Abstract
This study was undertaken to investigate epidermal growth factor receptor (EGFR) and human epidermal growth factor receptor 2 (HER-2)/neu expression in a cohort of apocrine carcinomas of the breast with emphasis on the classification of the breast tumors with apocrine morphology. In total, 55 breast carcinomas morphologically diagnosed as apocrine were evaluated for the steroid receptor expression profile characteristic of normal apocrine epithelium (androgen receptor positive/estrogen receptor (ER) negative/progesterone receptor (PR) negative), and for the expression of EGFR and Her-2/neu proteins, and the copy number ratios of the genes EGFR/CEP7 and HER-2/CEP17. On the basis of the results of steroid receptors expression, 38 (69%) cases were classified as pure apocrine carcinoma (androgen receptor positive/ER negative/PR negative), whereas 17 (31%) were re-classified as apocrine-like carcinomas because they did not have the characteristic steroid receptor expression profile. Her-2/neu overexpression was observed in 54% of the cases (57% pure apocrine carcinomas vs 47% apocrine-like carcinomas). HER-2/neu gene amplification was demonstrated in 52% of all cases (54% pure apocrine carcinomas vs 46% apocrine-like carcinomas). EGFR protein (scores 1 to 3+) was detected in 62% of all cases and was expressed in a higher proportion of pure apocrine carcinomas than in the apocrine-like carcinomas group (76 vs 29%, P=0.006). In the pure apocrine carcinoma group, Her-2/neu and EGFR protein expression were inversely correlated (P=0.006, r=−0.499). EGFR gene amplification was observed in two pure apocrine carcinomas and one apocrine-like carcinoma. Polysomy 7 was commonly present in pure apocrine carcinomas (61 vs 27% of apocrine-like carcinomas; P=0.083) and showed a weak positive correlation with EGFR protein expression (P=0.025, r=0.326). Our study showed that apocrine breast carcinomas are molecularly diverse group of carcinomas. Strictly defined pure apocrine carcinomas are either HER-2-overexpressing breast carcinomas or triple-negative breast carcinomas, whereas apocrine-like carcinomas predominantly belong to the luminal phenotype. Pure apocrine carcinomas show consistent overexpression of either EGFR or HER-2/neu, which could have significant therapeutic implications.
Similar content being viewed by others
Main
Apocrine carcinomas of the breast, defined as breast tumors composed of epithelium with apocrine differentiation in >90% of the tumor cell population, represent a rare subtype, constituting <5% of all breast cancers.1, 2, 3 Apocrine differentiation is defined by the presence of large cells with prominent eosinophilic, flocculent cytoplasm, with sharply defined cell borders, and with large nuclei containing prominent macronucleoli. Importantly, a characteristic steroid receptor expression profile further defines these tumors as consistently estrogen receptor (ER) negative, progesterone receptor (PR) negative and androgen receptor (AR) positive.4, 5, 6, 7, 8 Although AR expression has been variably observed in up to 60–70% breast carcinomas,9, 10 consistent AR expression tends to be a feature of apocrine breast lesions including invasive apocrine carcinomas.4, 5, 8, 11, 12 Moreover, recently published gene expression microarray studies defined a characteristic ‘molecular apocrine’ gene expression profile found in apocrine carcinomas. These studies showed apocrine tumors to be different from common luminal and basal cell breast carcinoma subtypes.13, 14, 15, 16 This molecular apocrine group was characterized by increased AR signaling along with increased human epidermal growth factor receptor 2 (HER-2)/neu gene signaling.13, 16 A study using an apocrine cell line model also demonstrated the existence of a functionally significant cross-talk between AR and HER-2/neu pathways through ERK1/2 in ER-negative breast carcinomas.17 This cross-talk affects cell proliferation and apoptosis and could have a significant therapeutic impact.17 Although apocrine carcinoma exhibits distinctive histopatological and molecular features, the lack of standardized diagnostic criteria has produced controversial and heterogeneous results in the scientific literature in terms of its immunohistochemical profile and molecular classification.2, 18, 19, 20
The erbB (HER) family is comprised of four homologous transmembrane receptors involved in growth factor cellular signaling.21 Epidermal growth factor receptor (EGFR) (or HER-1) and HER-2/neu genes are of particular importance in breast cancer pathogenesis as their activation and coexpression are associated with an aggressive clinical course and a poor outcome.22 Both proteins can be targeted by specific therapeutic modalities. However, these tyrosine kinase receptors have not been systematically studied in invasive apocrine carcinomas of the breast.
