Abstract
Objective
Polypharmacy increases the risk of adverse drug events and drug–drug interactions, and contributes to falls, hospital admissions, morbidity and mortality. Veterans with post-traumatic stress disorder often have psychological and physical comorbidities, increasing the likelihood of general and psychotropic polypharmacy. This study investigates the prevalence of general and psychotropic polypharmacy in inpatient veterans with post-traumatic stress disorder, and illustrates potential risks associated with polypharmacy in this population.
Methods
Medical records of 219 veterans admitted to a mental health facility for post-traumatic stress disorder management were retrospectively reviewed. Medication lists on admission were extracted and coded according to Anatomical Therapeutic Chemical Classification classes. The prevalence of general (five or more total medications), psychotropic (two or more N-code medications), and sedative (two or more medications with sedating effects) polypharmacy and Drug Burden Index were calculated. Class combinations were reported, and associations between demographic characteristics and polypharmacy were determined.
Results
Mean age was 62.5 (± 14.6) years. In addition to post-traumatic stress disorder, 90.9% had a diagnosis of at least one other psychiatric condition, and 96.8% had a diagnosis of at least one non-psychiatric medical condition. The prevalence of general polypharmacy was 76.7%, psychotropic polypharmacy was 79.9% and sedative polypharmacy was 75.3%. Drug Burden Index scores ranged from 0 to 8.2, with 66.2% of participants scoring ≥ 1.
Conclusions
This cohort of inpatient veterans with post-traumatic stress disorder had a high prevalence of general, psychotropic and sedative polypharmacy, and were at high risk for drug-related adverse events. This highlights the importance of increasing awareness of polypharmacy and potentially inappropriate drug combinations, and the need for improved medication review by prescribers.
Similar content being viewed by others
There is a high prevalence of general, psychotropic and sedative polypharmacy in veterans admitted for the management of post-traumatic stress disorder, placing them at high risk for drug-related adverse events. |
This highlights the urgent need to improve medication review and prescribing practice for veterans with psychological and physical comorbidities. |
1 Introduction
Polypharmacy is the concurrent use of multiple medications in a single patient. It is associated with an increased risk of adverse drug events, drug–drug interactions and drug–disease interactions. This can contribute to falls, cognitive impairment, hospital admissions, and overall morbidity and mortality, especially in older patients who may have reduced drug clearance [1]. Polypharmacy and inappropriate prescribing also impose a significant economic burden, with polypharmacy-related adverse drug events leading to increased drug expenses, longer hospital stays or hospital readmissions, and higher overall total medical costs [2]. Two to three percent of Australian hospital admissions are medication related, representing an estimated 250,000 medication-related hospital admissions per year, with associated costs of AUD$1.375 billion. Notably, it is estimated that approximately 50% of medication-related hospital admissions and adverse drug reactions associated with hospitalisation are potentially preventable [3]. In 2017–2018, harmful exposure to pharmaceutical drugs made up 84% of accidental poisoning hospitalisation cases [4] and in the USA, one study found that the accidental poisoning mortality rate due to medications in veterans was significantly higher than the general US population. The more concerning statistic from this study identified that a veterans’ risk of accidental poisoning death as a consequence of polypharmacy was greater than that of death by suicide [5]. Opioids (18.5%) and methadone (13.8%) were the medications most frequently mentioned in cause of death records (T-code reporting); however, antidepressants and benzodiazepines comprised 8.1% and 7.5%, respectively, of the medications reported to be involved in fatal accidental poisoning.
Psychotropic polypharmacy refers to combination therapy with two or more psychotropic medicines [6], which are defined as any drug capable of affecting the mind, emotions and behaviour [7]. There is a paucity of strong evidence supporting the safety and effectiveness of psychotropic drug combinations. In the general Australian population, the prevalence of psychotropic polypharmacy is approximately 15–22%, with the most common drug combinations including benzodiazepines [6, 8, 9]. Problematic psychotropic prescribing (e.g. benzodiazepine use in the elderly, antipsychotic use in dementia and prescribing two or more antipsychotics concurrently) was associated with an estimated cost of over AUD$21 million to the government in 2016 [10].
Post-traumatic stress disorder (PTSD) is a complex mental health condition that can develop after exposure to a traumatic event [11]. Australian guidelines recommend evidence-based psychological treatments as first-line therapy for PTSD, and that pharmacotherapy may be used as an adjunct to psychosocial interventions, or as an alternative when psychosocial interventions are unavailable, not effective, or not preferred. There is evidence for the selective serotonin reuptake inhibitors fluoxetine, paroxetine and sertraline in the pharmacological management of PTSD but comparative trials are lacking. There is also some evidence for venlafaxine, a serotonin noradrenaline reuptake inhibitor (SNRI), but patients with PTSD may be particularly sensitive to its adverse effects. Although there are no data for other selective serotonin reuptake inhibitors and SNRIs, they are likely to have similar effectiveness [12].
