Abstract
Background
Diagnostic standards and codes related to excessive weight exist so that clinicians may inform patients that they are overweight: a status which may be a harbinger of more severe obesity and negative health outcomes. Equipped with this knowledge, patients may pursue medical interventions or behavioral changes to reduce their risk. However, diagnoses of overweight are unequally applied in the United States along racial lines.
Methods
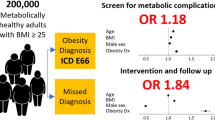
Binary logistic regression was used to analyze National Health and Nutrition Examination Survey (NHANES) 2009–2016 data from 7460 participants to examine the relationship between race of non–Hispanic White and non–Hispanic Black Americans and having ever been told that one is overweight by a clinician when controlling for demographic and socioeconomic factors. The body mass index (BMI) of participants along with obesity-associated comorbidities was then incorporated into the model to see if physical size or disease status mediated the primary relationship.
Results
Black Americans are significantly less likely to report being told that they are overweight by a clinician than are White Americans regardless of clinical weight status and weight-associated comorbidities. We find that these racial differences are greatest when respondents’ BMIs approach the lower threshold for clinical obesity.
Conclusions
Our findings suggest that the lower likelihood of Black Americans to be told they are overweight compared to their White counterparts can result in serious health implications. We posit that implicit biases among clinicians may partly explain this disparity, which may exacerbate health outcome inequalities.

Similar content being viewed by others
Notes
Among other applications, BMI also allows researchers to compare groups of different height and body compositions to one another, which was in fact its original purpose.
Although “overweight” and “obese” are two discrete categories by today’s standards, this was not always the case in the twentieth century. At times, any BMI or other corporeal status that exceeded what was considered clinically desirable was classed as simply “overweight” [67]. This has led to a kind of rectangle-and-square relationship between the two terms in lay speak, with some writers and observers casually noting percentages of Americans who are “overweight” and then specifying that a percentage of that group is in fact “obese.” This is technically improper, but it implies that we often think of obesity simply as a more extreme form of overweight, which is not an unreasonable position to take.
References
Nuttall FQ. Body Mass Index. Nutr Today. 2015;50:117–28.
Ogden CL, Fryar CD, Carroll MD, Flegal KM. Mean body weight, height, and body mass index, United States 1960–2002. Adv Data. 2004. p. 1–17.
Fryar CD, Kruszon-Moran D, Gu Q, Ogden CL. Mean body weight, height, waist circumference, and body mass index among adults: United States, 1999–2000 Through 2015–2016. Natl Health Stat Report. 2018. p. 1–16.
National Center for Health Statistics (US). Health, United States, 2015: with special feature on racial and ethnic health disparities [Internet]. Hyattsville (MD): National Center for Health Statistics (US); 2016 [cited 2021 Nov 28]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK367640/
Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–41.
Saguy A. What’s wrong with fat?: the war on obesity and its collateral damage [Internet]. New York: Oxford University Press; 2013 [cited 2021 Nov 28]. Available from: https://oxford.universitypressscholarship.com/https://doi.org/10.1093/acprof:oso/9780199857081.001.0001/acprof-9780199857081
National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med. 2000;160:898–904.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9.
Kushner RF, Foster GD. Obesity and quality of life. Nutrition. 2000;16:947–52.
Krueger PM, Rogers RG, Hummer RA, Jason D. Boardman. Body mass, smoking, and overall and cause-specific mortality among older U.S. adults - 2004 [Internet]. [cited 2021 Nov 28]. Available from: https://journals-sagepub-com.libproxy.temple.edu/doi/https://doi.org/10.1177/0164027503258518
Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Xia JY, Lloyd-Jones DM, Khan SS. Association of body mass index with mortality in cardiovascular disease: new insights into the obesity paradox from multiple perspectives. Trends Cardiovasc Med. 2019;29:220–5.
Bosello O, Donataccio MP, Cuzzolaro M. Obesity or obesities? Controversies on the association between body mass index and premature mortality. Eat Weight Disord. 2016;21:165–74.
Tsatsoulis A, Paschou SA. Metabolically healthy obesity: criteria, epidemiology, controversies, and consequences. Curr Obes Rep. 2020;9:109–20.
Goacher PJ, Lambert R, Moffatt PG. Can weight-related health risk be more accurately assessed by BMI, or by gender specific calculations of percentage body fatness? Med Hypotheses. 2012;79:656–62.