We studied EGFR and HER-2/neu in apocrine breast carcinomas meeting strict morphological and immunophenotypic criteria with regard to both protein expression and gene copy number. We identified significant differences between pure apocrine carcinoma (apocrine morphology and a characteristic AR+/ER−/PR− steroid receptor profile) and apocrine-like breast carcinomas (apocrine morphology without characteristic apocrine steroid receptor profile), which could have important diagnostic and therapeutic implications.
Materials and methods
Specimens
The formalin-fixed paraffin-embedded tumor samples were obtained from 55 female patients with invasive apocrine carcinomas (52 surgical and 3 core biopsy specimens). Mean age of patients was 62 years (range: 32–92 years). The cases were retrieved from the files of Creighton University Medical Center (Omaha, NE, USA), Kansas University Medical Center (Kansas City, KS, USA), Thomas Jefferson University Hospital (Philadelphia, PA, USA), The University of Texas Medical Branch (Galveston, TX, USA) and Clinical Center of the University of Sarajevo (Bosnia and Herzegovina). Routinely stained hematoxylin and eosin tumor sections were re-examined (ZG and SV) and the diagnoses were confirmed. Institutional review board of the Creighton University approved the study.
Immunohistochemistry
Immunohistochemical assays for ER-alpha (ER-α; clone 6F11, Ventana Medical Systems, Tucson, AZ, USA), PR (clone 16, Ventana Medical Systems), AR (Clone AR441, DakoCytomation, Carpinteria, CA, USA), EGFR (DAKO EGFR PharmDX diagnostic kit; DakoCytomation) and Her-2/neu (Clone CB11, Ventana Medical Systems) expression were performed on the formalin-fixed paraffin-embedded sections using the commercially available detection kits and automated staining procedures.
The tumor was regarded as positive for ER and PR if >5% of the cells showed nuclear staining, whereas a 10% cutoff was applied for AR staining.8, 23
Her-2/neu protein expression results were scored according to the American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations.24 Briefly, cases showing no membrane immunostaining or membrane immunostaining in <10% tumor cells were scored 0+; cases with weak and incomplete membrane staining in >10% of tumor cells were scored 1+; cases with complete membrane staining that was either nonuniform or weak in intensity but with obvious circumferential distribution in >10% of cells were scored 2+; and cases with strong membrane staining in >30% tumor cells were scored 3+.24
EGFR scoring was carried out according to the manufacturer's (Dako) recommendation: only membranous staining is considered as a specific positive result; weak (1+) intensity is defined as faint and incomplete membrane positivity; moderate (2+) intensity and strong (3+) staining are both varying degrees of circumferential staining of membranes. The tumor was considered positive if a proportion of stained cells exceeded 1% at any intensity.
Automated Cell Imaging System (ChromaVision Medical Systems, San Juan Capistrano, CA, USA) was used for measuring the percentage of cells with the nuclear staining for ER, PR and AR, and the extent and intensity of membranous staining of EGFR and Her-2/neu. Pathologists reviewed the images and selected tumor-rich areas of the sections for the analysis.
FISH Analysis
Fluorescent in situ hybridization (FISH) was performed to evaluate copy number at EGFR and HER-2/neu loci. Chromosome enumeration probes CEP7 and CEP17 were used as positive controls and indicators of chromosome ploidy (Abbott Molecular, Des Plaines, IL, USA). Probe signals were enumerated in predominant tumor cell populations. At least 30 nuclei were scored per sample. A ratio of HER-2/CEP17 >2.2 was defined as gene amplification; a ratio 1.8–2.1 was interpreted as borderline, and a ratio <1.8 was defined as negative. The same criteria were used for interpretation of EGFR/CEP7 ratios. Equivocal FISH results (ratio of 1.8–2.2) were considered as negative for HER-2/neu and EGFR gene amplification, respectively.24 Polysomy 7 and 17 were defined as three or more CEP signals per cell.21, 25, 26 Stromal cells and normal breast epithelial cells served as an internal control.
SNP Array Karyotyping
SNP array karyotyping was performed on selected cases. Following tumor enrichment through manual microdissection, DNA was obtained from 10-μm paraffin sections according to a previously described protocol for de-paraffinization and DNA extraction.27 Samples were processed with the 250K Nsp Assay Kits (Affymetrix, Santa Clara, CA, USA). Briefly, 1 μg of gDNA was digested with Nsp restriction enzyme, ligated to the adaptors and amplified by PCR using a universal primer. After purification of PCR products with SNP Clean magnetic beads (Agencourt Biosciences, Beverly MA, USA), amplicons were quantified, fragmented, labeled and hybridized to 250K Nsp arrays. After washing and staining, the arrays were scanned to generate CEL files for downstream analysis.
