amloid beta-protein following head injury. Nat Med 1:135–137
Koochmeshgi J, Hosseini-Mazinani SM, Seifati SM, Hosein-Pur-Nobari N, Teimoori-Toolabi L (2004) Apolipoprotein E genotype and age at menopause. Ann NY Acad Sci 1019:564–567
He L-N, Recker RR, Deng H-W, Dvornyk V (2009) A polymorphism of apolipoprotein E (APOE) gene is associated with age at natural menopause in Caucasian females. Maturitas 62:37–41
Hanlon CS, Rubinsztein DC (1995) Arginine residues at codons 112 and 158 in the apolipoprotein E gene correspond to the ancestral state in humans. Atherosclerosis 112(1):85–90
Ashford JW (2002) Apo E4: is it the absence of good or the presence of bad? J Alzheimer’s Dis 4:141–143
Hill JM, Bhattacharjee PS, Neumann DM (2007) Apolipoprotein E alleles can contribute to the pathogenesis of numerous clinical conditions including HSV-1 corneal disease. Exp Eye Res 84:801–811
Sapolsky RM, Finch CE (2000) Alzheimer’s disease and some speculations about the evolution of its modifiers. Ann NY Acad Sci 924:99–103
Lahdenperä M, Russell AF, Tremblay M, Lummaa V (2010) Selection on menopause in two premodern human populations: no evidence for the mother hypothesis. Evolution 65(2):476–489
Cant MA, Johnstone RA (2008) Reproductive conflict and the separation of reproductive generations in humans. PNAS 105(14):5332–5336
Lahdenperä M, Russell AF, Lummaa V (2007) Selection for long lifespan in men: Benefits of grandfathering? Proc R Soc Lond [Biol] 274(1624):2437–2444
Williams GC (1957) Pleiotropy, natural selection, and the evolution of senescence. Evol Dev 11:398–411
Rose MR (1991) The evolutionary biology of aging. Oxford University Press, New York
Martin GM (2002) Gene action in the aging brain: an evolutionary biological perspective. Neurobiol Aging 23:647–654
Zetterberg H, Palmér M, Ricksten A, Poirier J, Palmqvist L, Rymo L, Zafiropoulos A, Arvanitis DA, Spandidos DA, Blennow K (2002) Influence of the apolipoprotein E 14 allele on human embryonic development. Neurosci Lett 324:189–192
Ravaja N, Räikkönen K, Lyytinen H, Lehtimäki T, Keltikangas-Järvinen L (1997) Apolipoprotein E phenotypes and cardiovascular responses to experimentally induced mental stress in adolescent boys. J Behav Med 20(6):571–587
Wozniak MA, Itzhaki RF, Faragher EB, James MW, Ryder SD, Irving WL (2002) Apolipoprotein E-epsilon 4 protects against severe liver disease caused by hepatitis C virus. Hepatology 36(2):456–463
Rusted JM, Evans SL, King SL, Dowell N, Tabet N, Tofts PS (2013) APOE e4 polymorphism in young adults is associated with improved attention and indexed by distinct neural signatures. NeuroImage 65:364–373. doi:10.1016/j.neuroimage.2012.10.010
Bufill E, Blesa R, Agusti J (2013) Alzheimer’s disease: an evolutionary approach. J Anthropol Sci 91:135–157
Reser JE (2009) Alzheimer’s disease and natural cognitive aging may represent adaptive metabolism reduction programs. Behav Brain Funct 5:13
Horn JL, Cattell RB (1967) Age differences in fluid and crystallized intelligence. Acta Psychol (Amst) 26:107–129. doi:10.1016/0001-6918(67)90011-X
Haxby JV, Grady CL, Duara R, Schlageter N, Berg G, Rapoport SI (1986) Neocortical metabolic abnormalities precede nonmemory cognitive defects in early alzheimer’s-type dementia. Arch Neurol 43(9):882–885. doi:10.1001/archneur.1986.00520090022010
Kuusisto J, Koivisto K, Mykkänen L, Helkala E-L, Vanhanen M, Hänninen T, Kervinen K, Kesäniemi YA, Riekkinen PJ, Laakso M (1997) Association between features of the insulin resistance syndrome and Alzheimer’s disease independently of apolipoprotein e4 phenotype: Cross sectional population based study. BMJ 315(7115):1045–1049
Martins IJ, Hone E, Foster JK, Sunram-Lea SI, Gnjec A, Fuller SJ, Nolan D, Gandy SE, Martins RN (2006) Apolipoprotein E, cholesterol metabolism, diabetes, and the convergence of risk factors for Alzheimer’s disease and cardiovascular disease. Mol Psychiatry 11(8):721–736
