Abstract
Objective
To evaluate the safety of fertility-sparing surgery (FSS) in reproductive women (younger than 50 years) with early epithelial ovarian cancer (EOC).
Methods
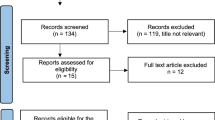
Reproductive women diagnosed with stage I EOC in the Surveillance, Epidemiology and End Results (SEER) database were identified. Surgeries that did not undergo hysterectomy and/or bilateral salpingo-oophorectomy were categorized as FSS, whereas non-FSS included bilateral salpingo-oophorectomy and hysterectomy. Propensity-score matching (PSM) was conducted to balance the covariates. Risk factor was identified by COX analysis. Kaplan–Meier curves were performed to evaluate the overall survival (OS) and cancer-specific survival (CSS).
Results
3556 patients with stage I EOC were identified and divided into non-FSS group and FSS group. After PSM, 625 pairs of patients with stage I EOC were included. FSS was not inferior to non-FSS in the OS curve [HR 0.9127, 95% CI (0.6971 ~ 0.1.195), P = 0.5174; HR: 0.9378, 95% CI (0.6358 ~ 0.1.383), P = 0.7460] and the CSS curve [HR 0.8284, 95% CI (0.5932 ~ 1.157), P = 0.2949; HR 0.9003, 95% CI (0.5470 ~ 1.482), P = 0.6803] both in overall cohort and in matched cohort. Univariate COX analysis identified older age (45–49), moderate-differentiated to un-differentiation grade, IC stage, bigger tumor size (> 10 cm) and chemotherapy as risk factors of prognostic outcome (P < 0.1). Not only in univariate subgroup analyses but also in bivariate factors subgroup analysis, the evidence was not enough to regard FSS as a harmful factor compared with non-FSS.
Conclusions
Fertility-sparing surgery was comparable to non-FSS in terms of survival in reproductive women with stage I EOC. Patients with high-risk factors could also consider FSS as an effective alternative compared with non-FSS.





Similar content being viewed by others
Data availability
All data were from the publicly available SEER database; no ethical approval was required.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Greenlee RT, Hill-Harmon MB, Murray T, Thun M (2001) Cancer statistics. CA Cancer J Clin 51(1):15–36. https://doi.org/10.3322/canjclin.51.1.15
National Cancer Institute. Surveillance, Epidemiology and End Results Program. Cancer stat facts: ovarian cancer. . https://seer.cancer.gov/statfacts/html/ovary.html. 2021.8
Moser EC, Meunier F (2014) Cancer survivorship: a positive side-effect of more successful cancer treatment. EJC Suppl 12(1):1–4. https://doi.org/10.1016/j.ejcsup.2014.03.001
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology [NCCN Guidelines]. Ovarian Cancer. https://www.nccn.org/professionals/physician_gls/default.aspx#site. July 28, 2021.
Schlaerth AC, Chi DS, Poynor EA, Barakat RR, Brown CL (2009) Long-term survival after fertility-sparing surgery for epithelial ovarian cancer. Int J Gynecol Cancer 19(7):1199–1204. https://doi.org/10.1111/IGC.0b013e31819d82c3
Wright JD, Shah M, Mathew L, Burke WM, Culhane J, Goldman N, Schiff PB, Herzog TJ (2009) Fertility preservation in young women with epithelial ovarian cancer. Cancer 115(18):4118–4126. https://doi.org/10.1002/cncr.24461
Crafton SM, Cohn DE, Llamocca EN, Louden E, Rhoades J, Felix AS (2020) Fertility-sparing surgery and survival among reproductive-age women with epithelial ovarian cancer in 2 cancer registries. Cancer 126(6):1217–1224. https://doi.org/10.1002/cncr.32620
Satoh T, Hatae M, Watanabe Y, Yaegashi N, Ishiko O, Kodama S, Yamaguchi S, Ochiai K, Takano M, Yokota H, Kawakami Y, Nishimura S, Ogishima D, Nakagawa S, Kobayashi H, Shiozawa T, Nakanishi T, Kamura T, Konishi I, Yoshikawa H (2010) Outcomes of fertility-sparing surgery for stage I epithelial ovarian cancer: a proposal for patient selection. J Clin Oncol 28(10):1727–1732. https://doi.org/10.1200/JCO.2009.24.8617