Data acquired from the Affymetrix GeneChip Operating System v4.0 (GCOS) was analyzed using Affymetrix Gene-Chip Genotyping Analysis Software (GTYPE) 4.1. Copy number analysis was performed with Copy Number Analyzer for Affymetrix GeneChip arrays (CNAG 3.0), as described before.28
Statistical Analysis
Where appropriate, χ2-test/Fisher's exact test or nonparametric tests (Mann–Whitney U-test) were used for comparisons of the groups. Spearman's correlation rank was applied for the correlation between the variables. All statistical analysis was carried out using the Statistical Package for the Social Sciences version 17.0 (SPSS, Chicago, IL, USA). P-values of <0.05 were considered significant.
Results
Classification and Steroid Receptor Profile of Apocrine Carcinomas
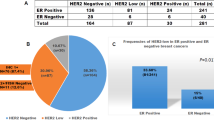
Morphologically, all 55 cases fulfilled the criteria for apocrine carcinoma and were characterized by large cells with prominent eosinophilic, flocculent cytoplasm, sharp cell borders and large nuclei with prominent macronucleoli (Figures 1a and b). Of these, 38 cases (69%) also fulfilled immunophenotypic diagnostic requirements for pure apocrine carcinoma: ER and PR negative, AR positive (Figures 1c and e, Table 1). The 17 remaining cases (31%) were then termed ‘apocrine-like’ carcinomas because they lacked the specific apocrine immunophenotypic profile (Figures 1d and f). These were further subcharacterized as apocrine-like carcinomas with ER+/AR− immunophenotype (three cases), apocrine-like carcinomas with ER−/AR− immunophenotype (four cases) and apocrine-like carcinomas with ER+/AR+ immunophenotype (10 cases) (Table 1).
(a and b) Hematoxylin and eosin -stained sections of two cases of breast carcinomas with apocrine features: pure apocrine carcinoma (a) and apocrine-like carcinoma (b) ( × 40 magnification). (c and d) Immunohistochemistry showing negative estrogen receptor expression in a case of pure apocrine carcinoma with a positive staining of normal epithelium (c), and strongly positive expression in an apocrine-like breast carcinoma (d) ( × 10 magnification). (e and f) Immunohistochemistry showing diffusely positive androgen receptor expression in a case of a pure apocrine carcinoma (e), and negative expression in an apocrine-like carcinoma (f) ( × 20 magnification). (g and h) Immunohistochemistry showing strong membrane expression of EGFR protein in a case of pure apocrine carcinoma (g), and 3+ membrane expression of Her-2/neu protein in a case of apocrine-like breast carcinoma (h) ( × 20 magnification).
The mean tumor AR positivity was significantly higher in the pure apocrine carcinoma subgroup in comparison with the apocrine-like carcinoma AR+/ER+ subgroup (76 vs 59%, P=0.037). Pure apocrine carcinomas exhibited a diffuse and strong nuclear staining of AR (16 of 30 or 53% of pure apocrine carcinomas had a 100% cells expressing AR). In contrast, none of the 17 apocrine-like carcinoma cases exhibited such complete AR expression.
HER-2/neu Expression in Apocrine Carcinomas
Her-2/neu protein overexpression (score 3+) was observed in 54% of the cases in the entire cohort without significant difference between the pure apocrine carcinoma and apocrine-like carcinoma groups (57 vs 47%, P=0.81) (Figure 1g).
HER-2/neu gene amplification was detected in 28 of 54 tested cases (52%) without significant differences between the pure apocrine carcinoma and the apocrine-like carcinoma group (54 vs 46%, P=0.42) (Figure 2a). The average HER-2/neu gene signal number per cell ranged from 1.67 to 50 (mean: 9.57). HER-2/neu FISH results were concordant with Her-2/neu immunohistochemistry results in 49 of 53 available cases (92%). Four positive immunohistochemistry Her-2/neu results (score 3+) were discordant with HER-2 FISH results (negative for HER-2/neu gene amplification). Three of eight cases (38%) with equivocal immunohistochemistry (score 2+) had HER-2/neu gene amplification.
Pure apocrine carcinomas showing HER-2/neu gene amplification (a), EGFR gene amplification (b), polysomy 17 (CEP17) without HER-2/neu gene amplification in a case of an apocrine-like carcinoma (average: 6.06 signals per cell) (c) and polysomy 7 (CEP7) without EGFR gene amplification (average: 3.62 signals per cell) (d).
Six samples had fewer HER-2/neu signals per cell than signals for chromosome 17 centromere (ratio: 0.72–0.99). One of these cases had a Her-2/neu protein overexpression.