de la Monte SM (2009) Insulin resistance and Alzheimer’s disease. BMB Reports 42(8):475–481
Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, Fuino RL, Kawaguchi KR, Samoyedny AJ, Wilson RS, Arvanitakis Z, Schneider JA, Wolf BA, Bennett DA, Trojanowski JQ, Arnold SE (2012) Demonstrated brain insulin resistance in Alzheimer’s disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest 122(4):1316–1338
Pontzer H, Raichlen DA, Wood BM, Mabulla AZP, Racette SB, Marlowe FW (2012) Hunter-gatherer energetics and human obesity. PLoS ONE 7(7):e40503
Fox M, Knapp LA, Andrews PW, Fincher CL (2013) Hygiene and the world distribution of Alzheimer’s disease: epidemiological evidence for a relationship between microbial environment and age-adjusted disease burden. Evol Med Publ Health 1:173–186. doi:10.1093/emph/eot015
Karran E, Mercken M, Strooper BD (2011) The amyloid cascade hypothesis for Alzheimer’s disease: an appraisal for the development of therapeutics. Nat Rev Drug Discov 10(9):698–712
Kokjohn TA, Roher AE (2009) Antibody responses, amyloid-beta peptide remnants and clinical effects of AN-1792 immunization in patients with AD in an interrupted trial. CNS Neurol Disord Drug Targets 8(2):88–97
Salloway S, Sperling R, Fox NC, Blennow K, Klunk W, Raskind M, Sabbagh MN, Honig LS, Porsteinsson AP, Ferris S, Reichert M, Ketter N, B. N, Guenzler V, Miloslavsky M, Wang D, Lu Y, Lull J, Tudor IC, Liu E, Grundman M, Yuen E, Black R, Brashear HR, Investigators BaCT (2014) Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s disease. New Engl J Med 370(4):322–333
Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, Raman R, Sun X, Aisen PS, Siemers E, Liu-Seifert H, Mohs R (2014) Phase 3 trials of solanezumab for mild-to-moderate alzheimer’s disease. New Engl J Med 370(4):311–321. doi:10.1056/NEJMoa1312889
Doody RS, Raman R, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, He F, Sun X, Thomas RG, Aisen PS, Siemers E, Sethuraman G, Mohs R (2013) A phase 3 trial of semagacestat for treatment of alzheimer’s disease. New Engl J Med 369(4):341–350. doi:10.1056/NEJMoa1210951
Lesné S, Kotilinek L, Ashe KH (2008) Plaque-bearing mice with reduced levels of oligomeric amyloid-β assemblies have intact memory function. Neuroscience 151(3):745–749
Hefti F, Goure WF, Jerecic J, Iverson KS, Walicke PA, Krafft GA (2013) The case for soluble Aβ oligomers as a drug target in Alzheimer’s disease. Trends Pharmacol Sci 34(5):261–266. doi:10.1016/j.tips.2013.03.002
Lee H-G, Castellani RJ, Zhu X, Perry G, Smith MA (2005) Amyloid-β in Alzheimer’s disease: the horse or the cart? Pathogenic or protective? Int J Exp Pathol 86(3):133–138
Lee H-G, Casadesus G, Zhu X, Takeda A, Perry G, Smith MA (2009) Challenging the amyloid cascade hypothesis: senile plaques and amyloid-β as protective adaptations to Alzheimer disease. Ann NY Acad Sci 1019:1–4
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman BT, Burton MA, Goldstein LE, Duong S, Tanzi RE, Moir RD (2010) The Alzheimer’s disease-associated amyloid ß-protein is an antimicrobial peptide. PloS ONE 5:3
Glass DJ, Arnold SE (2012) Some evolutionary perspectives on Alzheimer’s disease pathogenesis and pathology. Alzheimer’s Dement 8(4):343–351. doi:10.1016/j.jalz.2011.05.2408
Ewbank DC, Arnold SE (2009) Cool with plaques and tangles. New Engl J Med 360(22):2357–2359
Kamenetz F, Tomita T, Hsieh H, Seabrook GR, Borchelt D, Iwatsubo T, Sisodia SS, Malinow R (2003) APP processing and synaptic function. Neuron 37(6):925–937
Yao Z-X, Papadopoulos V (2002) Function of ß-amyloid in cholesterol transport: a lead to neurotoxicity. FASEB J 16:1677–1679
Puzzo D, Privitera L, Leznik E, Fa M, Staniszewski A, Palmeri A, Arancio O (2008) Picomolar amyloid-β positively modulates synaptic plasticity and memory in hippocampus. J Neurosci 28(53):14537–14545
Garcia-Osta A, Alberini CM (2009) Amyloid beta mediates memory formation. Learn Mem 16:267–272
