Abstract
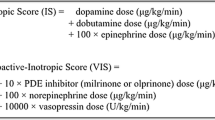
Low cardiac output syndrome (LCOS) and maximum vasoactive inotropic score (VIS) have been used as surrogate markers for early postoperative outcomes in pediatric cardiac surgery. The objective of this study was to determine the associations between LCOS and maximum VIS with clinical outcomes in neonatal cardiac surgery. This was a secondary retrospective analysis of a prospective randomized trial, and the setting was a pediatric cardiac intensive care unit in a tertiary care children’s hospital. Neonates (n = 76) undergoing corrective or palliative cardiac operations requiring cardiopulmonary bypass were prospectively enrolled. LCOS was defined by a standardized clinical criteria. VIS values were calculated by a standard formula during the first 36 postoperative hours, and the maximum score was recorded. Postoperative outcomes included hospital mortality, duration of mechanical ventilation, intensive care unit (ICU) and hospital lengths of stay (LOS), as well as total hospital charges. At surgery, the median age was 7 days and weight was 3.2 kg. LCOS occurred in 32 of 76 (42%) subjects. Median maximum VIS was 15 (range 5–33). LCOS was not associated with duration of mechanical ventilation, ICU LOS, hospital LOS, and hospital charges. Greater VIS was moderately associated with a longer duration of mechanical ventilation (p = 0.001, r = 0.36), longer ICU LOS (p = 0.02, r = 0.27), and greater total hospital costs (p = 0.05, r = 0.22) but not hospital LOS (p = 0.52). LCOS was not associated with early postoperative outcomes. Maximum VIS has only modest correlation with duration of mechanical ventilation, ICU LOS, and total hospital charges.



Similar content being viewed by others
References
Balaguru D, Haddock PS, Puglisi JL, Bers DM, Coetzee WA, Artman M (1997) Role of the sarcoplasmic reticulum in contraction and relaxation of immature rabbit ventricular myocytes. J Mol Cell Cardiol 29(10):2747–2757
Basaran M, Sever K, Kafali E, Ugurlucan M, Sayin OA, Tansel T et al (2006) Serum lactate level has prognostic significance after pediatric cardiac surgery. J Cardiothorac Vasc Anesth 20(1):43–47
Bradley SM, Simsic JM, McQuinn TC, Habib DM, Shirali GS, Atz AM (2004) Hemodynamic status after the Norwood procedure: a comparison of right ventricle-to-pulmonary artery connection versus modified Blalock–Taussig shunt. Ann Thorac Surg 78(3):933–941 (discussion 933–941)
Carmona F, Manso PH, Vicente WV, Castro M, Carlotti AP (2008) Risk stratification in neonates and infants submitted to cardiac surgery with cardiopulmonary bypass: a multimarker approach combining inflammatory mediators, N-terminal pro-B-type natriuretic peptide and troponin I. Cytokine 42(3):317–324
Dorfman AT, Marino BS, Wernovsky G, Tabbutt S, Ravishankar C, Godinez RI et al (2008) Critical heart disease in the neonate: presentation and outcome at a tertiary care center. Pediatr Crit Care Med 9(2):193–202
Froese NR, Sett SS, Mock T, Krahn GE (2009) Does troponin-I measurement predict low cardiac output syndrome following cardiac surgery in children? Crit Care Resusc 11(2):116–121
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG et al (2010) Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11(2):234–238
Graham EM, Atz AM, Butts RJ, Baker NL, Zyblewski SC, Deardorff RL et al (2011) Standardized preoperative corticosteroid treatment in neonates undergoing cardiac surgery: results from a randomized trial. J Thorac Cardiovasc Surg 142(6):1523-1529
Hatem SN, Sweeten T, Vetter V, Morad M (1995) Evidence for presence of Ca2+ channel-gated Ca2+ stores in neonatal human atrial myocytes. Am J Physiol 268(3 Pt 2):H1195–H1201
Hoffman TM, Wernovsky G, Atz AM, Kulik TJ, Nelson DP, Chang AC et al (2003) Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation 107(7):996–1002
Horvath R, Shore S, Schultz SE, Rosenkranz ER, Cousins M, Ricci M (2010) Cerebral and somatic oxygen saturation decrease after delayed sternal closure in children after cardiac surgery. J Thorac Cardiovasc Surg 139(4):894–900
Iversen LL, De Champlain J, Glowinski J, Axelrod J (1967) Uptake, storage and metabolism of norepinephrine in tissues of the developing rat. J Pharmacol Exp Ther 157(3):509–516
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI (2002) Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 123(1):110–118
Khairy P, Ionescu-Ittu R, Mackie AS, Abrahamowicz M, Pilote L, Marelli AJ (2010) Changing mortality in congenital heart disease. J Am Coll Cardiol 56(14):1149–1157
Kulik TJ, Moler FW, Palmisano JM, Custer JR, Mosca RS, Bove EL et al (1996) Outcome-associated factors in pediatric patients treated with extracorporeal membrane oxygenator after cardiac surgery. Circulation 94(9 Suppl):II63–II68
Lacour-Gayet F, Clarke D, Jacobs J, Comas J, Daebritz S, Daenen W et al (2004) The Aristotle score: a complexity-adjusted method to evaluate surgical results. Eur J Cardiothorac Surg 25(6):911–924
Marino BS, Tomlinson RS, Wernovsky G, Drotar D, Newburger JW, Mahony L et al (2010) Validation of the pediatric cardiac quality of life inventory. Pediatrics 126(3):498–508
Marino BS, Drotar D, Cassedy A, Davis R, Tomlinson RS, Mellion K et al (2011) External validity of the pediatric cardiac quality of life inventory. Qual Life Res 20(2):205–214
Maylie JG (1982) Excitation–contraction coupling in neonatal and adult myocardium of cat. Am J Physiol 242(5):H834–H843
Nassar R, Reedy MC, Anderson PA (1987) Developmental changes in the ultrastructure and sarcomere shortening of the isolated rabbit ventricular myocyte. Circ Res 61(3):465–483
Newburger JW, Wypij D, Bellinger DC, du Plessis AJ, Kuban KC, Rappaport LA et al (2003) Length of stay after infant heart surgery is related to cognitive outcome at age 8 years. J Pediatr 143(1):67–73
Schroeder VA, Pearl JM, Schwartz SM, Shanley TP, Manning PB, Nelson DP (2003) Combined steroid treatment for congenital heart surgery improves oxygen delivery and reduces postbypass inflammatory mediator expression. Circulation 107(22):2823–2828
Seear MD, Scarfe JC, LeBlanc JG (2008) Predicting major adverse events after cardiac surgery in children. Pediatr Crit Care Med 9(6):606–611
Soul JS, Robertson RL, Wypij D, Bellinger DC, Visconti KJ, du Plessis AJ et al (2009) Subtle hemorrhagic brain injury is associated with neurodevelopmental impairment in infants with repaired congenital heart disease. J Thorac Cardiovasc Surg 138(2):374–381
Wernovsky G, Wypij D, Jonas RA, Mayer JEJ, Hanley FL, Hickey PR et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92(8):2226–2235
Acknowledgment
This study was supported in part by a Career Development Award from the American College of Cardiology Foundation/Pfizer Scholarship (E. M. G.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Butts, R.J., Scheurer, M.A., Atz, A.M. et al. Comparison of Maximum Vasoactive Inotropic Score and Low Cardiac Output Syndrome As Markers of Early Postoperative Outcomes After Neonatal Cardiac Surgery. Pediatr Cardiol 33, 633–638 (2012). https://doi.org/10.1007/s00246-012-0193-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-012-0193-z