Abstract
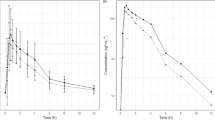
Cytochrome P450s (CYPs) are an important family of enzymes in the metabolism of many therapeutic agents and endogenous metabolic reactions. The CYP3A subfamily is especially prominent in these metabolic activities. This review article focuses on how the factors of age and sex may influence the in vivo activity of human CYP3A. The functional activity of CYP3A varies based on issues such as interaction with one or more substrates and between individuals and/or localisation. For CYP3A substrates, intrinsic clearance is the component of total clearance that is contributed by the enzymes. Depending on the route of administration and the contribution of hepatic blood flow to overall clearance, sensitivities to changes in CYP3A activities may differ. Additionally, age may influence the hepatic blood flow and, in turn, affect CYP3A activity. A review of the literature regarding age influences on the clearance of CYP3A substrates does suggest that age can affect the clearance of certain CYP3A substrates.
CYP3A is responsible for a large number of endogenous metabolic reactions involving steroid hormones, and enzyme activity has been reported to be induced and/or inhibited in the presence of some sex steroids. Based on published studies for most CYP3A substrates, sex does not appear to influence clearance; however, with certain substrates significant sex-related differences are found. In such cases, women primarily have higher clearance than men.





Similar content being viewed by others
References
Guengerich FP. Catalytic selectivity of human cytochrome P450 enzymes: relevance to drug metabolism and toxicity. Toxicol Lett 1994; 70: 133–8
Venkatakrishnan K, von Moltke LL, Greenblatt DJ. Human drug metabolism and the cytochromes P450: application and relevance of in vitro models. J Clin Pharmacol 2001; 41: 1149–79
Guengerich FP. Cytochrome P-450 3A4: regulation and role in drug metabolism. Annu Rev Pharmacol Toxicol 1999; 39: 1–7
Shimada T, Yamazaki H, Mimura M, et al. Interindividual variations in human liver cytochrome P-450 enzymes involved in the oxidation of drugs, carcinogens and toxic chemicals: studies with liver microsomes of 30 Japanese and 30 Caucasians. J Pharmacol Exp Ther 1994; 270: 414–23
Smith DA, Abel SM, Hyland R, et al. Human cytochrome P450s: selectivity and measurement in vivo. Xenobiotica 1998; 28: 1095–128
Clarke SE. In vitro assessment of human cytochrome P450. Xenobiotica 1998; 28: 1167–202
Smith G, Stubbins MJ, Harries LW, et al. Molecular genetics of the human cytochrome P450 monooxygenase superfamily. Xenobiotica 1998; 28: 1129–65
Watkins PB, Wrighton SA, Schuetz EG, et al. Identification of glucocorticoid-inducible cytochromes P450 in the intestinal mucosa of rats and man. J Clin Invest 1987; 80: 1029–36
Lown KS, Kolars JC, Thummel KE, et al. Interpatient heterogeneity in expression of CYP3A4 and CYP3A5 in small bowel: lack of prediction by the erythromycin breath test. Drug Metab Dispos 1994; 22: 947–55
Paine MF, Khalighi M, Fisher JM, et al. Characterization of interintestinal and intraintestinal variations in human CYP3A-dependent metabolism. J Pharmacol Exp Ther 1997; 283: 1552–62
Lown KS, Ghosh M, Watkins PB. Sequences of intestinal and hepatic cytochrome P450 3A4 cDNAs are identical. Drug Metab Dispos 1998; 26: 185–7
Watkins PB, Wrighton SA, Maurel P, et al. Identification of an inducible form of cytochrome P-450 in human liver. Proc Natl Acad Sci U S A 1985; 82: 6310–4
Wrighton SA, Molowa DT, Guzelian PS. Identification of a cytochrome P-450 in human fetal liver related to glucocorticoid-inducible cytochrome P-450HLp in the adult. Biochem Pharmacol 1988; 37: 3053–5
Komori M, Kishio K, Ohi H, et al. Molecular cloning and sequence analysis of cDNA containing the entire coding sequence region for human fetal liver cytochrome P-450. J Biochem 1989; 105: 161–3
Domanski TL, Finta C, Halpert JR, et al. CDNA cloning and initial characterization of CYP3A43, a novel human cytochrome P450. Mol Pharmacol 2001; 59: 386–92
Aoyama T, Yamano S, Waxman DJ, et al. Cytochrome P450 hPCN3, a novel cytochrome P-450 IIIA gene product that is differentially expressed in adult human liver. J Biol Chem 1989; 264: 10388–95
Wrighton SA, Ring BJ, Watkins PB, et al. Identification of a polymorphically expressed member of the human cytochrome P-450III family. Mol Pharmacol 1989; 36: 97–105
Wrighton SA, Brain WR, Sari M-A, et al. Studies on the expression and metabolic capabilities of human liver cytochrome P450IIIA5 (HLp3). Mol Pharmacol 1990; 38: 207–13
