Abstract
Purpose
Diabetes-related distress (DRD) has negative emotional effects on the patients’ quality of life. This is while the condition often goes undiagnosed despite it being common among diabetic patients. This study investigated the prevalence of DRD and its association with diabetes complications among a group of Iranian type 2 diabetic patients (T2DM).
Methods
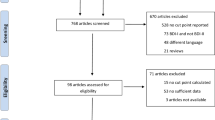
This descriptive-analytical cross-sectional study was conducted on 186 T2DM patients referred to a diabetes clinic in a teaching hospital from the beginning of May 2019 to the end of April 2020. Two questionnaires on disease-related information and diabetes distress screening scale (DDS) were filled out for each patient. The latter was divided into four domains, emotional burden (EB), diabetes-related interpersonal distress (ID), physician-related distress (PD), and regimen-related distress (RD). In addition to the frequency of DRD and its association with age, sex, body mass index (BMI), hypertension, hemoglobin A1C, duration of disease, and type of medication regimen (oral, insulin, or mix) along with the history of cardiovascular disease (CVDs), retinopathy, nephropathy, and diabetic foot were assessed.
Results
DRD was reported in 47% of the patients. Being female, old age, hypertension, high hemoglobin A1C levels, nephropathy, and retinopathy were significantly associated with DRD (P-value = < 0.001, 0.013, 0.014, 0.007, 0.001, and 0.004, respectively). The history of the diabetic foot had a significant relationship with PD and ID (P-value = 0.007 and < 0.001, respectively). Multivariate regression showed gender and the existence of complications to have a direct effect on the development of DRD.
Conclusion
DRD prevalence is relatively high and requires screening to identify and treat high-risk patients. Further studies are needed to study diabetes, its complications and their relation with DRD to help reduce such conditions and improve the patient’s quality of life.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM), characterized by increased blood glucose levels, is the seventh leading cause of death worldwide [1, 2]. DM is one of the most common chronic diseases with a rapidly growing incidence among low to middle-income countries mainly due to urbanization and lifestyle changes. DM is a challenging disease as it affects several organs simultaneously, leading to serious complications. These complications range from microvascular such as neuropathy, nephropathy, and retinopathy to macrovascular ones including cardiovascular, cerebrovascular (stroke), and peripheral vascular diseases [3].
Type 2 diabetes (T2DM), the most common type of DM, is caused by a relative lack of insulin due to defects in the pancreatic beta cells or insulin resistance in the target organs [4]. The estimated prevalence of T2DM is about 6% worldwide and between 1.3% and 14.5% in Iran [5]. T2DM, therefore, is associated with negative emotions such as anxiety, depression, and distress. Diabetes-related emotional distress is getting more attention these days. It is mainly caused due to special lifestyle restrictions coupled with the feeling of being sick and the complexity of the instructions given by the physicians to the patient with no medical background [6, 7]. Diabetes-related distress (DRD) has been correlated to poor clinical consequences including non-adherence to medication and poor glycemic control [8, 9]. Despite all this, DRD is often undiagnosed or left untreated, mainly because of the low awareness from both the physician and the patient [10].
Several studies have assessed the prevalence of DRD and depression among T2DM patients in Western countries; however, there are limited studies on this concept in Iran [11, 12]. Considering the heavy burden and limited knowledge of DRD in the country, this study was designed to assess its prevalence and relationship with the patient's demographic, micro- or macrovascular complications, and diabetes control in a group of Iranians.
Material and methods
This descriptive-analytical cross-sectional study was conducted on consecutive adult T2DM patients visiting Imam Khomeini diabetes clinic between May 2019 and April 2020. The routine follow-up in the clinic consisted of checking for the diabetes-related complications and glycemic and blood pressure control among other variables every three to six months.
The study was approved by the ethics committee of Tehran University of Medical Sciences (TUMS) (ethics code 1397.363.IR.TUMS.IKHC.REC). All the patients signed written informed consent. The patients were selected from among those fulfilling the inclusion criteria, having a complete workup, and signing the consent form.
They completed two questionnaires. The first one consisted of three main sections on personal and anthropometric description, diabetes-related information (duration of the disease, history of cardiovascular diseases (CVD), diabetic foot (history of amputation or chronic foot injuries), use of antihypertensive drugs, hospitalization in recent months, recent psychiatric illnesses confirmed by a psychiatrist, and consumption of psychiatric medications), diabetes-related paraclinical data based on medical records (blood pressure, hemoglobin A1c, medication (oral, insulin or both), retinopathy (proliferative and non-proliferative changes), and nephropathy (diagnosed based on persistent albuminuria of more than 300 mg/d or > 200 μg/min confirmed in at least two occasions 3–6 months apart or low estimated glomerular filtration rate (eGFR)). Those with a history of psychiatric disorders, use of psychiatric drugs, or hospitalization in recent months were excluded.