In the treatment of PTSD in Australian Defence Force (ADF) veterans, the selection of medications is often challenging, owing not only to limited clinical pharmacotherapy guidelines and a lack of trialled and approved medications, but also a high prevalence of comorbid illnesses [13], sleep disturbance [14] and chronic pain [15, 16]. This increases the likelihood of general and psychotropic polypharmacy. In the USA, it was reported that prescribing prevalence for both benzodiazepines and opioids for veterans with PTSD is in excess of 30% individually, and nearly 16% in combination [17]. This raises concern about adherence to guidelines for evidence-based treatment. In general, pharmacological guidelines for the management of PTSD are relatively consistent [18,19,20,21]; however, there are no guidelines for concurrent pharmacological management of other physical and medical comorbidities, and little is currently known about how psychotropic medications are combined with other medications used to treat associated conditions.
Additional problems can arise because of limited co-ordination and communication between multiple providers [22] who may be separately addressing each concomitant condition in a patient with PTSD and multiple comorbidities. It has been reported that mental health specialists are predominant benzodiazepine prescribers in veterans with PTSD, whereas primary care and non-mental health specialists are the more prominent prescribers of opioids [23]. This poses a high likelihood of high-risk medication combinations.
With approximately 6% of the Australian population and 25% of recently transitioned ADF members estimated to experience PTSD in their lifetime [24], PTSD-related psychotropic polypharmacy is of significant concern. In a recent study, it was found that the prevalence of psychotropic polypharmacy in Australian Vietnam veterans with PTSD was more than double that of the general population [25], and was associated with increased PTSD symptom severity, comorbid depression and concurrent suicidality. In Australia, quality data on psychotropic medication prescribing for PTSD, particularly in association with comorbidities, are currently lacking. Further Australian studies are essential to understand psychotropic polypharmacy and associated risk due to drug–drug or drug–disease interactions and adverse drug reactions related to pharmacotherapeutic treatment of PTSD.
2 Aims
The primary aim of this study was to investigate the prevalence of psychotropic polypharmacy in veterans with PTSD upon admission to an Australian inpatient mental health treatment facility, and to report the prevalence of class combinations, including intra-class polypharmacy. The secondary aim was to illustrate potential risks associated with polypharmacy in this population. Through utilising a hospitalised population, we can identify prescribing patterns in individuals with more severe psychopathology, for whom pharmacotherapy is likely to be more complex. This is an early step in the process of improving pharmacotherapeutic treatment of PTSD, reducing unnecessary overprescribing and addressing a modifiable contributor to morbidity and mortality rates in individuals with PTSD.
3 Methods
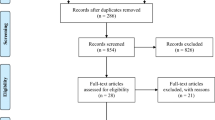
Medical records of patients admitted for the treatment of PTSD, as identified by the Health Information Services Admission Diagnosis, within the time frame 1 January, 2019–1 January, 2020 to an ADF veteran facility were reviewed. Approval for this study was received from the Departments of Defence and Veterans’ Affairs Human Research Ethics Committee (DDVA HREC/OUT/2020/BN18528191). A waiver of participant consent under National Statement paragraph 2.3.10 was also approved by this committee, as all data were de-identified. Demographic details for each participant (age, sex and any psychiatric and physical comorbidities) were recorded, as well as a list of all medications documented on the date of the first admission (including medication type, dose, frequency, indication and duration).
Medications were coded according to their Anatomical Therapeutic Chemical Classification (ATC) class [26]. The total number of medications prescribed to patients were recorded, including those prescribed to be taken as needed, pro re nata, as well as the total number of psychotropic medications, and total number of medications with sedative effects. The prevalence of general, psychotropic and sedative polypharmacy was calculated. We defined general polypharmacy as concurrent use of five or more medications, and psychotropic and sedative polypharmacy as concurrent use of two or more psychotropic or sedative medications, respectively [1]. Psychotropic medications were defined as those in ATC class “N” owing to their effect on the nervous system, and grouped into different medication classes according to third-level ATC codes. Anaesthetics (NO1) and other analgesics (NO2B), including paracetamol were not included as a psychotropic medication as they are not psychoactive and not generally used for psychiatric purposes. Prochlorperazine (NO5) was not included as a psychotropic medication as it is primarily prescribed for its anti-emetic and anti-nauseant properties. Sedative medications were those that were ATC coded as sedatives or were listed by previous authors as having primary or secondary sedative effects [27]. Therefore, this count also includes psychotropic medications with sedative effects.