Gibbs MA, Thummel KE, Shen DD, et al. Inhibition of cytochrome P-450 (CYP3A) in human intestinal and liver microsomes: comparison of KI values and impact of CYP3A5 expression. Drug Metab Dispos 1999; 27: 180–7
Hirota N, Ito K, Iwatsubo T, et al. In vitro/in vivo scaling of alprazolam metabolism by CYP3A4 and CYP3A5 in humans. Biopharm Drug Dispos 2001; 22: 53–71
Kuehl P, Zhang J, Lin Y, et al. Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet 2001; 27: 383–91
Schuetz JD, Kauma S, Guzelian PS. Identification of the fetal liver cytochrome CYP3A7 in human endometrium and placenta. J Clin Invest 1993; 92: 1018–24
Lin JH, Lu AY. Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet 1998; 35: 361–90
Thummel KE, Wilkinson GR. In vitro and in vivo drug interactions involving human CYP3A. Annu Rev Pharmacol Toxicol 1998; 38: 389–430
Venkatakrishnan K, von Moltke LL, Greenblatt DJ. Effects of the antifungal agents on oxidative drug metabolism: clinical relevance. Clin Pharmacokinet 2000; 38: 111–80
Halpert JR. Structural basis of selective cytochrome P450 inhibition. Annu Rev Pharmacol Toxicol 1995; 35: 29–53
von Moltke LL, Greenblatt DJ, Grassi JM, et al. Protease inhibitors as inhibitors of human cytochromes P450: high risk associated with ritonavir. J Clin Pharmacol 1998; 38: 106–11
Bailey DG, Malcom J, Arnold O, et al. Grapefruit juice: drug interactions. Br J Clin Pharmacol 1998; 46: 101–10
Ameer B, Weintraub RA. Drug interactions with grapefruit juice. Clin Pharmacokinet 1997; 33: 103–21
Greenblatt DJ, Patki KC, von Moltke LL, et al. Drag interactions with grapefruit juice: an update. J Clin Psychopharmacol 2001; 21: 357–9
Lown KS, Bailey DG, Fontana RJ, et al. Grapefruit juice increases felodipine oral availability in humans by decreasing intestinal CYP3A protein expression. J Clin Invest 1997; 99: 2545–53
Schmiedlin-Ren P, Edwards DJ, Fitzsimmons ME, et al. Mechanisms of enhanced oral availability of CYP3A4 substrates by grapefruit constituents: decreased enterocyte CYP3A4 concentration and mechanism-based inactivation by furanocoumarins. Drag Metab Dispos 1997; 25: 1228–33
Fukuda K, Ohta T, Oshima Y, et al. Specific CYP3A4 inhibitors in grapefruit juice: furocoumarin dimers as components of drug interaction. Pharmacogenetics 1997; 7: 391–6
Bailey DG, Kreeft JH, Munoz C, et al. Grapefruit juicefelodipine interaction: effect of naringin and 6′,7′-dihydroxybergamottin in humans. Clin Pharmacol Ther 1998; 64: 248–56
Bertilsson L. Geographical/interracial differences in polymorphic drag oxidation: current state of knowledge of cytochromes P450 (CYP) 2D6 and 2C19. Clin Pharmacokinet 1995; 29: 192–209
Bertilsson L, Dahl M-L. Polymorphic drag oxidation. CNS Drugs 1996; 3: 200–23
Nebert DW. Polymorphisms in drag-metabolizing enzymes: what is their clinical relevance and why do they exist? Am J Hum Genet 1997; 60: 265–71
Paulussen A, Lavrijsen K, Bohets H, et al. Two linked mutations in transcriptional regulatory elements of the CYP3A5 gene constitute the major genetic determinant of polymorphic activity in humans. Pharmacogenomics 2000; 10: 415–24
Hustert E, Haberl M, Burk O, et al. The genetic determinants of the CYP3A5 polymorphism. Pharmacogenomics 2001; 11: 773–9
Fukuen S, Fukuda T, Maune H, et al. Novel detection assay by PCR-RFLP and frequency of the CYP3A5 SNPs, CYP3A5*3 and *6, in a Japanese population. Pharmacogenomics 2002; 12: 331–4
Watkins PB. Noninvasive tests of CYP3A enzymes. Pharmacogenetics 1994; 4: 171–84
Streetman DS, Bertino JS, Nafziger AN. Phenotyping of drug metabolizing enzymes in adults: a review of in-vivo cytochrome P450 phenotyping probes. Pharmacogenetics 2000; 10: 187–216
Kronbach T, Mathys D, Umeno M, et al. Oxidation of midazolam and triazolam by human liver cytochrome P450IIIA4. Mol Pharmacol 1989; 36: 89–96
Gorski JC, Hall SD, Jones DR, et al. Regioselective biotransformation of midazolam by members of the human cytochrome P450 3A (CYP3A) subfamily. Biochem Pharmacol 1994; 47: 1643–53
von Moltke LL, Greenblatt DJ, Schmider J, et al. Midazolam hydroxylation by human liver microsomes in vitro: inhibition by fluoxetine, norfluoxetine, and by azole antifungal agents. J Clin Pharmacol 1996; 36: 783–91
Perloff MD, von Moltke LL, Court MH, et al. Midazolam and triazolam biotransformation in mouse and human liver microsomes: relative contribution of CYP3A and CYP2C isoforms. J Pharmacol Exp Ther 2000; 292: 618–28