Polysomy of chromosome 17 (defined as three or more copies of CEP17 signals per nucleus) was observed in 10 pure apocrine carcinomas (32%) and 8 apocrine-like carcinomas (50%). Polysomy 17 was seen without HER-2/neu gene amplification in 8 cases (Figure 2c) and with HER-2/neu gene amplification in 10 cases. The polysomy 17 rate was low: mean 3.55 CEP17 signals; (range: 3.0–6.0). Two pure apocrine carcinomas and three apocrine-like carcinomas (5 of 8, 63%) with polysomy 17 alone had Her-2/neu protein expression scores of 2 to 3+ by immunohistochemistry.
EGFR Expression in Apocrine Carcinomas
In all, 34 out of 55 (62%) cases expressed EGFR protein (scores 1 to 3+). A significantly higher proportion of pure apocrine carcinomas was positive for EGFR protein in comparison with the apocrine-like carcinoma subgroups (76 vs 29%, P=0.006) (Figure 1h). A diffuse (>50% of positive cells) and strong (intensity scores 2 to 3+) EGFR expression was seen in 20 of 29 (69%) of the pure apocrine carcinoma-positive cases and in 5 out of 5 (100%) of the apocrine-like carcinoma-positive cases.
EGFR gene amplification was a rare event present only in three (two pure apocrine and one apocrine-like tumors) of 44 studied cases (7%) (Figure 2b). All three cases exhibited EGFR protein overexpression. The average EGFR gene signal number per cell ranged from 1.6 to 20 (mean: 5.76).
Polysomy of chromosome 7 (defined as three or more copies of CEP7 signals per nucleus) was detected in 20 of 33 pure apocrine carcinomas (61%) and in 3 of 11 apocrine-like carcinomas (27%) either alone (21 cases) (Figure 2d) or in association with the EGFR gene amplification (two cases). Polysomy 7 was more frequently observed in the pure apocrine carcinoma subgroup compared with the apocrine-like carcinoma subgroup (P=0.083). Overall, the level of polysomy 7 was low (mean: 4.09, range: 3.0–7.06). A weak positive correlation between polysomy 7 and the EGFR protein expression was also present (P=0.025, r=0.326).
Chromosomal Analysis Using Conventional Cytogenetics and SNP Array Assay
Corroborative genetic evidence for FISH results was obtained in three cases, which were further studied by conventional cytogenetics and SNP arrays. One case of pure apocrine carcinoma (displaying polysomy 7 (4.37 CEP7 copies on average) and HER-2/neu gene amplification) was analyzed by conventional cytogenetic analysis (see Acknowledgement) and showed complex cytogenetic alterations (Figure 3) described as: 65–69,XXX,+i(1)(q10),−2,−3,add(3)(p12),add(6) (q27),+7,−8,−10,−11,add(11)(p15),add(11)(q23),−12,−13,add(14)(p11.2),−15,+16,−17,−18,−19,add(19)(q13.4),−520,−21,−22,+mar1,+mar2,+mar3,+mar4,+mar5,+5-8mar[5]/130–138, idemx2[2]/46,XX[13]. Another two cases (one pure apocrine carcinoma and one apocrine-like carcinoma, both with HER-2/neu gene amplification) were studied by SNP arrays, which confirmed FISH results and further revealed amplification of CEP17 without polysomy 17 in the first one, whereas the second one (Sample GLID09_0050) had coamplification of HER-2/neu and TOP2A along with a gain of CEP17 (Figure 4).
SNP array karyotypes of chromosome 17 for two samples with amplification of HER-2/neu. The first one (Sample GLID09_0048) had amplification of both CEP17 and HER-2/neu amplification without polysomy 17, whereas the second one (Sample GLID09_0050) had coamplification of HER-2/neu and TOP2A along with a gain of CEP17. Plots are as follows: (A) the raw log 2 ratio of tumor/normal for each probe on the array; (B) smoothing average over 10 probes; and (C) Hidden Markov Model of copy number with aqua=1, yellow=2, pink=3, pink-red=4, red-pink=5 and red >5.
Molecular Subclassification of Carcinomas with Apocrine Morphology
We found a statistically significant inverse correlation between EGFR and Her-2/neu expression in the pure apocrine carcinoma subgroup (P=0.006, r=−0.499). Therefore, 20 of 37 (54%) pure apocrine carcinoma cases can be classified as HER-2-overexpressing, whereas the remaining 17 cases (46%) as triple-negative breast carcinomas. In all, 16 out of 17 triple-negative pure apocrine carcinomas (94%) overexpressed EGFR and would accordingly be classified as basal-like breast carcinomas29 (Table 2). None of the pure apocrine carcinomas fulfilled the criteria for luminal tumors.29, 30, 31
In contrast, a large proportion of apocrine-like carcinomas belonged to the luminal group (13 of 17 cases, 76%). Only three cases (18%) could be classified as triple-negative breast carcinomas and one case only as HER-2-overexpressing breast carcinoma.