Between-class combinations of psychotropic medications were reported, as well as within-class combinations. To more accurately determine within-class polypharmacy, we defined lithium (NO5AN) as its own class rather than as an antipsychotic, and included benzodiazepines in the hypnotics and sedative class (NO5CD) with anxiolytics (NO5B).
The Drug Burden Index (DBI), a measure that quantifies the cumulative burden of anticholinergic and sedative medications [28], was calculated for patients based on the medications recorded at admission. Using the Australian product information, all medications with an anticholinergic and/or sedative effect were identified [29]. The DBI for each regular anticholinergic and/or sedative medication was calculated and a total DBI was derived for each patient using the below equation [30], in which D is the daily dose taken by the patient and ∂ is the minimum effective daily dose:
Higher DBI scores show a greater drug burden from medications with anticholinergic and/or sedative effects. The DBI was summarised as median (inter-quartile range), and the proportions of patients with no (0), low (> 0 and < 1) and high (≥ 1) DBI were also reported [31].
Further analyses using logistic regression were performed to determine any associations between veterans’ demographic characteristics and general polypharmacy, psychotropic polypharmacy and sedative polypharmacy. Associations were adjusted for age, sex, total number of medications (except for general polypharmacy analysis), total number of other psychiatric conditions and total number of non-psychiatric medical conditions. An adjusted weighted multiple linear regression was used to determine associations between veterans’ demographic characteristics and the DBI. Associations were adjusted for age, sex, total number of non-psychiatric medical conditions, total number of other psychiatric conditions, total number of medications and total number of psychotropic medications. The final model was checked for homoscedasticity, multicollinearity, normality and independence of errors.
Incidences of potential drug–drug interactions were determined by the use of the MIMS (Monthly Index of Medicine Specialties) online drug interaction checking software. A drug–drug interaction was only noted if the combination of medications could cause an interaction that was considered “well-established” and had a severity level of “1” (meaning it could be clinically significant) on the drug interaction checking software.
4 Results
The population of 219 patients admitted during the study period of 1 year was predominantly male (97.3%), with a mean age (± standard deviation) of 62.5 (±14.6) years, and a range from 26 to 93 years. In addition to PTSD, 90.9% of the population had a diagnosis of another psychiatric condition, the most common being depression (78.1%), and 96.8% had a diagnosis of at least one non-psychiatric medical condition, most commonly chronic musculoskeletal pain (58.4%) (Table 1).
General polypharmacy was highly prevalent in this population (168 of 219, 76.7%). Additionally, the prevalence of psychotropic polypharmacy was high, with 175 of 219 participants (79.9%) prescribed two or more psychotropic medications, and the prevalence of sedative polypharmacy was also high with 165 participants (75.3%) prescribed two or more of these medications (Table 2).
Antidepressants were the most commonly prescribed psychotropic medications (84.9% [n = 186] of participants were taking antidepressants), followed by anxiolytics (49.3% [n = 108] of participants). Opioids, antipsychotics and antiepileptics were prescribed at similar rates (35.6% [n = 78], 31.5% [n = 69] and 28.8% [n = 63] of the population) [Table S1 of the Electronic Supplementary Material (ESM)].
The most commonly prescribed combinations of psychotropic medications were antidepressants with anxiolytics (45.7%, n = 100), followed by antidepressants and opioids (32.0%, n = 70), antidepressants and antipsychotics (28.8%, n = 63) and antidepressants and antiepileptics (25.1%, n = 55). Anxiolytics were prescribed with opioids in 22.8% (n = 50) of participants, and with antipsychotics in 17.4% (n = 38) of participants (Table 3).
Within-class polypharmacy was most common for antidepressants, with 22.4% (n = 49) being prescribed two or more antidepressants (Table 3). The most common antidepressant combinations included desvenlafaxine (SNRI) or venlafaxine (SNRI) with mirtazapine (atypical antidepressant) [n = 20 patients]. Agomelatine (atypical antidepressant) was included in nine of the 24 different antidepressant class combinations (n = 13 patients). The three selective serotonin reuptake inhibitors most commonly recommended for first-line pharmaceutical management of PTSD (fluoxetine, sertraline and paroxetine) are seen in five of the 24 different antidepressant class combinations (n = 5 patients) (Table S2 of the ESM). The level of within-class polypharmacy noted with antidepressants can provide some indication about the responsiveness of the patient to recommended guideline approaches for the pharmaceutical management of PTSD.
Drug Burden Index scores in this population ranged from 0 to 8.2, with 93.6% taking at least one DBI-associated medication (Table 4). In the adjusted weighted multiple linear regression analysis, DBI was significantly associated with sex, total number of medications and total number of psychotropic medications (Table S3 of the ESM).