Tsunoda SM, Velez RL, von Moltke LL, et al. Differentiation of intestinal and hepatic cytochrome P450 3A activity with use of midazolam as an in vivo probe: effect of ketoconazole. Clin Pharmacol Ther 1999; 66: 461–71
Thummel KE, O’shea D, Paine MF, et al. Oral first-pass elimination of midazolam involves both gastrointestinal and hepatic CYP3A-mediated metabolism. Clin Pharmacol Ther 1996; 59: 491–502
Hebert MF, Roberts JP, Praeksaritanont T, et al. Bioavailability of cyclosporine with concomitant rifampin administration is markedly less than predicted by hepatic enzyme induction. Clin Pharmacol Ther 1992; 52: 453–7
Thummel KE, Shen DD, Podoll TD, et al. Use of midazolam as a human cytochrome P450 3A probe. I: in vitro-in vivo correlations in liver transplant patients. J Pharmacol Exp Ther 1994; 271: 549–56
Thummel KE, Shen DD, Podoll TD, et al. Use of midazolam as a human cytochrome P450 3A probe. II: characterization of inter- and intraindividual hepatic CYP3A variability after liver transplantation. J Pharmacol Exp Ther 1994; 271: 557–66
Gomez DY, Wacher VJ, Tomlanovich SJ, et al. The effects of ketoconazole on the intestinal metabolism and bioavailability of cyclosporine. Clin Pharmacol Ther 1995; 58: 15–9
Paine MF, Shen DD, Kunze KL, et al. First-pass metabolism of midazolam by the human intestine. Clin Pharmacol Ther 1996; 60: 14–24
Gorski JC, Jones DR, Haehner-Daniels BD, et al. The contribution of intestinal and hepatic CYP3A to the interaction between midazolam and clarithromycin. Clin Pharmacol Ther 1998; 64: 133–43
Wu CY, Benet LZ, Hebert MF, et al. Differentiation of absorption and first-pass gut and hepatic metabolism in humans: studies with cyclosporine. Clin Pharmacol Ther 1995; 58: 492–7
Hall SD, Thummel KE, Watkins PB, et al. Molecular and physical mechanisms of first-pass extraction. Drug Metab Dispos 1999; 27: 161–6
McIntosh JF, Moller I, van Slyke DD. Studies of urea clearance. III: the influence of the body size on urea output. J Clin Invest 1928; 6: 467–83
Wilkinson GR. Clearance approaches in pharmacology. Pharmacol Rev 1987; 39: 1–47
Chen CJ, Chin JE, Ueda K, et al. Internal duplication and homology with bacterial transport proteins in the MDR1 (P-glycoprotein) gene from multidrug-resistant human cells. Cell 1986; 47: 381–9
Roninson IB, Chin JE, Choi KG, et al. Isolation of human MDR DNA sequences amplified in multidrug-resistant KB carcinoma cells. Proc Natl Acad Sci U S A 1986; 83: 4538–42
Biedler JL, Riehm H. Cellular resistance to actinomycin D in Chinese hamster cells in vitro: cross-resistance, radioautographic and cytogenetic studies. Cancer Res 1970; 30:1174–84
Kessel D, Bosmann HB. On the characteristics of actinomycin D resistance in L5178Y cells. Cancer Res 1970; 30: 2695–701
Juliano R, Ling V. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim Biophys Acta 1976; 455: 152–62
Wacher VJ, Wu C, Benet LZ. Overlapping substrate specificities and tissue distribution of cytochrome P450 3A and P-glycoprotein: implications for drug delivery and activity in cancer chemotherapy. Mol Carcinog 1995; 13: 129–34
Yu DK. The contribution of p-glycoprotein to pharmacokinetic drug-drag interactions. J Clin Pharmacol 1999; 39: 1203–11
Schuetz EG, Furuya KN, Schuetz JD. Interindividual variation in expression of p-glycoprotein in normal human liver and secondary hepatic neoplasms. J Pharmacol Exp Ther 1995; 275: 1011–8
Lown KS, Mayo RR, Leichtman AB, et al. Role of intestinal p-glycoprotein (MDR1) in interpatient variation in the oral bioavailability of cyclosporine. Clin Pharmacol Ther 1997; 62: 248–60
Kim RB, Fromm MF, Wandel C, et al. The drag transporter p-glycoprotein limits oral absorption and brain entry of HIV-1 protease inhibitors. J Clin Invest 1998; 101: 289–94
Koudriakova T, Iatsimirskaia E, et al. Metabolism of the human immunodeficiency virus protease inhibitors indinavir and ritonavir by human intestinal microsomes and expressed cytochrome P4503A4/3A5: mechanism-based inactivation of cytochrome P4503A by ritonavir. Drug Metab Dispos 1998; 26: 552–61
Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest 1950; 29: 496–507
Abernethy DR. Aging effects on drag disposition and effect. Geriatr Nephrol Urol 1999; 9: 15–9
Wynne HA, Cope LH, Mutch E, et al. The effect of age upon liver volume and apparent liver blood flow in healthy man. Hepatology 1989; 9: 297–301
Le Couteur DG, McLean AJ. The aging liver: drag clearance and an oxygen diffusion barrier hypothesis. Clin Pharmacokinet 1998; 34: 359–73