The second questionnaire was the Persian version of the diabetes distress screening scale (DDS) [13]. The validity and reliability of the translated version were confirmed in another study [5]. It consisted of 17 questions divided into four domains, emotional burden (EB) (questions 1, 3, 8, 11, and 14) assessing patients’ anger or fear due to living as a diabetic; interpersonal distress (ID) (questions 7, 13, and 17) indicating their suffering due to not being understood by friends or family; physician-related distress (PD) (questions 2, 4, 9, and 15) suggesting their disappointment in not being consulted by a physician regarding the treatment options; and regimen-related distress (RD) (questions 5, 6, 10, 12, And 16) linked with their concern about not feeling motivated for diabetes self-management.
The patients gave a score between 1 and 6 to each question based on their feeling in the past month. A score of 3 or higher for each question indicated DRD. The total score was calculated by averaging the sum of all points. A mean score of less than 2.0 was considered little or no distress, 2.0 to less than 3.0 showed moderate distress, and 3.0 or more pointed out high distress.
Sample size
The sample size was calculated based on the data gathered in previous studies (expected prevalence of 35% [5]), and a power of 80%. Ten percent was added to compensate for possible data loss, resulting in a sample size of 186 patients.
Statistical analysis
The information was analyzed using SPSS software version 25. Mean and standard deviation were used to report the quantitative variables, whereas frequency and percentages were for the qualitative ones. T-test and Mann–Whitney U test were used for quantitative data with normal and non-normal distribution, respectively. Chi-square and Fisher exact tests were used for qualitative ones. The relationship between DRD and quantitative variables with normal distribution was assessed using Pearson correlation, whereas Spearman correlation was used for the others. Phi and V Cramer tests were used to evaluate the intensity of qualitative relationships. Uni and multivariate logistic regression were applied to determine the variables with a direct effect on DRD. In this regard, only covariates with a significant effect on the outcome, DRD, were entered in the multivariate logistic regression. The significance level was considered as P-value < 0.05.
Results
From among the 186 T2DM patients, 82 were men and 104 were women. Their mean age and BMI values were 61 years and 28.44 kg/m2, correspondingly. DRD and its subscales were reported in 47% of the participants, with EB found in 81%, RD in 77%, ID in 14%, and PD in 2% of them.
There was a significant but not strong relationship between age (p-value: 0.013) and DRD and only EB (P-value = 0.020). Similar relationship was found between patients' gender and their hypertension status and DRD (gender: p-value < 0.001, Phi Cramer test = 0.31; hypertension: p-value = 0.014, Phi Cramer = 0.19) (Table 1). As for the subscales, however, a significant relationship was only reported with EB (gender: p-value = 0.015; hypertension: p-value = 0.025). While BMI did not have any significant relationship with DRD, it was reported to be correlated with EB and PD (p-value = 0.003 and 0.019, respectively) (Table 2).
Patients with DRD had slightly but significantly higher hemoglobin A1C values compared with those with no distress (8.03 vs 7.73, p-value = 0.007); similar significant difference was noted in those with all the subscales except for RD (ID p-value = 0.018, PD p-value = 0.006, and EB p-value = 0.036) (Table 2). There was, however, no significant relationship in terms of disease duration and treatment options and experiencing distress (p-value = 0.298 and 0.28, retrospectively) or its subscales (ID p-value = 0.288 and 0.87, PD p-value = 0.330 and 0.25, EB p-value = 0.099 and 0.52, RD p-value = 0.799 and 0.99, retrospectively).
About 61% of the patients with DRD suffered from at least one complication. There was a significant and high correlation between having at least one complication and DRD, EB, ID, and RD (p-value = < 0.001, < 0.001, 0.009, and < 0.001, with Phi Cramer = 0.30, 0.37, 0.27, and 0.27 respectively).