Senechal Y, Kelly PH, Dev KK (2008) Amyloid precursor protein knockout mice show age-dependent deficits in passive avoidance learning. Behav Brain Res 186(1):126–132
Castellani RJ, H-g Lee, Nunomura A, Perry G, Smith MA (2006) Neuropathology of Alzheimer disease: pathognomonic but not pathogenic. Acta Neuropathol (Berl) 111(6):503–509
Bennett DA, Schneider JA, Arvanitakis Z, Kelly JF, Aggarwal NT, Shah RC, Wilson RS (2006) Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology 66(12):1837–1844
White L (2009) Brain lesions at autopsy in older Japanese-American men as related to cognitive impairment and dementia in the final years of life: a summary report from the honolulu-asia aging study. J Alzheimers Dis. doi:10.3233/JAD-2009-1178
O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L, Crain BJ, Pletnikova O, Rudow G, Iacono D, Riudavets MA, Driscoll I, Price DL, Martin LJ, Troncoso JC (2009) Neuropathologic studies of the Baltimore longitudinal study of aging (BLSA). J Alzheimers Dis. doi:10.3233/JAD-2009-1179
Iacono D, Markesbery WR, Gross M, Pletnikova O, Rudow G, Zandi P, Troncoso JC (2009) The nun study: clinically silent AD, neuronal hypertrophy, and linguistic skills in early life. Neurology 73(9):665–673. doi:10.1212/WNL.0b013e3181b01077
Braak H, Braak E (1997) Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging 18(4):351–357
Hardy JA (2003) The relationship between amyloid and tau. J Mol Neurosci 20(2):203–206
Eckert A, Schulz KL, Rhein V, Götz J (2010) Convergence of amyloid-β and tau pathologies on mitochondria in vivo. Mol Neurobiol 41(2–3):107–114
Lee HG, Perry G, Moreira PI, Garrett MR, Liu Q, Zhu X, Takeda A, Nunomura A, Smith MA (2005) Tau phosphorylation in Alzheimer’s disease: pathogen or protector? Trends Mol Med 11(4):164–169
Jucker M, Walker LC (2011) Pathogenic protein seeding in alzheimer disease and other neurodegenerative disorders. Ann Neurol 70(4):532–540. doi:10.1002/ana.22615
Guo JL, Lee VMY (2014) Cell-to-cell transmission of pathogenic proteins in neurodegenerative diseases. Nat Med 20:130–138
Li J, Browning S, Mahal SP, Oelschlegel AM, Weissmann C (2010) Darwinian evolution of prions in cell culture. Science 327(5967):869–872
Finch CE, Sapolsky RM (1999) The evolution of Alzheimer disease, the reproductive schedule, and apoE isoforms. Neurobiol Aging 20:407–428
Kimura N, Nakamura S, Goto N, Narushima E, Hara I, Shichiri S, Saitou K, Nose M, Hayashi T, Kawamura S, Yoshikawa Y (2001) Senile plaques in an aged western lowland gorilla. Exp Anim 50(1):77–81
Rosen RF, Walker LC, LeVine H (2011) PIB binding in aged primate brain: Enrichment of high-affinity sites in humans with Alzheimer’s disease. Neurobiol Aging 32(2):223–234
Sarasa M, Gallego C (2006) Alzheimer-like neurodegeneration as a probable cause of cetacean stranding. FENS Forum 3
Nakayama H, Katayama K, Ikawa A, Miyawaki K, Shinozuka J, Uetsuka K, Nakamura S, Kimura N, Yoshikawa Y, Doi K (1999) Cerebral amyloid angiopathy in an aged great spotted woodpecker (Picoides major). Neurobiol Aging 20(1):53–56
Fahlström A, Yu Q, Ulfhake B (2009) Behavioral changes in aging female C57BL/6 mice. Neurobiol Aging
Landsberg G, Araujo JA (2005) Behavior problems in geriatric pets. Vet Clin Small Anim 35:675–698
Maldonado TA, Jones RE, Norris DO (2000) Distribution of b-amyloid and amyloid precursor protein in the brain of spawning (senescent) salmon: a natural, brain-aging model. Brain Res 858:237–251
Yu J-T, Tan L, Hardy JA (2014) Apolipoprotein E in Alzheimer’s disease: an update. Ann Rev Neurosci 37:79–100
Nesse RM, Williams GC (1994) Why we get sick: the new science of Darwinian medicine. Times Books, New York
Nesse RM, Bergstrom CT, Ellison PT, Flier JS, Gluckman P, Govindaraju DR, Niethammer D, Omenn GS, Perlman RL, Schwartz MD, Thomas MG, Stearns SC, Valle D (2010) Making evolutionary biology a basic science for medicine. Proc Natl Acad Sci 107(suppl 1):1800–1807. doi:10.1073/pnas.0906224106