Zoli M, Magalotti D, Bianchi G, et al. Total and functional hepatic blood flow decrease in parallel with ageing. Age Ageing 1999; 28: 29–33
Herrlinger C, Klotz U. Drug metabolism and drug interactions in the elderly. Best Pract Res Clin Gastroenterol 2001; 15: 897–918
Greenblatt DJ, Sellers EM, Shader RI. Drug disposition in old age. N Engl J Med 1982; 306: 1081–7
Kyle UG, Genton L, Hans D, et al. Total body mass, fat mass, fat-free mass, and skeletal muscle in older people: crosssectional differences in 60-year-old persons. J Am Geriatr Soc 2001; 49: 1633–40
Borkan GA, Hults DE, Gerzof SG, et al. Age changes in body composition revealed by computed tomography. J Gerontol 1983; 38: 673–7
Vermeulen A, Goemaere S, Kaufman JM. Testosterone, body composition and aging. J Endocrinol Invest 1999; 22: 110–6
Greenblatt DJ, Allen MD, Harmatz JS, et al. Diazepam disposition determinants. Clin Pharmacol Ther 1980; 27: 301–12
Klotz U, Avant GR, Hoyumpa A, et al. The effects of age and liver disease on the disposition and elimination of diazepam in adult man. J Clin Invest 1975; 55: 347–59
Fleishaker JC, Hulst LK, Ekernäs S-Å, et al. Pharmacokinetics and pharmacodynamics of adinazolam and N-desmethy-ladinazolam after oral and intravenous dosing in healthy young and elderly volunteers. J Clin Psychopharmacol 1992; 12: 403–14
Lemmens HJM, Burm AGL, Hennis PJ, et al. Influence of age on the pharmacokinetics of alfentanil: gender dependence. Clin Pharmacokinet 1990; 19: 416–22
Scott JC, Stanski DR. Decreased fentanyl and alfentanil dose requirements with age: a simultaneous pharmacokinetic and pharmacodynamic evaluation. J Pharmacol Exp Ther 1987; 240: 159–66
Greenblatt DJ, Divoll M, Abemethy DR, et al. Alprazolam kinetics in the elderly: relation to antipyrine disposition. Arch Gen Psychiatry 1983; 40: 287–90
Bertz RJ, Kroboth PD, Kroboth FJ, et al. Alprazolam in young and elderly men: sensitivity and tolerance to psychomotor, sedative and memory effects. J Pharmacol Exp Ther 1997; 281: 1317–29
Ochs HR, Greenblatt DJ, Friedman H, et al. Bromazepam pharmacokinetics: influence of age, gender, oral contraceptives, Cimetidine, and propranolol. Clin Pharmacol Ther 1987; 41: 562–70
Gammans RE, Westrick ML, Shea JP, et al. Pharmacokinetics of buspirone in elderly subjects. J Clin Pharmacol 1989; 29: 72–8
Cheng H, Rogers JD, Sweany AE, et al. Influence of age and gender on the plasma profiles of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitory activity following multiple doses of lovastatin and simvastatin. Pharm Res 1992; 9: 1629–33
Avram MJ, Fragen RJ, Caldwell NJ. Midazolam kinetics in women of two age groups. Clin Pharmacol Ther 1983; 34: 505–8
Greenblatt DJ, Abemethy DR, Locniskar A, et al. Effect of age, gender, and obesity on midazolam kinetics. Anesthesiology 1984; 61: 27–35
Holazo AA, Winkler MB, Patel IH. Effects of age, gender and oral contraceptives on intramuscular midazolam pharmacokinetics. J Clin Pharmacol 1988; 28: 1040–5
Albrecht S, Ihmsen H, Hering W, et al. The effect of age on the pharmacokinetics and pharmacodynamics of midazolam. Clin Pharmacol Ther 1999; 65: 630–9
Fleishaker JC, Pearson LK, Pearson PG, et al. Hormonal effects on tirilazad clearance in women: assessment of the role of CYP3A. J Clin Pharmacol 1999; 39: 260–7
Gorski JC, Wang Z, Haehner-Daniels BD, et al. The effect of hormone replacement therapy on CYP3A activity. Clin Pharmacol Ther 2000; 68: 412–7
Barbhaiya RH, Buch AB, Greene DS. A study of the effect of age and gender on the pharmacokinetics of nefazodone after single and multiple doses. J Clin Psychopharmacol 1996; 16: 915–23
Robertson DR, Waller DG, Renwick AG, et al. Age-related changes in the pharmacokinetics and pharmacodynamics of nifedipine. Br J Clin Pharmacol 1988; 25: 297–305
Mück W, Breuel HP, Kuhlmann J. The influence of age on the pharmacokinetics of nimodipine. Int J Clin Pharmacol Ther 1996; 34: 293–8
Lettieri JT, Krol GJ, Yeh SC, et al. The effects of age and race on nitrendipine pharmacokinetics and pharmacodynamics. J Cardiovasc Pharmacol 1988; 12: S129–S32
Harris RZ, Tsonoda SM, Mroczkowski P, et al. The effects of menopause and hormone replacement therapies on prednisolone and erythromycin pharmacokinetics. Clin Pharmacol Ther 1996; 59: 429–35
Greenblatt DJ, Friedman H, Burstein ES, et al. Trazodone kinetics: effect of age, gender, and obesity. Clin Pharmacol Ther 1987; 42: 193–200
Greenblatt DJ, Divoll M, Abernethy DR, et al. Reduced clearance of triazolam in old age: relation to antipyrine oxidizing capacity. Br J Clin Pharmacol 1983; 15: 303–9