Nephropathy (39%) and retinopathy (37%) were the most common complications, whereas diabetic foot was reported in only four percent of the participants. Except for three patients with nephropathy alone, the rest suffered from both complications. DRD was reported in about 60% of the patients with these complications. There was a significant relationship between nephropathy and DRD, EB, and RD (p-value = 0.001, < 0.001, and 0.005, respectively). The correlation coefficient of these relationships, however, indicated a high-intensity relationship between them (Phi Cramer = 0.25, 0.29, and 0.22, respectively). Similarly, a significant and strong relationship was reported between retinopathy and DRD, EB, and RD (p-value = 0.004, < 0.001, and 0.003, with the Phi Cramer = 0.22, 0.28, and 0.23, respectively) (Table 1).
CVD with a prevalence of 56% among DRD patients ranked next on the complication list. This is while no significant relationship was found between having a history of CVD and DRD (p-value = 0.171). As for the subscales, however, a significant relationship was found between the CVD history and EB and RD, (P-value = 0.011 and 0.015, respectively). In line with the high prevalence, the intensity of the correlation coefficients for these relationships was relatively high (Phi Cramer = 0.20 and 0.19, respectively).
Six out of seven patients with a positive history of diabetic foot suffered from DRD. A significant relationship was found between experiencing diabetic foot and DRD subscales, ID and PD, rather than DRD itself (p-value = < 0.001, 0.007, and 0.052, respectively).
Table 3 illustrates the estimated effect of covariates with a significant effect on DRD using a multivariate logistic regression model. Gender and complications were the only determinants that were significantly associated with DRD (p-value = 0 and 0.001, respectively). The estimated odds of developing DRD in a female diabetic with at least a complication were 0.165 and 0.253 times the estimated odds of a male diabetic with no complications, respectively.
Discussion
The present study revealed being a female and having at least one of the diabetes-related complications are at a greater risk of experiencing DRD, highlighting the need for special attention for the condition in diabetic patients. Living with DM requires self-care including taking medication, following an appropriate diet, physical activity, and performing regular blood sugar check-ups. This is mainly because keeping the hemoglobin A1C levels within the target range can reduce the risk of developing complications and thus prevent or delay the long-term effects of the disease. All these are responsible for the development of DRD among diabetic patients [14]. The prevalence of DRD ranges between 21 and 49% in different parts of the world. Baradaran et al. [5] estimated the number to be about 35% in Iran, which is lower than the results of the current study (45%). This may be explained by the fact that the current study was conducted in a tertiary referral center with a high number of patients in advanced stages of DM.
In line with previous studies, EB and RD had the highest prevalence among our patients [5, 15]. Al-Jaeed et al. showed EB (54%) and PD (25%) as the most common subscales among patients with moderate to severe DRD in Saudi Arabia [15]. The lower prevalence of PD in our study could be due to the patient's higher satisfaction with their doctor as well as the better quality of the doctor-patient relationship. This could also be the result of a bias because of possible fear of negative effects on their treatment process in case they declare low satisfaction. The higher RD prevalence in our study, on the other hand, points out the need for our physicians to discuss diet and treatment options with the patients to help reduce their concerns and improve their adherence by making treatment more realistic and personalized.
DRD was twice more prevalent among women in this study, and a significant relationship was found between being a woman and EB. In accordance with our results, Chew et al. concluded the female gender is a risk factor for DRD, especially EB (35). They also showed a significant relationship between depression and DRD. The prevalence of major depression in women is twice the rate in men could point out underlying and possibly undiagnosed major depression as an important reason behind higher rates of DRD among women [16].
Apart from being female, having at least one complication was the only other determinant of DRD in the present study. This suggests that other covariates may affect the risk of developing DRD indirectly. The following paragraphs explain these covariates and how they may increase a patient’s risk of experiencing DRD.
We found old age to be significantly associated with DRD and EB; it should be kept in mind that the higher prevalence of accompanying complications at older ages could explain this finding.
Previous studies have linked DRD with poor self-management among diabetic patients [17]. Fisher et al. reported the condition to be linked with female gender, previous history of major depressive disorders, diabetes complications, non-adherence to appropriate diet, and low physical activity [12]. In another study, low engagement in physical activity and non-adherence to appropriate diet or medication, as the strong contributors to poor glycemic control, were linked with DRD [18, 19]. Pena-Purcel also showed a higher rate of poor glycemic control among patients with diabetes and co-morbid DRD compared with those with DM alone [20]. In line with these studies, we found significantly higher Hemoglobin A1C levels in the individuals with higher distress compared with those with mild to moderate distress, suggesting a significant relationship between higher hemoglobin A1C values and DRD and its subscales [15]. Similar to age, there is an interaction between poor glycemic control and complications. In another word, the higher DRD rates among individuals with poor glycemic control regardless of the treatment type could be due to the presence of complications. This theorem suggests that better diabetes control and prevention of its complications could reduce DRD risk significantly.