Logistic regression analyses showed that age, and total number of medications were significantly associated with psychotropic polypharmacy. For each unit increase in age (years), the odds of psychotropic polypharmacy decrease by 6%, and for each additional medication prescribed in this cohort, the odds of psychotropic polypharmacy increase by 51% (Table S4 of the ESM). It was also shown that the total number of non-psychiatric medical conditions was significantly associated with general polypharmacy. For each additional non-psychiatric medical condition reported, the odds of general polypharmacy increase by 59% (Table S5 of the ESM). Logistic regression analyses also showed that for each unit increase in age (years), the odds of sedative polypharmacy decrease by 4%, and for each additional medicine prescribed in this cohort, the odds of sedative polypharmacy increased by 49% (Table S6 of the ESM).
According to MIMS classifications, 50 patients (22.8%) were taking one or more combinations of drugs that could have resulted in a clinically significant drug–drug interaction. The total incidence of potential drug–drug interactions in the cohort was 77 drug combinations.
5 Discussion
In this cohort of 219 ADF veterans admitted to an inpatient mental health facility for the management of PTSD, there was a high prevalence of psychotropic polypharmacy (79.9%). This is over three and a half times that of the general population (22.6%) [9] and almost two and a half times more than a previously studied population of Australian Vietnam veterans with PTSD (33.1%) [25]. Greater than three quarters of veterans in this study were taking five or more medications of all classes, and over three quarters were taking two or more medications with sedative effects. More than two thirds had a high DBI. These results highlight the challenges encountered by prescribing clinicians in managing this complex patient population (who commonly present with numerous psychological and physical comorbidities requiring pharmaceutical interventions), and illustrate the risks of adverse drug-related complications that these patients are exposed to. Previously, Theal et al. noted that, in a population of community-dwelling Vietnam veterans with PTSD, psychotropic polypharmacy was associated with increased PTSD severity, comorbid major depressive disorder and increased suicide risk [25]. Although we were unable to determine the severity of PTSD, the higher rates of psychotropic polypharmacy reported in this population may be due to more severe levels of PTSD that require admission to a mental health facility for acute management, more complex psychopathology, possible unresponsiveness to conventional first-line approaches to management such as cognitive behavioural therapy, and high levels of comorbid depression.
Antidepressants were the most common medications involved in psychotropic polypharmacy class combinations. Opioids were the second most common, possibly owing to the study population manifesting high rates of comorbid chronic musculoskeletal pain (58.4%). In a population of community-dwelling Australian Vietnam veterans with PTSD, antidepressants were also the most common medication in polypharmacy combinations but to a lesser degree [25]. This prescribing pattern in veterans differs from the general Australian population, in which antiepileptics and atypical antipsychotics are the most common medications involved in psychotropic polypharmacy combinations [9]. Additionally, the prescribing prevalence of benzodiazepines and opioids in this study is higher than that reported for veterans with PTSD in the USA. Bernardy and colleagues reported US figures in excess of 30% for benzodiazepines or opioids individually and nearly 16% in combination [17], whilst our results reported 47% and 35.6%, respectively, and 21% in combination.
Anxiolytics (including benzodiazepines) were the most commonly prescribed psychotropic medication with antidepressants (43.8%). They were also prescribed with opioids in over a fifth of the population. The use of benzodiazepines is not recommended by the Veterans Affairs Department of Defence for the primary treatment of PTSD [21], nor does it recommend them as augmentation therapy, owing to the lack of evidence for effectiveness and because risks outweigh potential benefits. The US guidelines also recommend avoidance of concurrent prescribing of opioids and specifically benzodiazepines based on established adverse risks such as respiratory depression, subsequently associated with overdose deaths, altered mental states, and postural stability associated with falls and fractures in those aged over 65 years [32]. Benzodiazepine use is associated with tolerance and dependence, thus it can be difficult to discontinue these medications because of significant withdrawal symptoms [33]. Benzodiazepines are also contraindicated in patients with a history of traumatic brain injury, sleep apnoea, chronic obstructive pulmonary disorder or substance abuse disorder [34]. In this cohort, 68.4% of participants with one or more of these conditions had been prescribed benzodiazepines. The increased prescription of benzodiazepines in an inpatient sample is not unexpected given elevated symptom acuity and the drugs’ sedating and short-term anxiolytic effects; however, the above comorbid conditions are prevalent in our inpatient sample, and the cohort had an average age above 60 years, raising questions about prescribing practice. Despite the existing recommendations against their use in PTSD, benzodiazepines are still widely prescribed off-label for PTSD, other mental health conditions and chronic pain [35]. This common practice has been reported in up to 30–74% of cases of patients with PTSD, with advocates arguing that the effective symptomatic management with benzodiazepines for the anxiety and insomnia associated with PTSD makes them necessary for treatment-resistant patients with severe symptoms. However, these short-term benefits are at the cost of prolonging and worsening other features of PTSD in the long term [34], and reducing the efficacy of cognitive behavioural therapy, the current gold-standard treatment for PTSD [20]. The proportion of participants prescribed anxiolytics with opioids is also not unexpected, considering the prevalence of chronic pain in this population- 36 participants with chronic pain (28%) were taking this combination. Associations between psychotropic medication use and prescription opioid use have been described previously [36, 37]. Nevertheless, it is concerning, as concurrent use of opioids and benzodiazepines increases the risk of falls/fractures and emergency department visits [37].