Smith RB, Divoll M, Gillespie WR, et al. Effect of subject age and gender on the pharmacokinetics of oral triazolam and temazepam. J Clin Psychopharmacol 1983; 3: 172–6
Greenblatt DJ, Harmatz JS, Shapiro L, et al. Sensitivity to triazolam in the elderly. N Engl J Med 1991; 324: 1691–8
Robin DW, Hasan SS, Edeki T, et al. Increased baseline sway contributes to increased losses of balance in older people following triazolam. J Am Geriate Soc 1996; 44: 300–4
Abernethy DR, Schwartz JB, Todd EL, et al. Verapamil pharmacodynamics and disposition in young and elderly hypertensive patients: altered electrocardiographic and hypotensive responses. Ann Intern Med 1986; 105: 329–36
Sasaki M, Tateishi T, Ebihara A. The effects of age and gender on the stereoselective pharmacokinetics of verapamil. Clin Pharmacol Ther 1993; 54: 278–85
Schwartz JB, Capili H, Daugherty J. Aging of women alters S-verapamil pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther 1994; 55: 509–17
Fromm MF, Dilger K, Busse D, et al. Gut wall metabolism of verapamil in older people: effects of rifampicin-mediated enzyme induction. Br J Clin Pharmacol 1998; 45: 247–55
Olubodun JO, Ochs HR, von Moltke LL, et al. Pharmacokinetic properties of Zolpidem in elderly and young adults: possible modulation by testosterone in men. Br J Clin Pharmacol 2003 Sep; 56(3): 297–304
Helmers H, Van Peer A, Woestenborghs R, et al. Alfentanil kinetics in the elderly. Clin Pharmacol Ther 1984; 36: 239–43
Kaplan GB, Greenblatt DJ, Ehrenberg BL, et al. Single-dose pharmacokinetics and pharmacodynamics of alprazolam in elderly and young subjects. J Clin Pharmacol 1998; 38: 14–21
Elliott HL, Meredith PA, Reid JL, et al. A comparison of the disposition of single oral doses of amlodipine in young and elderly subjects. J Cardiovasc Pharmacol 1988; 12: S64–6
Gibson DM, Bron NJ, Richens A, et al. Effect of age and gender on pharmacokinetics of atorvastatin in humans. J Clin Pharmacol 1996; 36: 242–6
Chu S, Wilson DS, Guay DRP, et al. Clarithromycin pharmacokinetics in healthy young and elderly volunteers. J Clin Pharmacol 1992; 32: 1045–9
Schwartz JB, Abernethy DR. Responses to intravenous and oral diltiazem in elderly and younger patients with systemic hypertension. Am J Cardiol 1987; 59: 1111–7
Landahl S, Edgar B, Gabrielsson M, et al. Pharmacokinetics and blood pressure effects of felodipine in elderly hypertensive patients: a comparison with young healthy subjects. Clin Pharmacokinet 1988; 14: 374–83
Lind MJ, Margison JM, Cerny T, et al. The effect of age on the pharmacokinetics of ifosfamide. Br J Clin Pharmacol 1990; 30: 140–3
Harper KW, Collier PS, Dundee JW, et al. Age and nature of operation influence the pharmacokinetics of midazolam. Br J Anaesth 1985; 57: 866–71
Platten H-P, Schweizer E, Dilger K, et al. Pharmacokinetics and the pharmacodynamic action of midazolam in young and elderly patients undergoing tooth extraction. Clin Pharmacol Ther 1998; 63: 552–60
Baksi AK, Edwards JS, Ahr G. A comparison of the pharmacokinetics of nisoldipine in elderly and young subjects. Br J Clin Pharmacol 1991; 31: 367–70
Ochs HR, Greenblatt DJ, Woo E, et al. Reduced quinidine clearance in elderly persons. Am J Cardiol 1978; 42: 481–5
Hulst LK, Fleishaker JC, Peters GR, et al. Effect of age and gender on tirilazad pharmacokinetics in humans. Clin Pharmacol Ther 1994; 55: 378–84
Sotaniemi EA, Anttila MI. Influence of age on toremifene pharmacokinetics. Cancer Chemother Pharmacol 1997; 40: 185–8
Schwartz JB. Aging alters verapamil elimination and dynamics: single dose and steady-state responses. J Pharmacol Exp Ther 1990; 255: 364–73
Ahmed JH, Meredith PA, Elliott HL. The influence of age on the pharmacokinetics of verapamil. Pharmacol Res 1991; 24: 227–33
Schwartz JB, Troconiz IF, Verotta D, et al. Aging effects on stereoselective pharmacokinetics and pharmacodynamics of verapamil. J Pharmacol Exp Ther 1993; 265: 690–8
Gupta SK, Atkinson L, Tu T, et al. Age and gender related changes in stereoselective pharmacokinetics and pharmacodynamics of verapamil and norverapamil. Br J Clin Pharmacol 1995; 40: 325–31
Krecic-Shepard ME, Barnas CR, Slimko J, et al. Genderspecific effects on verapamil pharmacokinetics and pharmacodynamics in humans. J Clin Pharmacol 2000; 40: 219–30
Dundee JW, Collier PS, Carlisle RJT, et al. Prolonged midazolam elimination half-life. Br J Clin Pharmacol 1986; 21: 425–9