Finch CE (2010) Evolution of the human lifespan and diseases of aging: roles of infection, inflammation, and nutrition. Proc Natl Acad Sci 107(suppl 1):1718–1724. doi:10.1073/pnas.0909606106
Terry RD, Katzman R (2001) Life span and synapses: will there be a primary senile dementia? Neurobiol Aging 22(3):347–348
Health UNIo (2014) Estimates of funding for various research, condition, and disease categories (RCDC). http://report.nih.gov/categorical_spending.aspx. Accessed 25 Aug 2014
Corder EH, Saunders AM, Risch NJ, Strittmatter WJ, Schmechel DE, Gaskell PC, Rimmler JB, Locke PA, Conneally PM, Schmader KE, Small GW, Roses AD, Haines JL, Pericak-Vance MA (1994) Protective effect of apolipoprotein E type 2 for late-onset alzheimer’s disease. Nature Genet 7:180–184
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Glossary
- APOE
-
A gene involved in the expression of a protein called apolipoprotein-E. This protein is implicated in transporting cholesterol through the bloodstream. There are three variants of the protein caused by different forms of the gene, known as E2, E3, and E4 or sometimes ε2, ε3, and ε4. The E3 allele is the most common. The E4 allele is associated with a higher risk of cardiovascular disease and AD than E3, whereas the E2 allele is associated with a reduced risk of AD relative to E3 [8, 82].
- Amyloid-β
-
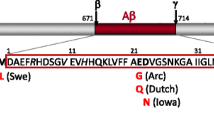
(pronounced “amyloid-beta”; a.k.a. beta-amyloid, Aβ) One of the proteins involved in the pathology of AD. It can take one of several forms including oligomers, which are small chainlike molecules, and plaques, which are large insoluble aggregates of Aβ that accumulate in the brains of Alzheimer’s patients. Its normal function is not well-understood, although it may be involved in immune response, cellular metabolism, or a number of other processes. Aβ is formed when a protein called amyloid precursor protein (APP) is cut by two other proteins, known as β-secretase (beta-secretase) and γ-secretase (gamma-secretase). Aβ in plaque or oligomeric form has traditionally been thought to be one of the causes of the neurodegeneration seen in Alzheimer’s disease.
- Tau protein
-
The other protein whose abnormal processing forms the signature neurofibrillary tangle of Alzheimer’s disease. Normally, tau functions to stabilize microtubules, which support the cytoskeleton of neurons in the central nervous system. As part of its normal function, tau changes its shape via phosphorylation, a process wherein phosphate groups bind to tau and allow it to change configurations. In Alzheimer’s disease, tau becomes saturated with phosphates, a process called hyperphosphorylation, which promotes its misfolding into filamentous structures called paired helical filaments. These paired helical filaments, in turn, aggregate into neurofibrillary (i.e., “nerve fiber”) tangles, which, along with plaques, are a marker of Alzheimer’s disease. Tau tangles have been thought to play a role in neuron death.
- Oxidative stress
-
A process caused by by-products of metabolism in which so-called reactive oxygen species or free radicals overwhelm the body’s ability to neutralize them, potentially causing damage to DNA and proteins. Reactive oxygen species are molecules or ions of oxygen that are missing one electron, making them highly reactive. Oxidative stress may play key roles in a number of neurodegenerative diseases, including Alzheimer’s disease.
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Glass, D.J., Arnold, S.E. (2016). Why Are Humans Vulnerable to Alzheimer’s Disease?. In: Alvergne, A., Jenkinson, C., Faurie, C. (eds) Evolutionary Thinking in Medicine. Advances in the Evolutionary Analysis of Human Behaviour. Springer, Cham. https://doi.org/10.1007/978-3-319-29716-3_21
Download citation
DOI: https://doi.org/10.1007/978-3-319-29716-3_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29714-9
Online ISBN: 978-3-319-29716-3
eBook Packages: MedicineMedicine (R0)