Combination antidepressant therapy or augmentation of antidepressants with second-generation antipsychotics have become accepted strategies in the management of treatment-resistant depression [38, 39], and the US Food and Drug Administration has approved the use of one of four second-generation antipsychotics (aripiprazole, quetiapine, olanzapine plus fluoxetine, and brexpiprazole) for augmented or adjunctive treatment of depressed adults who do not respond adequately to antidepressants alone. In our cohort, over one fifth were taking two or more antidepressants, suggesting higher rates of difficult-to-treat depressive symptoms. However, taking multiple serotonergic antidepressants conveys a theoretical risk of serotonin toxicity, and this risk is elevated further when other medications that affect the serotonin system are also added (e.g. tramadol, tapentadol, cyproheptadine or pseudoephedrine) [40]. Almost a third of this population were prescribed antipsychotics with antidepressants, which again suggests higher rates of difficult-to-treat depressive symptoms in this population with PTSD.
To further illustrate the degree of risk of functional impairment from medications with anticholinergic and sedative effects, we calculated the DBI. Higher DBI has been associated with physical function impairment, hospitalisation, frailty and mortality in older adults [28], and each unit increase of DBI has a negative effect on physical function similar to that of three additional physical morbidities [28]. In our cohort, over 90% of patients were exposed to a DBI-associated medication, which is higher than the prevalence rates of up to 83% reported in other Australian and international studies of older people in different settings [27, 41,42,43]. Of note, the most frequently prescribed classes of medications in this cohort (antidepressants, anxiolytics including benzodiazepines, opioids and antipsychotics) all have the potential for both anticholinergic and sedative effects and are included in the calculation of the DBI.
In this population, the odds of psychotropic polypharmacy increased significantly with every additional medication prescribed. The occurrence of psychotropic polypharmacy in PTSD can be unavoidable in people who are treatment resistant and present with numerous comorbid psychiatric conditions. For example, the augmentation of antidepressants with benzodiazepines is recognised as appropriate treatment in acute inpatient management of comorbid depression, anxiety, and insomnia or other sleep disorders in people not responsive to first-line approaches. One US study investigating trends of psychotropic polypharmacy in adults with depressive disorders was able to justify 53.9% of between-class psychotropic prescriptions on the basis of treatment of psychiatric comorbidities [44]. However, it is when this medication regime continues beyond a hospital stay and/or becomes long term where problems can occur. Psychiatric comorbid conditions are common in our cohort, highlighting the challenges faced when delivering evidence-based treatments to veteran populations, particularly when there is little guidance to support clinical decision making when patients with PTSD have an atypical and/or complex presentation, do not respond to first-line or second-line treatments for psychosocial problems, or experience other physical comorbidities [45]. In our cohort, the total number of non-psychiatric medical comorbidities also significantly increased the odds of general polypharmacy.
A conceptual framework developed by Phoenix Australia to guide the implementation of best practice in services for veterans with PTSD acknowledges the paucity of guidance available to clinicians when best managing comorbid conditions, and the challenges in coordinating care [46]. It emphasises the importance of veterans’ mental health service systems having the best possible care coordination models in place to facilitate communication between providers, veterans and their families. At a more individual level, approaches to addressing these issues may include prescribers taking advantage of the use of programmes such as electronic real-time prescription monitoring and national electronic health records. The Australian Government Department of Health provides a webpage (National Real Time Prescription Monitoring) [47] with information for doctors and pharmacists about a patient’s history and the use of controlled medications when they are considering prescribing or dispensing these medicines. A home medicines review by an accredited pharmacist [48] can assist in minimising adverse medicine events by helping people to better understand and manage their medicines. This may also prompt prescribers to de-prescribe medications no longer effective or necessary. Recently, the Pharmacy Programs Administrator Program Rules were updated to allow hospital-based medical practitioners to refer patients to an accredited pharmacist for a home medicines review [49], which is an ideal initiative for specialists to help regulate polypharmacy in their veteran PTSD population. The development and distribution of simple resources (such as pocket cards) to primary care providers for pharmacological management of PTSD with other comorbid conditions may be helpful [50]. Obtaining a thorough medical history by the provider before a new drug prescription is essential to make appropriate management decisions, and the use of educational resources, such as the Beers Criteria would assist in appropriate medication prescription choices in older adults [51]. Additionally, more emphasis should be placed on implementing and persevering with non-pharmacological interventions such as psychosocial interventions and physical exercise.
