Abstract
Background
Proton pump inhibitors (PPIs) may reduce the risk of esophageal adenocarcinoma (EAC) in patients with Barrett’s esophagus. PPIs are prescribed for virtually all patients with Barrett’s esophagus, irrespective of the presence of reflux symptoms, and represent a de facto chemopreventive agent in this population. However, long-term PPI use has been associated with several adverse effects, and the cost-effectiveness of chemoprevention with PPIs has not been evaluated.
Aim
The purpose of this study was to assess the cost-effectiveness of PPIs for the prevention of EAC in Barrett’s esophagus without reflux.
Methods
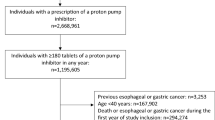
We designed a state-transition Markov microsimulation model of a hypothetical cohort of 50-year-old white men with Barrett’s esophagus. We modeled chemoprevention with PPIs or no chemoprevention, with endoscopic surveillance for all treatment arms. Outcome measures were life-years, quality-adjusted life years (QALYs), incident EAC cases and deaths, costs, and incremental cost-effectiveness ratios.
Results
Assuming 50 % reduction in EAC, chemoprevention with PPIs was a cost-effective strategy compared to no chemoprevention. In our model, administration of PPIs cost $23,000 per patient and resulted in a gain of 0.32 QALYs for an incremental cost-effectiveness ratio of $12,000/QALY. In sensitivity analyses, PPIs would be cost-effective at $50,000/QALY if they reduce EAC risk by at least 19 %.
Conclusions
Chemoprevention with PPIs in patients with Barrett’s esophagus without reflux is cost-effective if PPIs reduce EAC by a minimum of 19 %. The identification of subgroups of Barrett’s esophagus patients at increased risk for progression would lead to more cost-effective strategies for the prevention of esophageal adenocarcinoma.



Similar content being viewed by others
References
Brown LM, Devesa SS, Chow WH. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst. 2008;100:1184–1187.
Abrams JA, Sharaiha RZ, Gonsalves L, et al. Dating the rise of esophageal adenocarcinoma: analysis of Connecticut Tumor Registry data, 1940–2007. Cancer Epidemiol Biomarkers Prev. 2011;20:183–186.
Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Wani S, Falk G, Hall M, et al. Patients with nondysplastic Barrett’s esophagus have low risks for developing dysplasia or esophageal adenocarcinoma. Clin Gastroenterol Hepatol. 2011;9:220–227. (quiz e26).
Hvid-Jensen F, Pedersen L, Drewes AM, et al. Incidence of adenocarcinoma among patients with Barrett’s esophagus. N Engl J Med. 2011;365:1375–1383.
Bhat S, Coleman HG, Yousef F, et al. Risk of malignant progression in Barrett’s esophagus patients: results from a large population-based study. J Natl Cancer Inst. 2011;103:1049–1057.
Shaheen NJ, Crosby MA, Bozymski EM, et al. Is there publication bias in the reporting of cancer risk in Barrett’s esophagus? Gastroenterology. 2000;119:333–338.
Wang KK, Sampliner RE. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett’s esophagus. Am J Gastroenterol. 2008;103:788–797.
Corley DA, Mehtani K, Quesenberry C, et al. Impact of endoscopic surveillance on mortality from Barrett’s esophagus-associated esophageal adenocarcinomas. Gastroenterology. 2013;145:312 e1–319 e1.
Lagergren J, Bergstrom R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–831.
Jung KW, Talley NJ, Romero Y, et al. Epidemiology and natural history of intestinal metaplasia of the gastroesophageal junction and Barrett’s esophagus: a population-based study. Am J Gastroenterol. 2011;106:1447–1455. (quiz 1456).
Hillman LC, Chiragakis L, Shadbolt B, et al. Effect of proton pump inhibitors on markers of risk for high-grade dysplasia and oesophageal cancer in Barrett’s oesophagus. Aliment Pharmacol Ther. 2008;27:321–326.
El-Serag HB, Aguirre TV, Davis S, et al. Proton pump inhibitors are associated with reduced incidence of dysplasia in Barrett’s esophagus. Am J Gastroenterol. 2004;99:1877–1883.
de Jonge PJ, Steyerberg EW, Kuipers EJ, et al. Risk factors for the development of esophageal adenocarcinoma in Barrett’s esophagus. Am J Gastroenterol. 2006;101:1421–1429.
Singh S, Garg SK, Singh PP, et al. Acid-suppressive medications and risk of oesophageal adenocarcinoma in patients with Barrett’s oesophagus: a systematic review and meta-analysis. Gut. 2013. doi:10.1136/gutjnl-2013-305997.
Spechler SJ. Barrett esophagus and risk of esophageal cancer: a clinical review. JAMA. 2013;310:627–636.
Nguyen DM, Richardson P, El-Serag HB. Medications (NSAIDs, statins, proton pump inhibitors) and the risk of esophageal adenocarcinoma in patients with Barrett’s esophagus. Gastroenterology. 2010;138:2260–2266.