Kassai A, Toth G, Eichelbaum M, et al. No evidence of a genetic polymorphism in the oxidative metabolism of midazolam. Clin Pharmacokinet 1988; 15: 319–25
Scavone JM, Greenblatt DJ, Locniskar A, et al. Alprazolam pharmacokinetics in women on low-dose oral contraceptives. J Clin Pharmacol 1988; 28: 454–7
Tsuruo T, Iida H, Yamashiro M, et al. Enhancement of vincristine- and adriamycin-induced cytotoxicity by verapamil in P388 leukemia and its sublines resistant to vincristine and adriamycin. Biochem Pharmacol 1982; 31: 3138–40
Haubermann K, Benz B, Gekeler V, et al. Effects of verapamil enantiomers and major metabolites on the cytotoxicity of vincristine and daunomycin in human lymphoma cell lines. Eur J Clin Pharmacol 1991; 40: 53–9
Nielsen TL, Rasmussen BB, Flinois J-P, et al. In vitro metabolism of quinidine: the (3S)-3-hydroxylation of quinidine is a specific marker reaction for cytochrome P-4503A4 activity in human liver microsomes. J Pharmacol Exp Ther 1999; 289: 31–7
Damkier P, Brsen K. Quinidine as a probe for CYP3A4 activity: intrasubject variability and lack of correlation with probebased assays for CYP1 A2, CYP2C9, CYP2C19, and CYP2D6. Clin Pharmacol Ther 2000; 68: 199–209
Yun CH, Wood M, Wood AJJ, et al. Identification of the pharmacogenetic determinants of alfentanil metabolism: cytochrome P450 3A4. Anesthesiology 1992; 77: 467–74
Labroo RB, Thummel KE, Kunze DL, et al. Catalytic role of cytochrome P4503A4 in multiple pathways of alfentanil metabolism. Drug Metab Dispos 1995; 23: 490–6
Guitton J, Buronfosse T, Desage M, et al. Possible involvement of multiple cytochrome P450S in fentanyl and sufentanil metabolism as opposed to alfentanil. Biochem Pharmacol 1997; 53: 1613–9
von Moltke LL, Greenblatt DJ, Granda BW, et al. Nefazodone, meta-chlorophenylpiperazine, and their metabolites in vitro: cytochromes mediating transformation, and P450-3A4 inhibitory actions. Psychopharmacology 1999; 145: 113–22
Zalma A, von Moltke LL, Granda BW, et al. In vitro metabolism of trazodone by CYP3A: inhibition by ketoconazole and human immunodeficiency viral protease inhibitors. Biol Psychiatry 2000; 47: 655–61
Walker D, Flinois JP, Monkman SC, et al. Identification of the major human hepatic cytochrome P450 involved in activation and N-dechloroethylation of ifosphamide. Biochem Pharmacol 1994; 47: 1157–61
Berthou F, Dreano Y, Belloc C, et al. Involvement of cytochrome P450 3A enzyme family in the major metabolic pathways of toremifene in human liver microsomes. Biochem Pharmacol 1994; 47: 1883–95
Christians U, Jacobsen W, Floren LC. Metabolism and drug interactions of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor in transplant patients: are the statins mechanistically similar. Pharmacol Ther 1998; 80: 1–34
Corsini A, Bellosta S, Baetta R, et al. New insights into the pharmacodynamic and pharmacokinetic properties of statins. Pharmacol Ther 1999; 84: 413–28
Igel M, Sudhop T, von Bergmann K. Metabolism and drug interactions of 3-hydroxy-3-methylgluaryl coenzyme A-reductase inhibitors (statins). Eur J Clin Pharmacol 2001; 57: 357–64
Jacobsen W, Kuhn B, Soldner A, et al. Lactonization is the critical first step in the disposition of the 3-hydroxy-3-methyl-glutaryl-coA reductase inhibitor atorvastatin. Drug Metab Dispos 2000; 28: 1369–78
Rivistö KT, Lamberg TS, Neuvonen PJ. Interactions of buspirone with itraconazole and rifampicin: effects on the pharmacokinetics of the active 1-(2-pyrimidinyl)-piperazine metabolite of buspirone. Pharmacol Toxicol 1999; 84: 94–7
Lamberg TS, Rivistö KT, Laitila J, et al. The effect of fluvoxamine on the pharmacokinetics and pharmacodynamics of buspirone. Eur J Clin Pharmacol 1998; 54: 761–6
Lilja JJ, Kivistö KT, Backman JT, et al. Grapefruit juice substantially increases plasma concentrations of buspirone. Clin Pharmacol Ther 1998; 64: 655–60
Rodrigues AD, Roberts EM, Mulford DJ, et al. Oxidative metabolism of clarithromycin in the presence of human liver microsomes: major role for the cytochrome P4503A (CYP3A) subfamily. Drug Metab Dispos 1997; 25: 623–30
Pichard L, Fabre I, Fabre G, et al. Cyclosporine A drug interactions: screening for inducers and inhibitors of cytochrome P-450 (cyclosporin A oxidase) in primary cultures of human hepatocytes and in liver microsomes. Drug Metab Dispos 1990; 18: 595–606
Pichard L, Fabre I, Daujat M, et al. Effect of corticosteroide on the expression of cytochrome P450 and on cyclosporine A oxidase activity in primary cultures of human hepatocytes. Mol Pharmacol 1992; 41: 1047–55