Discussion
The diagnosis of apocrine carcinoma of the breast has been controversial because of the lack of strict diagnostic criteria. With the increasing use of immunohistochemistry, apocrine breast cancer differentiation has shown a consistent pattern of steroid receptor expression irrespective of grade8 and this method should be applied for unequivocal definition of this special carcinoma type. With such consistency, additional correlations between the histological phenotype and biological potential become more meaningful.
In this study, we applied strict morphological and immunohistochemical criteria to correctly classify and characterize apocrine carcinoma of the breast. Consequently, our results clearly separated breast tumors with apocrine cytomorphology into two different groups: the pure apocrine carcinomas with consistent lack of ER and overexpression of AR, and morphologically apocrine-like carcinomas that did not exhibit the protein expression profile associated with the true apocrine phenotype.4, 5, 13, 32 Similarly, Celis et al8 using another set of morphological and immunohistochemical criteria for classification of apocrine carcinoma defined and confirmed the existence of a distinct apocrine carcinoma group with a consistent steroid receptor profile (ER−, AR+). Together, these results strongly support the recent advances in molecular classification of breast carcinoma that have revealed the existence of a specific ‘molecular apocrine’ gene expression profile among ER-negative breast carcinomas characterized primarily by increased AR signaling, along with a common Her-2/neu gene amplification.13 The pure apocrine carcinoma subgroup from our study seems to be equivalent to the ‘molecular apocrine’ group from Farmers’ study although that cohort was not entirely compatible with pure apocrine carcinomas.13 Our findings showing coexpression of AR and Her-2/neu proteins in pure apocrine carcinomas also support results of other studies that highlighted a functional cross-talk and association between AR and HER-2/neu in a subset of breast carcinomas and breast carcinoma cell lines.17, 33
Pure apocrine carcinomas were further characterized by nearly mutually exclusive expression of Her-2/neu and EGFR proteins. Thus, a majority of HER-2-negative cases (that is, triple-negative apocrine carcinomas) overexpressed EGFR and accordingly could be classified as basal-like breast carcinomas.29, 30, 31 On the other hand, HER-2-overexpressing pure apocrine carcinomas were mostly negative for EGFR protein expression.
The apocrine-like carcinomas were much more heterogeneous with various combinations of steroid receptor expression including AR. Apocrine-like carcinomas are characterized by a common ER expression and HER-2/neu gene amplification but significantly less common EGFR overexpression, thus mainly belonging to the luminal phenotypes (A and B) according to the molecular classification of breast carcinomas.30, 31 It is noteworthy that of the remaining four ER-negative apocrine-like carcinomas, only one case had HER-2/neu gene amplification.
Our results suggest that a strict definition of pure apocrine carcinomas could clarify some of the previous contradictions in the classification of apocrine carcinoma (variable and heterogeneous gene expression profiles of morphologically defined apocrine tumors) leading some investigators to challenge its existence.18
Overexpression of Her-2/neu protein has been reported in up to 25% of invasive breast carcinomas and has been associated with a worse clinical outcome.34 In most cases, this can be attributed to amplification of the HER-2/neu gene located on the long arm of chromosome 17 (17q12).35 Our study revealed HER-2/neu gene amplification in ∼52% of the cases, similar to the rate of HER-2/neu gene amplification in invasive apocrine carcinomas of the breast observed in two previously published small cohorts (44 and 50%, Moinfar et al12 and Varga et al,36 respectively). The pure apocrine carcinoma subgroup exhibited slightly higher rate of HER-2/neu gene amplification in comparison with the apocrine-like carcinoma subgroup, but the difference was not statistically significant. This is in line with previous studies, which demonstrated a strong association between HER-2/neu status and apocrine differentiation.13, 37 Although we found a high degree of concordance between immunohistochemistry and FISH results, four cases were negative for HER-2/neu gene amplification despite high protein expression on immunohistochemistry, which was previously explained by various preanalytical and analytical factors including tissue fixation, a choice of the anti-Her-2/neu antibody and scoring system.37, 38
Aneusomy 17, including polysomy 17, has been a common observation in breast carcinomas,39, 40 although the definition of polysomy 17 is not universally defined.24 Therefore, we followed the arbitrary cutoff of three or more copies of CEP17 applied in previous publications.22, 25, 26 Our FISH analysis revealed polysomy 17 in a proportion of apocrine carcinomas, either as the sole finding or in combination with HER-2/neu gene amplification. CEP17 polysomy without concomitant HER-2/neu gene amplification was seen in eight cases of which five had Her-2/neu protein overexpression (scores 2+ and 3+). Several investigators previously considered polysomy 17 a potential cause of equivocal HER-2/neu results by FISH or immunohistochemistry.25 However, Vanden Bempt et al22 found neither increased Her-2/neu protein nor increased HER-2 mRNA in polysomy 17 cases and concluded that the tumors displaying unamplified polysomy 17 probably represented more Her-2/neu-negative than Her-2/neu-positive breast tumors. Some investigators recently questioned the interpretation of the CEP17 copy number as a reliable predictor of the entire chromosome 17 polysomy,41 and our whole genome analysis using SNP arrays in two cases also supports this observation.