This is the first study, to our knowledge, reporting the prevalence of general, psychotropic and sedative polypharmacy in a hospitalised sample of Australian veterans with PTSD. It highlights a readily modifiable clinical issue that can affect potential morbidity and mortality amongst inpatient veteran populations with PTSD and related comorbidities (and by extension, broader inpatient and outpatient populations in the veteran and general population). In addition to describing the prevalence of general, psychotropic and sedative polypharmacy in this population, we have attempted to quantify the potential for risk of functional impairment, hospitalisation and mortality by using an established measure (the DBI), which is readily available to clinicians as a clinical risk assessment tool [30]. By recognising the cumulative exposure of a patient to medications that could contribute to the individual’s functional impairment, the clinician can weigh the associated risks against the potential benefits of the medications and prescribing can be optimised to minimise drug-related functional impairment.
There are a number of study limitations to consider in the interpretation of these results. This medical record review is a snapshot of the medications reported on admission to a mental health facility, and we did not document treatment health outcomes or adverse event rates. The number of possible drug–drug interactions was calculated using an online drug interaction checking software; however, as these were retrospective data, we were unable to definitively determine if patients actually experienced a clinically meaningful drug–drug interaction. We extracted inpatient admission data from paper charts only, which lacked some details regarding duration and indication of drug therapy (because of the quality of the admission notes) and did not access other electronic sources, thus we may have under-reported total medication usage. Information is lacking on the number of prescribers involved in treating these patients, or whether there is a single clinician responsible for overseeing the patient’s medication regime. As not all indications for the prescription of each medication were evident, we cannot definitively determine prescribing appropriateness. Our comments on the use of drug combinations are based on the available literature; however, we understand that real-world prescribing can often be innovative and based on appropriate clinical grounds for an individual patient but has not yet established an evidence base.
6 Conclusions
This cohort of ADF veterans admitted to a mental health facility for the treatment of PTSD had a high prevalence of general, psychotropic and sedative polypharmacy, and were at high risk for drug-related serious adverse events. These findings highlight the necessity of ongoing caution around polypharmacy and potentially inappropriate drug combinations, particularly in the veteran population with comorbid psychiatric and physical conditions. Increasing awareness of the potential consequences of psychotropic polypharmacy, regular monitoring of medications by clinicians, pharmacists and other relevant health professionals, and improved communication between prescribers is required. Given the current focus on Australian veteran suicide rates, and the finding in US veterans that the risk of fatal accidental medication-related self-poisoning outstrips that of veteran suicide, we suggest the issue of polypharmacy, a more readily modifiable action, be addressed in a more comprehensive manner.
References
Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230.
Liao PJ, Mao CT, Chen TL, et al. Factors associated with adverse drug reaction occurrence and prognosis, and their economic impacts in older inpatients in Taiwan: a nested case-control study. BMJ Open. 2019;9(5):e026771.
Pharmaceutical Society of Australia. Medicine safety: take care. Canberra: Pharmaceutical Society of Australia; 2019. https://www.psa.org.au/wp-content/uploads/2019/01/PSA-Medicine-Safety-Report.pdf. Accessed 29 Mar 2022.
Australian Institute of Health and Welfare. Injury in Australia: accidental poisoning: Australian Government; 2021 [updated 9th December 2021]. https://www.aihw.gov.au/reports/injury/accidental-poisoning. Accessed 29 Mar 2022.
Bohnert AS, Ilgen MA, Galea S, et al. Accidental poisoning mortality among patients in the Department of Veterans Affairs Health System. Med Care. 2011;49(4):393–6.
Brett J, Daniels B, Karanges EA, et al. Psychotropic polypharmacy in Australia, 2006 to 2015: a descriptive cohort study. Br J Clin Pharmacol. 2017;83(11):2581–8.
Aged Care Quality and Safety Commission. Psychotropic medications used in Australia: information for aged care. Australian Government; 2020. agedcarequality.gov.au; acqsc_psychotropic_medications_v11.pdf. Accessed.