Lee KH, Shin JG, Chong WS, et al. Time course of the changes in prednisolone pharmacokinetics after administration or discontinuation of rifampin. Eur J Clin Pharmacol 1993; 45: 287–9
Wienkers LC, Steenwyk RC, Sanders PE, et al. Biotransformation of tirilazad in humans. I: cytochrome P450 3A-mediated hydroxylation of tirilazad mesylate in human liver microsomes. J Pharmacol Exp Ther 1996; 277: 982–90
Pichard L, Gillet G, Bonfils C, et al. Oxidative metabolism of Zolpidem by human liver cytochrome P450s. Drug Metab Dispos 1995; 23: 1253–62
von Moltke LL, Greenblatt DJ, Granda BW, et al. Zolpidem metabolism in vitro: responsible cytochromes, chemical inhibitors, and in vivo correlations. Br J Clin Pharmacol 1999; 48: 89–97
Mugford CA, Kedderis GL. Sex-dependent metabolism of xenobiotics. Drug Metab Rev 1998; 30: 441–98
Kashuba ADM, Nafziger AN. Physiological changes during the menstrual cycle and their effects on the pharmacokinetics and pharmacodynamics of drugs. Clin Pharmacokinet 1998; 34: 203–18
Meibohm B, Beierle I, Derendorf H. How important are gender differences in pharmacokinetics. Clin Pharmacokinet 2002; 41: 329–42
Yamazaki G, Shimada T. Progesterone and testosterone hydroxylation by cytochromes P450 2C19, 2C9, and 3A4 in human liver microsomes. Arch Biochem Biophys 1997; 346: 161–9
Lee AJ, Kosh JW, Conney AH, et al. Characterization of the NADPH-dependent metabolism of 17β-estradiol to multiple metabolites by human liver microsomes and selectively expressed human cytochrome P450 3A4 and 3A5. J Pharmacol Exp Ther 2001; 298: 420–32
Waxman DJ, Attisano C, Guengerich FP, et al. Human liver microsomal steroid metabolism: identification of the major microsomal steroid hormone 6β-hydroxylase cytochrome P-450 enzyme. Arch Biochem Biophys 1988; 263: 424–36
Maenpaa J, Hall SD, Ring BJ, et al. Human cytochrome P450 3A(CYP3A) mediated midazolam metabolism: the effect of assay conditions and regioselective stimulation by α-naphthoflavone, terfenadine and testosterone. Pharmacogenetics 1998; 8: 137–55
Nakamura H, Kakasa H, Ishii I, et al. Effects of endogenous steroids on CYP3A4-mediated drug metabolism by human liver microsomes. Drug Metab Dispos 2002; 30: 534–40
Shou M, Grogan J, Mancewicz JA, et al. Activation of CYP3A4: evidence for the simultaneous binding of two substrates in a cytochrome P450 active site. Biochemistry 1994; 33: 6450–5
Schrag ML, Wienkers LC. Covalent alteration of the CYP3A4 active site: evidence for multiple substrate binding domains. Arch Biochem Biophys 2001; 391: 49–55
Vermeulen A. Androgen secretion after age 50 in both sexes. Horm Res 1983; 18: 37–42
Nahoul K, Roger M. Age-related decline of plasma bioavailable testosterone in adult men. J Steroid Biochem 1990; 35: 293–9
Gray A, Feldman HA, McKinlay JB, et al. Age, disease, and changing sex hormone levels in middle-aged men: results of the Massachusetts male aging study. J Clin Endocrinol Metab 1991; 73: 1016–25
Simon D, Preziosi P, Barrett-Connor E, et al. The influence of aging on plasma sex hormones in men: the Telecom study. Am J Epidemiol 1992; 135: 783–91
Morley JE, Kaiser F, Raum WJ, et al. Potentially predictive and manipulable blood serum correlates of aging in the healthy human male: progressive decreases in bioavailable testosterone, dehydroepiandrosterone sulfate, and the ratio of insulinlike growth factor 1 to growth hormone. Proc Natl Acad Sci U S A 1997; 94: 7537–42
Sotaniemi EA, Arranto AJ, Pelkonen O, et al. Age and cytochrome P450-linked drug metabolism in humans: an analysis of 226 subjects with equal histopathologic conditions. Clin Pharmacol Ther 1997; 61: 331–9
Kirkwood C, Moore A, Hayes P, et al. Influence of menstrual cycle and gender on alprazolam pharmacokinetics. Clin Pharmacol Ther 1991; 50: 404–9
Kristjánsson F, Thorsteinsson SB. Disposition of alprazolam in human volunteers: differences between genders. Acta Pharm Nord 1991; 3: 249–50
Mendelson JH, Mello NK, Sholar MB, et al. Cocaine pharmacokinetics in men and in women during the follicular and luteal phases of the menstrual cycle. Neuropsychopharmacology 1999; 21: 294–303
Wing LMH, Miners JO, Birkett DJ, et al. Lidocaine disposition: sex differences and effects of Cimetidine. Clin Pharmacol Ther 1984; 35: 695–701
Zhou LX, Finley DK, Hassell AE, et al. Pharmacokinetic interaction between isradipine and lovastatin in normal, female and male volunteers. J Pharmacol Exp Ther 1995; 273: 121–7