Contrary to Kasteleyn et al., we failed to find any significant relationship between the duration of disease and DRD [21]. This is while suffering from the disease for a longer duration is also associated with a higher risk of developing micro- and macro-vascular complications, which as mentioned above increases the risk of experiencing DRD (34). The possible explanation for such a finding could be the fact that most of our patients were in the advanced stages of the disease with multiple complications, making it impossible to assess the effect of the duration of the disease without taking into account underlying complications. The high prevalence of hypertension among our population and its significant association with DRD and EB was consistent with previous studies [22]. This also explains the high prevalence of nephropathy and retinopathy, and their significant association with DRD and its subscales in this population. Having a history of diabetic foot was similarly linked with DRD and PD. Again, hypertension could have increased the risk of experiencing DRD by resulting in higher rates of such co-morbidities.
A positive history of CVDs was only significantly correlated with EB and RD, and not DRD in general. A positive history of CVD in this study was only considered if the patient had undergone angioplasty or open-heart surgery prior to the study; we, thus, might have underestimated the CVD rate, especially in the early stages of the disease. This suggests improving awareness about the disease and adverse wound complications could result in better engagement in foot care and thus improved ID and PD.
Limitations
Due to the cross-sectional nature of our study, a causal relationship between diabetes complications and DRD and its subscales cannot be inferred in this study, and further longitudinal studies are needed. Moreover, we might have overestimated the prevalence of hypertension among our subjects as the diagnosis was made based on having high blood pressure (greater or equal to 140/90 mmHg) at the time of visit or taking the corresponding medication. The rate of CVDs, on the other hand, as mentioned earlier might have been underestimated. It is also worth mentioning that the family history of diabetes-related complications or death along with the socio-economic and educational status of the patients may also affect DRD risk but were not studied in the present research. It should also be highlighted that the present study was conducted in a tertiary referral center; its results, therefore, cannot be representative of the whole society. Further multicentric studies are needed to help generalize and confirm our results. However, this study is one of the pioneer studies on DRD in the Iranian population and should be considered one of the strengths of the present research. Moreover, the longer sampling process and lower number of patients who visited the clinics during the study period (compared with the year before) were due to the COVID-19 pandemic.
Conclusion
The high prevalence of DRD in our population calls for more attention to the concept from both the policymakers, physicians, and patient point of view. The results of the present study can therefore help develop a national program for screening and diagnosis of DRD in the Iranian healthcare system. These interventions should focus on identifying high-risk individuals, preferably during regular diabetes visits, similar to what is currently done for other complications (such as nephropathy and retinopathy). Psychiatrists and psychologists working in the field of diabetes should also develop specific interventions (pharmacological or non-pharmacological) for the management of this condition.
References
Roden M. Diabetes mellitus – Definition, Klassifikation und Diagnose. Wien Klin Wochenschr [Internet]. 2016;128:37–40. Available from: https://doi.org/10.1007/s00508-015-0931-3. Accessed 20 Mar 2022.
Huynh G, Tran TT, Do THT, Truong TTD, Ong PT, Nguyen TNH, et al. Diabetes-Related Distress Among People with Type 2 Diabetes in Ho Chi Minh City, Vietnam: Prevalence and Associated Factors. Diabetes, Metab Syndr Obes Targets Ther [Internet]. 2021; Volume 14:683–90. Available from: https://www.dovepress.com/diabetes-related-distress-among-people-with-type-2-diabetes-in-ho-chi--peer-reviewed-article-DMSO. Accessed 20 Mar 2022.
Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of Diabetes and Diabetes-Related Complications. Phys Ther. 2008;88:1254–64.
Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet [Internet]. 2017;389:2239–51. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673617300582. Accessed 20 Mar 2022.
Baradaran HR, Mirghorbani S-M, Javanbakht A, Yadollahi Z, Khamseh ME. Diabetes distress and its association with depression in patients with type 2 diabetes in Iran. Int J Prev Med [Internet]. 2013;4:580–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23930169. Accessed 20 Mar 2022.
Chew B-H, Mohd-Sidik S, Shariff-Ghazali S. Negative effects of diabetes–related distress on health-related quality of life: an evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in Malaysia. Health Qual Life Outcomes [Internet]. 2015;13:187. Available from: https://doi.org/10.1186/s12955-015-0384-4.