Veldhuyzen van Zanten SJ, Thomson AB, Barkun AN, et al. The prevalence of Barrett’s oesophagus in a cohort of 1040 Canadian primary care patients with uninvestigated dyspepsia undergoing prompt endoscopy. Aliment Pharmacol Ther. 2006;23:595–599.
Voutilainen M, Sipponen P, Mecklin JP, et al. Gastroesophageal reflux disease: prevalence, clinical, endoscopic and histopathological findings in 1,128 consecutive patients referred for endoscopy due to dyspeptic and reflux symptoms. Digestion. 2000;61:6–13.
Abrams JA, Fields S, Lightdale CJ, et al. Racial and ethnic disparities in the prevalence of Barrett’s esophagus among patients who undergo upper endoscopy. Clin Gastroenterol Hepatol. 2008;6:30–34.
Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–1831.
Rex DK, Cummings OW, Shaw M, et al. Screening for Barrett’s esophagus in colonoscopy patients with and without heartburn. Gastroenterology. 2003;125:1670–1677.
Peery AF, Hoppo T, Garman KS, et al. Feasibility, safety, acceptability, and yield of office-based, screening transnasal esophagoscopy (with video). Gastrointest Endosc. 2012;75:945–953.
Kadri SR, Lao-Sirieix P, O’Donovan M, et al. Acceptability and accuracy of a non-endoscopic screening test for Barrett’s oesophagus in primary care: cohort study. BMJ. 2010;341:c4372.
Yang YX, Lewis JD, Epstein S, et al. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947–2953.
Dial S, Delaney JA, Barkun AN, et al. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA. 2005;294:2989–2995.
Gray SL, LaCroix AZ, Larson J, et al. Proton pump inhibitor use, hip fracture, and change in bone mineral density in postmenopausal women: results from the Women’s Health Initiative. Arch Intern Med. 2010;170:765–771.
Corley DA, Kubo A, Zhao W, et al. Proton pump inhibitors and histamine-2 receptor antagonists are associated with hip fractures among at-risk patients. Gastroenterology. 2010;139:93–101.
Loo VG, Bourgault AM, Poirier L, et al. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med. 2011;365:1693–1703.
Food and Drug Administration, U.S. Department of Health and Human Services. http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm213206.htm. Accessed October 15, 2013.
Food and Drug Administration, U.S. Department of Health and Human Services. http://www.fda.gov/drugs/drugsafety/ucm290510.htm. Accessed October 15, 2013.
Spechler SJ, Sharma P, Souza RF, et al. American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology. 2011;140:1084–1091.
Spechler SJ, Sharma P, Souza RF, et al. American Gastroenterological Association technical review on the management of Barrett’s esophagus. Gastroenterology. 2011;140:e18–e52. (quiz e13).
Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277–2288.
Streitz JM Jr, Andrews CW Jr, Ellis FH Jr. Endoscopic surveillance of Barrett’s esophagus. Does it help? J Thorac Cardiovasc Surg. 1993;105:383–387.
Corley DA, Levin TR, Habel LA, et al. Surveillance and survival in Barrett’s adenocarcinomas: a population-based study. Gastroenterology. 2002;122:633–640.
Khanna S, Pardi DS, Aronson SL, et al. The epidemiology of community-acquired Clostridium difficile infection: a population-based study. Am J Gastroenterol. 2012;107:89–95.
Chitnis AS, Holzbauer SM, Belflower RM, et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013;173:1359–1367.
National Cancer Institute, Surveillance Epidemiology and End Results. http://seer.cancer.gov/. Accessed October 15, 2013.
Gold M. Panel on cost-effectiveness in health and medicine. Med Care. 1996;34:197–199.
Centers for Medicare and Medicaid Services. Physician Fee Schedule Search. http://www.cms.gov/apps/physician-fee-schedule/. Accessed October 15, 2013.
Physician Fee Schedule Look-up. Available from: https://www.cms.gov/. Accessed September 1, 2011.
Roberts KJ, Harper E, Alderson D, et al. Long-term survival and cost analysis of an annual Barrett’s surveillance programme. Eur J Gastroenterol Hepatol. 2010;22:399–403.
Liu H, Michaud K, Nayak S, et al. The cost-effectiveness of therapy with teriparatide and alendronate in women with severe osteoporosis. Arch Intern Med. 2006;166:1209–1217.
Lee BY, Popovich MJ, Tian Y, et al. The potential value of Clostridium difficile vaccine: an economic computer simulation model. Vaccine. 2010;28:5245–5253.
Hunink M, Glasziou P. Decision Making in Health and Medicine: Integrating Evidence and Values. Cambridge: Cambridge University Press; 2001.
Hur C, Nishioka NS, Gazelle GS. Cost-effectiveness of aspirin chemoprevention for Barrett’s esophagus. J Natl Cancer Inst. 2004;96:316–325.
Inadomi JM, Somsouk M, Madanick RD, et al. A cost-utility analysis of ablative therapy for Barrett’s esophagus. Gastroenterology. 2009;136:2101 e1-6–2114 e1-6.
Gordon LG, Mayne GC, Hirst NG, et al. Cost-effectiveness of endoscopic surveillance of non-dysplastic Barrett’s esophagus. Gastrointest Endosc. 2013;79:242–256.