Brett J, Karanges EA, Daniels B, et al. Psychotropic medication use in Australia, 2007 to 2015: changes in annual incidence, prevalence and treatment exposure. Aust N Z J Psychiatry. 2017;51(10):990–9.
Brett J, Pearson SA, Daniels B, et al. A cross sectional study of psychotropic medicine use in Australia in 2018: a focus on polypharmacy. Br J Clin Pharmacol. 2021;87(3):1369–77.
Brett J, Zoega H, Buckley NA, et al. Choosing wisely? Quantifying the extent of three low value psychotropic prescribing practices in Australia. BMC Health Serv Res. 2018;18(1):1009.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington (VA): American Psychiatric Publishing; 2013.
Therapeutic Guidelines Limited. Mental health disorders following trauma exposure. eTG complete. 2019; June. https://www.tg.org.au. Accessed 29 Mar 2022.
McLeay SC, Harvey WM, Romaniuk MN, et al. Physical comorbidities of post-traumatic stress disorder in Australian Vietnam War veterans. Med J Aust. 2017;206(6):251–7.
Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder: epidemiology, impact and approaches to management. CNS Drugs. 2006;20(7):567–90.
Beckham JC, Crawford AL, Feldman ME, et al. Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. J Psychosom Res. 1997;43(4):379–89.
Shipherd JC, Keyes M, Jovanovic T, et al. Veterans seeking treatment for posttraumatic stress disorder: what about comorbid chronic pain? J Rehabil Res Dev. 2007;44(2):153–66.
Bernardy NC, Lund BC, Alexander B, et al. Prescribing trends in veterans with posttraumatic stress disorder. J Clin Psychiatry. 2012;73(3):297–303.
International Society for Traumatic Stress Studies. ISTSS PTSD guidelines: methodology and recommendations. Illinois, USA, 2018. www.istss.org. Accessed 29 Mar 2022.
National Institute of Health and Care Excellence. Post-traumatic stress disorder: NICE guidelines NG116. 2018. https://www.nice.org.uk/guidance/ng116. Accessed 29 Mar 2022.
Phoenix Australia. Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. 2013. www.phoenixaustralia.org. Accessed 29 Mar 2022.
US Department of Veterans Affairs and Department of Defence. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Washington DC. 2017. https://www.healthquality.va.gov/guidelines/mh/ptsd/. Accessed 29 Mar 2022.
Hovstadius B, Petersson G. Factors leading to excessive polypharmacy. Clin Geriatr Med. 2012;28(2):159–72.
Abrams TE, Lund BC, Bernardy NC, et al. Aligning clinical practice to PTSD treatment guidelines: medication prescribing by provider type. Psychiatr Serv. 2013;64(2):142–8.
Van Hooff M, Lawrence-Wood E, Hodson S, et al. Mental health prevalence, mental health and wellbeing transition study. Department of Defence and Department of Veterans' Affairs. Canberra 2018. www.dva.gov.au/mental-health-prevalence-report. Accessed 29 Mar 2022.
Theal R, McLeay S, Gibson JM, et al. Psychotropic polypharmacy in Australian Vietnam War veterans with post-traumatic stress disorder: a descriptive cohort study. J Military Veterans Health. 2020;28(4):34–45.
World Health Organization. WHO Collaborating Centre for Drug Statistics Methodology: ATC/DDD classification (temporary). WHO Drug Inf. 2019;33(2):226–32.
Byrne CJ, Walsh C, Cahir C, et al. Anticholinergic and sedative drug burden in community-dwelling older people: a national database study. BMJ Open. 2018;8(7):e022500.
Hilmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781–7.
Kouladjian L, Gnjidic D, Chen TF, et al. Drug Burden Index in older adults: theoretical and practical issues. Clin Interv Aging. 2014;9:1503–15.
Hilmer SN. Calculating and using the drug burden index score in research and practice. Expert Rev Clin Pharmacol. 2018;11(11):1053–5.
Gnjidic D, Hilmer SN, Hartikainen S, et al. Impact of high risk drug use on hospitalization and mortality in older people with and without Alzheimer’s disease: a national population cohort study. PLoS ONE. 2014;9(1):e83224.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain: United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49.
Petursson H. The benzodiazepine withdrawal syndrome. Addiction. 1994;89(11):1455–9.
Guina J, Rossetter SR, De Rhodes BJ, et al. Benzodiazepines for PTSD: a systematic review and meta-analysis. J Psychiatr Pract. 2015;21(4):281–303.
Pergolizzi JV, LeQuang JA. Reappraising the use of benzodiazepines in chronic pain patients. Postgrad Med. 2020;132(sup3):10–2.
Skurtveit S, Furu K, Bramness J, et al. Benzodiazepines predict use of opioids: a follow-up study of 17,074 men and women. Pain Med. 2010;11(6):805–14.