Bennett G, Wolin K, Duncan D. Social determinants of obesity. In: Hu F, editor. Obesity Epidemiology. Oxford, UK: Oxford University Press; 2008. p. 342–76.
Javed Z, Valero-Elizondo J, Maqsood MH, Mahajan S, Taha MB, Patel KV, et al. Social determinants of health and obesity: findings from a national study of US adults. Obesity (Silver Spring). 2022;30:491–502.
Park S, Pan L, Lankford T. Relationship between employment characteristics and obesity among employed U.S. adults. Am J Health Promot. 2014;28:389–96.
Ghosh-Dastidar B, Cohen D, Hunter G, Zenk SN, Huang C, Beckman R, et al. Distance to store, food prices, and obesity in urban food deserts. Am J Prev Med. 2014;47:587–95.
Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102:1644–54.
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319:1723–5.
Yusuf ZI, Dongarwar D, Yusuf RA, Bell M, Harris T, Salihu HM. Social determinants of overweight and obesity among children in the United States. Int J MCH AIDS. 2020;9:22–33.
2018 national healthcare quality and disparities report. :6.
Oh SS, Galanter J, Thakur N, Pino-Yanes M, Barcelo NE, White MJ, et al. Diversity in clinical and biomedical research: a promise yet to be fulfilled. PLoS Med. 2015;12:e1001918.
Medical apartheid : the dark history of medical experimentation on Black Americans from colonial times to the present / Harriet A. Washington. - Library Search [Internet]. [cited 2021 Nov 28]. Available from: https://librarysearch.temple.edu/catalog/991025794109703811
Wailoo K. How cancer crossed the color line. Oxford ; Oxford University Press, 2011.
Neal D, Magwood G, Jenkins C, Hossler CL. Racial disparity in the diagnosis of obesity among people with diabetes. J Health Care Poor Underserved. 2006;17:106–15.
Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7:130–8.
NHANES - about the National Health and Nutrition Examination Survey [Internet]. 2020 [cited 2022 Mar 15]. Available from: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm
Ferraro KF, Holland KB. Physician evaluation of obesity in health surveys: “who are you calling fat?” Soc Sci Med. 2002;55:1401–13.
Schwartz KL, Crossley-May H, Vigneau FD, Brown K, Banerjee M. Race, socioeconomic status and stage at diagnosis for five common malignancies. Cancer Causes Control. 2003;14:761–6.
Becker G, Newsom E. Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am J Public Health. 2003;93:742–8.
Khaodhiar L, McCowen KC, Blackburn GL. Obesity and its comorbid conditions. Clin Cornerstone. 1999;2:17–31.
Sullivan PW, Morrato EH, Ghushchyan V, Wyatt HR, Hill JO. Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S., 2000–2002. Diabetes Care. 2005;28:1599–603.
Pi-Sunyer FX. Comorbidities of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31:S602-608.
Bissell KL. I want to be thin, like you: gender and race as predictors of cultural expectations for thinness and attractiveness in women. Vis Commun Q. 2002;9:4–11.
Garner DM, Garfinkel PE, Schwartz D, Thompson M. Cultural expectations of thinness in women. SAGE Publications Inc; Psychol Rep. 1980;47:483–91.
Grossbard JR, Neighbors C, Larimer ME. Perceived norms for thinness and muscularity among college students: what do men and women really want? Eat Behav. 2011;12:192–9.
NW 1615 L. St, Washington S 800, Inquiries D 20036 U-419–4300 | M-857–8562 | F-419–4372 | M. Demographic trends and economic well-being [Internet]. Pew Research Center’s Social & Demographic Trends Project. 2016 [cited 2022 Feb 24]. Available from: https://www.pewresearch.org/social-trends/2016/06/27/1-demographic-trends-and-economic-well-being/
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat. 2013;2:1–24.
Chen T-C, Parker JD, Clark J, Shin H-C, Rammon JR, Burt VL. National Health and Nutrition Examination Survey: estimation procedures, 2011–2014. Vital Health Stat. 2018;2:1–26.
Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Arch Intern Med. 2009;169:313–4.
Boora SR, Nalla A, Jhaveri M, Sunkara T, Ona MA, Nigar S, et al. Prevalence and underdiagnosis of obesity: 2395. Off J Am Coll of Gastroenterol | ACG. 2015;110:S994.