Gershenson DM (2012) Treatment of ovarian cancer in young women. Clin Obstet Gynecol 55(1):65–74. https://doi.org/10.1097/GRF.0b013e318248045b
Kohn JR, Katebi Kashi P, Acosta-Torres S, Beavis AL, Christianson MS (2021) Fertility-sparing surgery for patients with cervical, endometrial, and ovarian cancers. J Minim Invasive Gynecol 28(3):392–402. https://doi.org/10.1016/j.jmig.2020.12.027
Bercow A, Nitecki R, Brady PC, Rauh-Hain JA (2021) Outcomes after fertility-sparing surgery for women with ovarian cancer: a systematic review of the literature. J Minim Invasive Gynecol 28(3):527-536 e521. https://doi.org/10.1016/j.jmig.2020.08.018
Park JY, Suh DS, Kim JH, Kim YM, Kim YT, Nam JH (2016) Outcomes of fertility-sparing surgery among young women with FIGO stage I clear cell carcinoma of the ovary. Int J Gynaecol Obstet 134(1):49–52. https://doi.org/10.1016/j.ijgo.2015.10.022
Kajiyama H, Shibata K, Mizuno M, Hosono S, Kawai M, Nagasaka T, Kikkawa F (2011) Fertility-sparing surgery in patients with clear-cell carcinoma of the ovary: is it possible? Hum Reprod 26(12):3297–3302. https://doi.org/10.1093/humrep/der342
Nasioudis D, Chapman-Davis E, Frey MK, Witkin SS, Holcomb K (2017) Could fertility-sparing surgery be considered for women with early stage ovarian clear cell carcinoma? J Gynecol Oncol 28(6):e71. https://doi.org/10.3802/jgo.2017.28.e71
Austin PC, Fine JP (2019) Propensity-score matching with competing risks in survival analysis. Stat Med 38(5):751–777. https://doi.org/10.1002/sim.8008
Lalani N, Jimenez RB, Yeap B (2020) Understanding propensity score analyses. Int J Radiat Oncol Biol Phys 107(3):404–407. https://doi.org/10.1016/j.ijrobp.2020.02.638
Haukoos JS, Lewis RJ (2015) The propensity score. JAMA 314(15):1637–1638. https://doi.org/10.1001/jama.2015.13480
Kajiyama H, Suzuki S, Yoshikawa N, Kawai M, Mizuno K, Yamamuro O, Nagasaka T, Shibata K, Kikkawa F (2019) Fertility-sparing surgery and oncologic outcome among patients with early-stage ovarian cancer ~propensity score- matched analysis~. BMC Cancer 19(1):1235. https://doi.org/10.1186/s12885-019-6432-4
Sun H, Chen X, Zhu T, Liu N, Yu A, Wang S (2018) Age-dependent difference in impact of fertility preserving surgery on disease-specific survival in women with stage I borderline ovarian tumors. J Ovarian Res 11(1):54. https://doi.org/10.1186/s13048-018-0423-y
Fruscio R, Ceppi L, Corso S, Galli F, Dell’Anna T, Dell’Orto F, Giuliani D, Garbi A, Chiari S, Mangioni C, Milani R, Floriani I, Colombo N, Bonazzi CM (2016) Long-term results of fertility-sparing treatment compared with standard radical surgery for early-stage epithelial ovarian cancer. Br J Cancer 115(6):641–648. https://doi.org/10.1038/bjc.2016.254
Kajiyama H, Shibata K, Mizuno M, Umezu T, Suzuki S, Nawa A, Kawai M, Nagasaka T, Kikkawa F (2011) Long-term survival of young women receiving fertility-sparing surgery for ovarian cancer in comparison with those undergoing radical surgery. Br J Cancer 105(9):1288–1294. https://doi.org/10.1038/bjc.2011.394
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
QX and QL conceived of the presented idea and wrote the manuscript. QX and XM extracted the data from SEER database and analysed the data. QL verified the analytical methods and supervised the findings of this work. All authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xie, Q., Meng, X. & Liao, Q. Oncologic outcomes of fertility-sparing surgery in early stage epithelial ovarian cancer: a population-based propensity score-matched analysis. Arch Gynecol Obstet 306, 1679–1688 (2022). https://doi.org/10.1007/s00404-022-06536-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06536-x