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing Psychosocial Distress in Diabetes. Diabetes Care [Internet]. 2005;28:626–31. Available from: https://diabetesjournals.org/care/article/28/3/626/27791/Assessing-Psychosocial-Distress-in. Accessed 20 Mar 2022.
Miller ST, Elasy TA. Psychometric evaluation of the Problem Areas in Diabetes (PAID) survey in Southern, rural African American women with Type 2 diabetes. BMC Public Health [Internet]. 2008;8:70. Available from: https://doi.org/10.1186/1471-2458-8-70.
Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The relationship between food insecurity and depression, diabetes distress and medication adherence among low-income patients with poorly-controlled diabetes. J Gen Intern Med [Internet]. 2015;30:1476–80. Available from: https://doi.org/10.1007/s11606-015-3351-1.
Pouwer F. Should we screen for emotional distress in type 2 diabetes mellitus? Nat Rev Endocrinol. 2009;5:665–71.
Geleta BA, Dingata ST, Emanu MD, Eba LB, Abera KB, Tsegaye D. Prevalence of Diabetes Related Distress and Associated Factors Among Type 2 Diabetes Patients Attending Hospitals, Southwest Ethiopia, 2020: A Cross-Sectional Study. Patient Relat Outcome Meas [Internet]. 2021;12:13–22. Available from: https://www.dovepress.com/prevalence-of-diabetes-related-distress-and-associated-factors-among-t-peer-reviewed-article-PROM. Accessed 20 Mar 2022.
Fisher L, Mullan JT, Skaff MM, Glasgow RE, Arean P, Hessler D. Predicting diabetes distress in patients with Type 2 diabetes: a longitudinal study. Diabet Med. 2009;26:622–7.
Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Ann Fam Med [Internet]. 2008;6:246–52. Available from: https://doi.org/10.1370/afm.842. Accessed 20 Mar 2022.
Dennick K, Sturt J, Speight J. What is diabetes distress and how can we measure it? A narrative review and conceptual model. J Diabetes Complications. 2017;31:898–911.
Aljuaid MO, Almutairi AM, Assiri MA, Almalki DM, Alswat K. Diabetes-related distress assessment among type 2 diabetes patients. J Diabetes Res [Internet]. 2018;2018:1–10. Available from: https://www.hindawi.com/journals/jdr/2018/7328128/. Accessed 20 Mar 2022.
Malhi GS, Mann JJ. Depression. Lancet [Internet]. 2018;392:2299–312. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673618319482. Accessed 20 Mar 2022.
Fritschi C, Quinn L. Fatigue in patients with diabetes: A review. J Psychosom Res [Internet]. 2010;69:33–41. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0022399910000620. Accessed 20 Mar 2022.
Kretchy IA, Koduah A, Ohene-Agyei T, Boima V, Appiah B. The association between diabetes-related distress and medication adherence in adult patients with Type 2 diabetes mellitus: a cross-sectional study. J Diabetes Res [Internet]. 2020;2020:1–10. Available from: https://www.hindawi.com/journals/jdr/2020/4760624/. Accessed 20 Mar 2022.
Egede LE, Dismuke CE. Serious psychological distress and diabetes: a review of the literature. Curr Psychiatry Rep [Internet]. 2012;14:15–22. Available from: https://doi.org/10.1007/s11920-011-0240-0.
Peña-Purcell N, Han G, Lee Smith M, Peterson R, Ory MG. Impact of diabetes self-management education on psychological distress and health outcomes among African Americans and Hispanics/Latinos with diabetes. Diabetes Spectr [Internet]. 2019;32:368–77. Available from: https://diabetesjournals.org/spectrum/article/32/4/368/32413/Impact-of-Diabetes-Self-Management-Education-on. Accessed 20 Mar 2022.
Kasteleyn MJ, de Vries L, van Puffelen AL, Schellevis FG, Rijken M, Vos RC, et al. Diabetes-related distress over the course of illness: results from the Diacourse study. Diabet Med [Internet]. 2015;32:1617–24. Available from: https://doi.org/10.1111/dme.12743. Accessed 20 Mar 2022.
Centers for Disease Control and Prevention. National Diabetes Statistics Report https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 20 Mar 2022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khashayar, P., Shirzad, N., Zarbini, A. et al. Diabetes-related distress and its association with the complications of diabetes in Iran. J Diabetes Metab Disord 21, 1569–1575 (2022). https://doi.org/10.1007/s40200-022-01103-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01103-2