Kashuba AD, Bertino Jr JS, Rocci Jr ML, et al. Quantification of 3-month intraindividual variability and the influence of sex and menstrual cycle phase on CYP3A activity as measured by phenotyping with intravenous midazolam. Clin Pharmacol Ther 1998; 64: 269–77
Fleishaker JC, Hulst-Pearson LK, Peters GR. Effect of gender and menopausal status on the pharmacokinetics of tirilazad mesylate in healthy subjects. Am J Ther 1995; 2: 553–60
Greenblatt DJ, Harmatz JS, Gouthro TA, et al. Distinguishing a benzodiazepine agonist (triazolam) from a non-agonist anxiolytic (buspirone) by electroencephalography: kinetic-dynamic studies. Clin Pharmacol Ther 1994; 56: 100–11
Greenblatt DJ, Harmatz JS, von Moltke LL, et al. Comparative kinetics and response to the benzodiazepine agonists triazolam and Zolpidem: evaluation of sex dependent differences. J Pharmacol Exp Ther 2000; 293: 435–43
Krecic-Shepard ME, Barnas CR, Slimko J, et al. Faster clearance of sustained release verapamil in men versus women: continuing observations on sex-specific differences after oral administration of verapamil. Clin Pharmacol Ther 2000; 68: 286–92
Kang D, Verotta D, Krecic-Shepard ME, et al. Population analyses of sustained-release verapamil in patients: effects of sex, race, and smoking. Clin Pharmacol Ther 2003; 73: 31–40
LeDuc BW, Sinclair PR, Shuster L, et al. Norcocaine and N-hydroxynorcocaine formation in human liver microsomes: role of cytochrome P-450 3A4. Pharmacology 1993; 46: 294–300
Pellinen P, Honkakoski P, Stenback F, et al. Cocaine N-demethylation and the metabolism-related hepatotoxicity can be prevented by cytochrome P450 3A inhibitors. Eur J Pharmacol 1994; 270: 35–43
Ladona MG, Gonzalez ML, Rane A, et al. Cocaine metabolism in human fetal and adult liver microsomes is related to cytochrome P450 3A expression. Life Sci 2000; 68: 431–43
Pellinen P, Kulmala L, Konttila J, et al. Kinetic characteristics of norcocaine N-hydroxylation in mouse and human liver microsomes: involvement of CYP enzymes. Arch Toxicol 2000; 74: 511–20
Wang J-S, Backman JT, Taavitsainen P, et al. Involvement of CYP1A2 and CYP3A4 in lidocaine N-demethylation and 3-hydroxylation in humans. Drug Metab Dispos 2000; 28: 959–65
Cummins CL, Wu CY, Benet LZ. Sex-related differences in the clearance of cytochrome P450 3A4 substrates may be caused by P-glycoprotein. Clin Pharmacol Ther 2002; 72: 474–89
Gandhi M, Aweeka F, Greenblatt RM, et al. Sex differences in pharmacokinetics and pharmacodynamics. Annu Rev Pharmacol Toxicol 2004; 44: 499–523
Schwartz JB. The influence of sex on pharmacokinetics. Clin Pharmacokinet 2003; 42: 107–21
McLean AJ, Le Couteur DG. Aging biology and geriatric clinical pharmacology. Pharmacol Rev 2004; 56: 163–84
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 2004; 57: 6–14
Hendrix CW, Jackson KA, Whitmore E, et al. The effect of isotretinoin on the pharmacokinetics and pharmacodynamics of ethinyl estradiol and norethindrone. Clin Pharmacol Ther 2004; 75: 464–75
Wolbold R, Klein K, Burk O, et al. Sex is a major determinant of CYP3A4 expression in human liver. Hepatology 2003; 38: 978–88
Wilson ZE, Rostami-Hodjegan A, Burn JL, et al. Inter-individual variability in levels of human microsomal protein and hepatocellularity per gram of liver. Br J Clin Pharmacol 2003; 56: 433–40
El-Eraky H, Thomas SHL. Effects of sex on the pharmacokinetic and pharmacodynamic properties of quinidine. Br J Clin Pharmacol 2003; 56: 198–204
Gorski JC, Vannaprasaht S, Hamman MA, et al. The effect of age, sex, and rifampin administration on intestinal and hepatic cytochrome P450 3A activity. Clin Pharmacol Ther 2003; 74: 275–87
Greenblatt DJ, Harmatz JS, von Moltke LL, et al. Age and gender effects on the pharmacokinetics and pharmacodynamics of triazolam, a cytochrome P450 3A substrate. Clin Pharmacol Ther 2004; 76: 467–79
Patki KC, von Moltke LL, Harmatz JS, et al. Effect of age on in vitro triazolam biotransformation in male human liver microsomes. J Pharmacol Exp Ther 2004; 308: 874–9
Acknowledgements
The preparation of this review was supported by grants AG-17880, MH-58435, MH-01237, DA-05258, DA-13209, DK/AI-58496, AT-01381 and RR-00054 from the Department of Health and Human Services, Washington, DC, USA. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cotreau, M.M., von Moltke, L.L. & Greenblatt, D.J. The Influence of Age and Sex on the Clearance of Cytochrome P450 3A Substrates. Clin Pharmacokinet 44, 33–60 (2005). https://doi.org/10.2165/00003088-200544010-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200544010-00002