EGFR is a 170-kDa transmembrane glycoprotein encoded by the HER-1 protooncogene, located at 7p11.2-p12.42 High expression of EGFR in a variety of epithelial tumors has led to the development of a number of drugs specifically targeting the EGFR that are now in use for treatment of advanced colorectal carcinoma, non-small cell lung carcinoma, head and neck squamous cell carcinoma and pancreatic carcinoma.43 EGFR protein expression has also been a common finding in breast carcinoma, particularly in a subgroup of triple-negative, basal-like breast carcinomas (>50%) leading some investigators to use it as a surrogate marker for a basal-like breast carcinoma.29 However, EGFR gene alterations (activating mutations and gene amplification) tend to be a rare event in breast carcinoma and were found in <8% of the cases.44, 45 In this study, we demonstrated EGFR protein expression in 62% of the cases. The expression pattern was predominantly strong (scores 2 to 3+) and diffuse (>50% of positive cells) in both subgroups and was not accompanied by the EGFR gene amplification, similar to the results of a study by Park et al.45 Polysomy of chromosome 7 (CEP7), which we found associated with the pure apocrine carcinoma subgroup, is a novel finding, not previously associated with apocrine breast cancer.46, 47, 48, 49 It also correlated and might be responsible for the EGFR protein overexpression in the pure apocrine carcinoma.
In summary, our study indicates that breast carcinomas with apocrine differentiation are heterogeneous in molecular terms. The combination of morphological and immunohistochemical criteria are essential for the proper identification of pure apocrine carcinomas. When strictly defined, these carcinomas express either Her-2/neu or EGFR in a nearly exclusive manner, resulting in their classification as either HER-2-overexpressing or triple-negative types of breast carcinomas. In contrast, apocrine-like carcinomas predominantly belong to the luminal molecular phenotype (both A and B). Our findings also demonstrate that EGFR and HER-2/neu have important roles in the pathogenesis of apocrine carcinomas and these findings may have significant therapeutic implications.
References
O’Malley FP, Bane A . An update on apocrine lesions of the breast. Histopathology 2008;52:3–10.
Celis JE, Gromova I, Gromov P, et al. Molecular pathology of breast apocrine carcinomas: a protein expression signature specific for benign apocrine metaplasia. FEBS Lett 2006;580:2935–2944.
Tavassoli FA, Devilee P, (eds). World Health Organization Classificaiton of Tumours. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. IARC Press: Lyon, 2003.
Gatalica Z . Immunohistochemical analysis of apocrine breast lesions. Consistent over-expression of androgen receptor accompanied by the loss of estrogen and progesterone receptors in apocrine metaplasia and apocrine carcinoma in situ. Pathol Res Pract 1997;193:753–758.
Tavassoli FA, Purcell CA, Bratthauer GL, et al. Androgen receptor expression along with loss of bcl-2, ER, and PR expression in benign and malignant apocrine lesions of the breast: implications for therapy. Breast J 1996;2:261–269.
Leal C, Henrique R, Monteiro P, et al. Apocrine ductal carcinoma in situ of the breast: histologic classification and expression of biologic markers. Hum Pathol 2001;32:487–493.
Masood S, Rosa M . The challenge of apocrine proliferations of the breast: a morphologic approach. Pathol Res Pract 2009;205:155–164.
Celis JE, Cabezon T, Moreira JM, et al. Molecular characterization of apocrine carcinoma of the breast: Validation of an apocrine protein signature in a well-defined cohort. Mol Oncol 2009;3:220–237.
Nicolás Díaz-Chico B, Germán Rodríguez F, González A, et al. Androgens and androgen receptors in breast cancer. J Steroid Biochem Mol Biol 2007;105:1–15.