Desai TK, Krishnan K, Samala N, et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012;61:970–976.
Kastelein F, Spaander MC, Steyerberg EW, et al. Proton pump inhibitors reduce the risk of neoplastic progression in patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2013;11:382–388.
Taylor JB, Rubenstein JH (2010) Meta-analyses of the effect of symptoms of gastroesophageal reflux on the risk of Barrett’s esophagus. Am J Gastroenterol. 2010;105:1729, 1730-7; quiz 1738.
Laroui H, Dalmasso G, Nguyen HT, et al. Drug-loaded nanoparticles targeted to the colon with polysaccharide hydrogel reduce colitis in a mouse model. Gastroenterology. 2010;138:843e1-2–853e1-2.
Chey WD, Inadomi JM, Booher AM, et al. Primary-care physicians’ perceptions and practices on the management of GERD: results of a national survey. Am J Gastroenterol. 2005;100:1237–1242.
Hillman LC, Chiragakis L, Shadbolt B, et al. Proton-pump inhibitor therapy and the development of dysplasia in patients with Barrett’s oesophagus. Med J Aust. 2004;180:387–391.
Fitzgerald RC, Omary MB, Triadafilopoulos G. Dynamic effects of acid on Barrett’s esophagus. An ex vivo proliferation and differentiation model. J Clin Invest. 1996;98:2120–2128.
Souza RF, Shewmake K, Terada LS, et al. Acid exposure activates the mitogen-activated protein kinase pathways in Barrett’s esophagus. Gastroenterology. 2002;122:299–307.
Souza RF, Shewmake K, Pearson S, et al. Acid increases proliferation via ERK and p38 MAPK-mediated increases in cyclooxygenase-2 in Barrett’s adenocarcinoma cells. Am J Physiol Gastrointest Liver Physiol. 2004;287:G743–G748.
Drug Topics, 2001 Red Book. Montvale, NJ: PDR Network, LLC; 2001.
Heath EI, Canto MI, Piantadosi S, et al. Secondary chemoprevention of Barrett’s esophagus with celecoxib: results of a randomized trial. J Natl Cancer Inst. 2007;99:545–557.
Abrams JA. Chemoprevention of esophageal adenocarcinoma. Therap Adv Gastroenterol. 2008;1:7–18.
Sinicrope FA, Broaddus R, Joshi N, et al. Evaluation of difluoromethylornithine for the chemoprevention of Barrett’s esophagus and mucosal dysplasia. Cancer Prev Res (Phila). 2011;4:829–839.
Jankowski J, Moayyedi P. Re: cost-effectiveness of aspirin chemoprevention for Barrett’s esophagus. J Natl Cancer Inst. 2004;96:885–887. (author reply 887).
Kwok CS, Arthur AK, Anibueze CI, et al. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. Am J Gastroenterol. 2012;107:1011–1019.
Janarthanan S, Ditah I, Adler DG, et al. Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: a meta-analysis. Am J Gastroenterol. 2012;107:1001–1010.
Targownik LE, Leslie WD, Davison KS, et al. The relationship between proton pump inhibitor use and longitudinal change in bone mineral density: a population-based study [corrected] from the Canadian Multicentre Osteoporosis Study (CaMos). Am J Gastroenterol. 2012;107:1361–1369.
Sonnenberg A, Fennerty MB. Medical decision analysis of chemoprevention against esophageal adenocarcinoma. Gastroenterology. 2003;124:1758–1766.
Choi SE, Perzan K, Tramontano AC, et al. Statins and aspirin for chemoprevention in Barrett’s esophagus: results of a cost-effectiveness analysis. Cancer Prev Res (Phila). 2014;7:341–350.
Hur C, Choi SE, Rubenstein JH, et al. The cost effectiveness of radiofrequency ablation for Barrett’s esophagus. Gastroenterology. 2012;143:567–575.
Acknowledgments
Dr. Sharaiha was supported by a training grant from the National Cancer Institute (T32 CA009529). Dr. Freedberg is supported in part by a training grant from the National Institute of Diabetes and Digestive and Kidney Diseases (T32 DK083256-04). Dr. Abrams was supported in part by a Career Development Award from the National Cancer Institute (K07 CA132892). This publication was also supported in part by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 RR024156.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10620_2014_3186_MOESM1_ESM.tif
Supplemental Figure 1. Sensitivity analyses varying cost and risk reduction for chemoprevention with proton pump inhibitors, with no chemoprevention (surveillance only) compared to PPIs. The X-axis represents the % EACs prevented by PPI therapy, and the Y-axis represents the cost ($/year) of PPIs. Figure 4A represents the analyses for WTP $50,000, whereas Figure 4B represents WTP $100,000. (TIFF 184 kb)
Rights and permissions
About this article
Cite this article
Sharaiha, R.Z., Freedberg, D.E., Abrams, J.A. et al. Cost-Effectiveness of Chemoprevention with Proton Pump Inhibitors in Barrett’s Esophagus. Dig Dis Sci 59, 1222–1230 (2014). https://doi.org/10.1007/s10620-014-3186-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3186-3