Post RE, Mainous AG, Gregorie SH, Knoll ME, Diaz VA, Saxena SK. The influence of physician acknowledgment of patients’ weight status on patient perceptions of overweight and obesity in the United States. Arch Intern Med. 2011;171:316–21.
Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003–2008 study. Int J Obes (Lond). 2011;35:1063–70.
Baron RB. Telling patients they are overweight or obese: an insult or an effective intervention?: comment on “The influence of physician acknowledgment of patients’ weight status on patient perceptions of overweight and obesity in the United States”. Arch Intern Med. 2011;171:321–2.
Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28:1504–10.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci. 2016;113:4296–301.
Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–94.
Tait RC, Chibnall JT, Kalauokalani D. Provider judgments of patients in pain: seeking symptom certainty. Pain Med. 2009;10:11–34.
Mort EA, Weissman JS, Epstein AM. Physician discretion and racial variation in the use of surgical procedures. Arch Intern Med. 1994;154:761–7.
Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians’ beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis. 2004;43:350–7.
Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34:2874–80.
Hester N, Gray K. For Black men, being tall increases threat stereotyping and police stops. Proc Natl Acad Sci U S A. 2018;115:2711–5.
Hannon L. White colorism. Social Currents. SAGE Publications Inc; 2015;2:13–21.
Motro D, Evans JB, Ellis APJ, Benson III L. Race and reactions to women’s expressions of anger at work: examining the effects of the “angry Black woman” stereotype. Journal of Applied Psychology. US: American Psychological Association; 2022;107:142–52.
Kowalski CP, McQuillan DB, Chawla N, Lyles C, Altschuler A, Uratsu CS, et al. “The hand on the doorknob”: visit agenda setting by complex patients and their primary care physicians. J Am Board Fam Med. 2018;31:29–37.
Zulman DM, Kerr EA, Hofer TP, Heisler M, Zikmund-Fisher BJ. Patient-provider concordance in the prioritization of health conditions among hypertensive diabetes patients. J Gen Intern Med. 2010;25:408–14.
Jaen CR, Stange KC, Tumiel LM, Nutting, P. Missed opportunities for prevention: smoking cessation counseling and the competing demands of practice. J FamPract. 1997;45(4): 348–354. - Google Search [Internet]. [cited 2022 Mar 14]. Available from: https://www.google.com/search?q=Jaen%2C+CR%3B+Stange%2C+KC%3B+Tumiel%2C+LM%3B+Nutting%2C+P.+1997.+Missed+Opportunities+for+Prevention%3A+Smoking+Cessation+Counseling+and+the+Competing+Demands+of+Practice.+The+Journal+of+Family+Practice.+45(4)%3A+348-354.&rlz=1C5CHFA_enUS965US965&oq=Jaen%2C+CR%3B+Stange%2C+KC%3B+Tumiel%2C+LM%3B+Nutting%2C+P.+1997.+Missed+Opportunities+for+Prevention%3A+Smoking+Cessation+Counseling+and+the+Competing+Demands+of+Practice.+The+Journal+of+Family+Practice.+45(4)%3A+348-354.&aqs=chrome..69i57.114j0j7&sourceid=chrome&ie=UTF-8
Health, United States 2018 Chartbook. 2018;65.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9.
LaVeist TA, Carroll T. Race of physician and satisfaction with care among African-American patients. J Natl Med Assoc. 2002;94:937–43.
Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–37.
Burkhauser RV, Cawley J. Beyond BMI: the value of more accurate measures of fatness and obesity in social science research. J Health Econ. 2008;27:519–29.
Gutin I. In BMI we trust: reframing the body mass index as a measure of health. Soc Theory Health. 2018;16:256–71.
Kuczmarski RJ, Flegal KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72:1074–81.
Acknowledgements
Special thanks to Dr. Lin Zhu, Dr. Gretchen Condran, and Dr. CiAuna Heard for their invaluable assistance and feedback on this paper.
Author information
Authors and Affiliations
Contributions
Chuck Galli contributed to the study conception and design and data analysis. The first draft of the manuscript was written by Chuck Galli, and revision and editing of the manuscript was performed by Tiffany Li. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Table 6
Rights and permissions
About this article
Cite this article
Galli, C., Li, T. Racial Differences in Diagnosis of Overweight and Obesity: Results from the National Health and Nutrition Examination Survey (NHANES) 2009–2016. J. Racial and Ethnic Health Disparities 10, 1096–1107 (2023). https://doi.org/10.1007/s40615-022-01297-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01297-4