Isola JJ . Immunohistochemical demonstration of androgen receptor in breast cancer and its relationship to other prognostic factors. J Pathol 1993;170:31–35.
Bratthauer GL, Lininger RA, Man YH, et al. Androgen and estrogen receptor mRNA status in apocrine carcinomas. Diagn Mol Pathol 2002;11:113–118.
Moinfar F, Okcu M, Tsybrovskyy O, et al. Androgen receptors frequently are expressed in breast carcinomas. Cancer 2003;98:703–711.
Farmer P, Bonnefoi H, Becette V, et al. Identification of molecular apocrine breast tumours by microarray analysis. Oncogene 2005;24:4660–4671.
Doane AS, Danso M, Lal P, et al. An estrogen receptor-negative breast cancer subset characterized by a hormonally regulated transcriptional program and response to androgen. Oncogene 2006;25:3994–4008.
Kreike B, van Kouwenhove M, Horlings H, et al. Gene expression profiling and histopathological characterization of triple-negative/basal-like breast carcinomas. Breast Cancer Res 2007;9:404.
Sanga S, Broom BM, Cristini V, et al. Gene expression meta-analysis supports existence of molecular apocrine breast cancer with a role for androgen receptor and implies interactions with ErbB family. BM Med Genomics 2009;2:59.
Naderi A, Hughes-Davies L . A functionally significant cross-talk between androgen receptor and erbB2 pathways in estrogen receptor negative breast cancer. Neoplasia 2008;10:542–548.
Weigelt B, Horlings HM, Kreike B, et al. Refinement of breast cancer classification by molecular characterization of histological special types. J Pathol 2008;216:141–150.
Kaya H, Bozkurt SU, Erbarut I, et al. Apocrine carcinomas of the breast in Turkish women: hormone receptors, c-erbB-2 and p53 immunoexpression. Pathol Res Pract 2008;204:367–371.
Matsuo K, Fukutomi T, Hasegawa T, et al. Histological and immunohistochemical analysis of apocrine breast carcinoma. Breast Cancer 2002;9:43–49.
Chan SK, Hill ME, Gullick WJ . The role of the epidermal growth factor receptor in breast cancer. J Mammary Gland Biol Neoplasia 2006;11:3–11.
Vanden Bempt I, Van Loo P, Drijkoningen M, et al. Polysomy 17 in breast cancer: clinicopathologic significance and impact on HER-2 testing. J Clin Oncol 2008;26:4869–4874.
Honma N, Sakamoto G, Akiyama F, et al. Breast carcinoma in women over the age of 85: distinct histological pattern an androgen, oestrogen, and progesterone receptor status. Histopathology 2003;42:120–127.
Wolff AC, Hammond ME, Schwartz JN, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 2007;25:118–145.
Krishnamurti U, Hammers JL, Atem FD, et al. Poor prognostic significance of unamplified chromosome 17 polysomy in invasive breast carcinoma. Mod Pathol 2009;22:1044–1048.
Varshney D, Zhou YY, Geller SA, et al. Determination of HER-2 status and chromosome 17 polysomy in breast carcinomas comparing HercepTest and PathVysion FISH assay. Am J Clin Pathol 2004;121:70–77.
Lyons-Weiler M, Hagenkord J, Sciulli CM, et al. Optimization of the Affymetrix GeneChip mapping 10 K 2.0 assay for routine clinical use on formalin fixed paraffin embedded tissues. Diagn Mol Pathol 2008;17:3–13.
Monzon FA, Hagenkord J, Lyons-Weiler M, et al. Whole genome SNP arrays as a potential diagnostic tool for the detection of characteristic chromosomal aberrations in renal epithelial tumors. Mod Pathol 2008;21:599–608.
Nielsen TO, Hsu FD, Jensen K, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 2004;10:5367–5374.
Sørlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 2001;98:10869–10874.
Perou CM, Sørlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 2000;406:747–752.
Moe RE, Anderson BO . Androgens and androgen receptors: a clinically neglected sector in breast cancer biology. J Surg Oncol 2007;95:437–439.
Agoff SN, Swanson PE, Linden H, et al. Androgen receptor expression in estrogen receptor-negative breast cancer. Immunohistochemical, clinical, and prognostic associations. Am J Clin Pathol 2003;120:725–731.
Slamon D, Clark G, Wong S, et al. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987;235:177–182.
Sauter G, Lee J, Bartlett JM, et al. Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodologic considerations. J Clin Oncol 2009;27:1323–1333.
Varga Z, Zhao J, Öhlschlegel C, et al. Preferential HER-2/neu overexpression and/or amplification in aggressive histological subtypes of invasive breast cancer. Histopathology 2004;44:332–338.