Musich S, Wang SS, Slindee LB, et al. Concurrent use of opioids with other central nervous system-active medications among older adults. Popul Health Manag. 2020;23(4):286–96.
Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–17.
Kato M, Chang CM. Augmentation treatments with second-generation antipsychotics to antidepressants in treatment-resistant depression. CNS Drugs. 2013;27:S11–9.
Roughead EE, McDermott B, Gilbert AL. Antidepressants: prevalence of duplicate therapy and avoidable drug interactions in Australian veterans. Aust N Z J Psychiatry. 2007;41(4):366–70.
Gnjidic D, Hilmer SN, Blyth FM, et al. High-risk prescribing and incidence of frailty among older community-dwelling men. Clin Pharmacol Ther. 2012;91(3):521–8.
Shafiee Hanjani L, Hubbard RE, Freeman CR, et al. Medication use and cognitive impairment among residents of aged care facilities. Intern Med J. 2021;51(4):520–32.
Nishtala PS, Narayan SW, Wang T, et al. Associations of drug burden index with falls, general practitioner visits, and mortality in older people. Pharmacoepidemiol Drug Saf. 2014;23(7):753–8.
Rhee TG, Rosenheck RA. Psychotropic polypharmacy reconsidered: between-class polypharmacy in the context of multimorbidity in the treatment of depressive disorders. J Affect Disord. 2019;252:450–7.
Phoenix Australia - Centre for Post-Traumatic Mental Health. Australian guidelines for the prevention and treatment of acute stress disorder, posttraumatic stress disorder and complex posttraumatic stress disorder. Melbourne. 2020. www.phoenixaustralia.org. Accessed 29 Mar 2022.
Phoenix Australia—Centre for Post-Traumatic Mental Health and the Canadian Centre of Excellence —PTSD. The conceptual framework to guide the implementation of best and next practice in services and supports for veterans and their families. 2020. phoenixaustralia.org/wp-content/uploads/2020/12/TecDoc_VeteranServices.pdf. Accessed 29 Mar 2022.
Department of Health. National real time prescription monitoring (RTPM): Australian Government; 2022. https://www.health.gov.au/initiatives-and-programs/national-real-time-prescription-monitoring-rtpm#. Accessed 29 Mar 2022.
Pharmacy Programs Administrator. Home medicines review: Australian Healthcare Associates; 2018. https://www.ppaonline.com.au/programs/medication-management-programs/home-medicines-review. Accessed 29 Mar 2022.
Pharmacy Programs Administrator. Program rules: residential medication management review. Australian Government Department of Health; 2021. https://www.ppaonline.com.au/programs/medicationmanagement-programs/residential-medication-management-review-and-quality-use-of-medicines. Accessed 29 Mar 2022.
Baig MR, Meraj A, Tapia RN. Development of a practice tool for primary care providers: medication management of posttraumatic stress disorder in veterans with mild traumatic brain injury. Psychiatr Q. 2020;91(4):1465–78.
The American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
Acknowledgements
We acknowledge Anousheh Page for coordinating pharmacy support for this project, and the Ramsay Hospital Research Foundation for awarding a grant to complete this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This project was funded by a grant received from the Ramsay Hospital Research Foundation, 16 April, 2020.
Conflicts of interest/competing interests
No conflicts of interest were declared by the authors RM, AK, ES, ER, MT, LSH, CF and DC. ER was supported for her contribution to the paper by the Ramsay Hospital Research Foundation grant.
Ethics approval
Approval for this study was received from the Departments of Defence and Veterans’ Affairs Human Research Ethics Committee (DDVA HREC/OUT/2020/BN18528191). A waiver of participant consent under National Statement paragraph 2.3.10 was also approved by this committee, as all data was de-identified.
Consent to participate
A waiver of participant consent under National Statement paragraph 2.3.10 was approved by the Departments of Defence and Veterans’ Affairs Human Research Ethics Committee (DDVA HREC/OUT/2020/BN18528191), as all data was de-identified.
Consent for publication
Not applicable for this study.
Availability of data and material
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
RM coordinated the project, interpreted the data and drafted the final manuscript; ESD and ER extracted, organised and interpreted the data; MWT, LSH and CF analysed and interpreted the data; and AK, CF and DC provided clinical interpretation and perspective. All authors reviewed and contributed to the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mellor, R., Khoo, A., Saunders-Dow, E. et al. Polypharmacy in Australian Veterans with Post-traumatic Stress Disorder upon Admission to a Mental Health Facility: A Retrospective Chart Review. Drugs - Real World Outcomes 9, 347–357 (2022). https://doi.org/10.1007/s40801-022-00298-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00298-3