Bhargava R, Striebel J, Beriwal S, et al. Prevalence, morphologic features and proliferation indices of breast carcinoma molecular classes using immunohistochemical surrogate markers. Int J Clin Exp Pathol 2009;2:444–455.
Gown AM, Goldstein LC, Barry TS, et al. High concordance between immunohistochemistry and fluorescence in situ hybridization testing for HER2 status in breast cancer requires a normalized IHC scoring system. Mod Pathol 2008;21:1271–1277.
Watters AD, Going JJ, Cooke TG, et al. Chromosome 17 aneusomy is associated with poor prognostic factors in invasive breast carcinoma. Breast Cancer Res Treat 2003;77:109–114.
Wang S, Saboorian MH, Frenkel EP, et al. Aneusomy 17 in breast cancer: Its role in HER-2/neu protein expression and implication for clinical assessment of HER-2/neu status. Mod Pathol 2002;15:137–145.
Yeh IT, Martin MA, Robetorye RS, et al. Clinical validation of an array CGH test for HER2 status in breast cancer reveals that polysomy 17 is a rare event. Mod Pathol 2009;22:1169–1175.
Hynes NE, Lane HA . ERBB receptors and cancer: the complexity of targeted inhibitors. Nature Rev Cancer 2005;5:341–354.
Laurent-Puig P, Lievre A, Blons H . Mutations and response to epidermal growth factor receptor inhibitors. Clin Cancer Res 2009;15:1133–1139.
Bhargava R, Gerald WL, Li AR, et al. EGFR gene amplification in breast cancer: correlation with epidermal growth factor receptor mRNA and protein expression and HER-2 status and absence of EGFR-activating mutations. Mod Pathol 2005;18:1027–1033.
Park K, Han S, Shin E, et al. EGFR gene and protein expression in breast cancers. Euro J Surg Oncol 2007;33:956–960.
Corzo C, Tusquets I, Salido M, et al. Characterization of HER1 (c-erbB1) status in locally advanced breast cancer using fluorescence in situ hybridization and immunohistochemistry. Tumour Biol 2005;26:25–30.
Kapranos N, Kounelis S, Karantasis H, et al. Numerical aberrations of chromosomes 1 and 7 by fluorescent in situ hybridization and DNA ploidy analysis in breast cancer. Breast J 2005;11:448–453.
Sauer T, Beraki K, Jebsen PW, et al. Numerical abnormalities of chromosome 7 in interphase cell nuclei of breast carcinoma have no impact on immunohistochemically determined EGFR status. APMIS 1999;107:211–216.
Gwin K, Lezon-Geyda K, Harris L, et al. Chromosome 7 aneusomy in metaplastic breast carcinomas with chondroid, squamous, and spindle-cell differentiation. Int J Surg Pathol 2009; doi:10.1177/1066896909334127.
Acknowledgements
The conventional cytogenetic study was performed at the Human Genetics Laboratory, Munroe Meyer Institute, University of Nebraska Medical Center, Omaha, NE, USA; we thank Dr Warren Sanger, Dr Julia Bridge and Ms Marilu Nelson for the excellent report and providing us with the Figure 3. We are also indebted to Kay M Krogman, Department of Pathology, Creighton University School of Medicine, for technical assistance. Dr Semir Vranic was a research fellow at the Creighton University Medical Center, Omaha, NE, USA, and had been supported by the UICC American Cancer Society Beginning Investigators Fellowship (ACSBI) award (ACS/08/004) funded by the American Cancer Society. The preliminary results of the study were presented at the 96th Annual Meeting of the United States and Canadian Academy of Pathology, San Diego, CA, USA, 2007.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vranic, S., Tawfik, O., Palazzo, J. et al. EGFR and HER-2/neu expression in invasive apocrine carcinoma of the breast. Mod Pathol 23, 644–653 (2010). https://doi.org/10.1038/modpathol.2010.50
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.50
Keywords
This article is cited by
-
Apocrine lesions of the breast
Virchows Archiv (2022)
-
HER2-positive apocrine carcinoma of the breast: a population-based analysis of treatment and outcome
Breast Cancer Research and Treatment (2022)
-
Triple-negative apocrine carcinoma as a rare cause of a breast lump in a Syrian female: a case report and review of the literature
BMC Women's Health (2021)
-
Metastatic colon cancer of the small intestine diagnosed using genetic analysis: a case report
Diagnostic Pathology (2020)
-
Androgen Receptor-Targeted Therapy for Breast Cancer
Current Breast Cancer Reports (2017)