Abstract
Objective
Rates of depression identification in oncology settings and referral to psychosocial services remain low. Patients with lung cancer face an elevated risk of depression relative to patients with other cancers. This study explored perceptions of somatic and affective symptoms and psychosocial care utilization among younger and older lung cancer survivors.
Methods
We conducted in-depth interviews with 20 adults at two academic medical centers in Boston, MA, who had received a lung cancer diagnosis in the past 24 months. A semi-structured interview guide was used to assess experiences with, and perceptions of, depression symptoms and psychosocial services. Interviews were audio-recorded, transcribed, and coded to identify themes. We also explored differences between younger (<65years; N=9) and older (>65years; N=11) patients.
Results
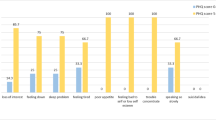
Participants commonly described somatic symptoms (i.e., changes in appetite, sleep, or energy levels) and affective symptoms (i.e., worry, fear, sadness) as side effects of cancer treatment. Older participants more commonly contextualized these symptoms with information about how they impacted daily life. Both younger and older participants faced barriers to accessing psychosocial services, with older adults more commonly referencing stigma of service referral and utilization.
Discussion
Patients with lung cancer associated both somatic and affective symptoms with their cancer and its treatment, with age differences in how symptoms were described and how psychosocial referrals may be perceived. More systematic integration of psychosocial care into cancer care may help to increase the identification of depression in lung cancer and reduce barriers to psychosocial service utilization.
Similar content being viewed by others
Data Availability
De-identified data is available upon request.
Code availability
Not applicable.
References
American Cancer Society (2020) Cancer Facts & Figures 2020. American Cancer Society, Atlanta
National Cancer Institute: Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Lung and Bronchus Cancer. Accessed on February 6, 2022. Accessed at https://seer.cancer.gov/statfacts/html/lungb.html
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2017/, based on November 2019 SEER data submission, posted to the SEER web site, April 2020.
McFarland DC, Holland JC (2016) The management of psychosocial issues in oncology. Clinc Adv Hematol Oncol 14(12):999–1009
Poghosyan H, Sheldon LK, Leveille SG, Cooley ME (2013) Health-related quality of life after surgical treatment in patients with non-small cell lung cancer: a systematic review. Lung Cancer (Amsterdam, Netherlands) 81(1):11–26
Steinberg T, Roseman M, Kasymjanova G et al (2009) Prevalence of emotional distress in newly diagnosed lung cancer patients. Support Care Cancer 17(12):1493–1497
Walsh K (2016) Addressing psychosocial issues in cancer survivorship: past, present and future. Future Oncol 12(24):2823–2834
Riedl D, Schuessler G (2021) Prevalence of depression and cancer - a systematic review. Z Psychosom Med Psychother OA11. https://doi.org/10.13109/zptm.2021.67.oa11
Martinez E, Tatum KL, Weber DM et al (2009) Issues related to implementing a smoking cessation clinical trial for cancer patients. Cancer Causes Control 20(1):97–104
Satin JR, Linden W, Phillips MJ (2009) Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer 115(22):5349–5361
Götze H, Brähler E, Gansera L, Polze N, Köhler N (2014) Psychological distress and quality of life of palliative cancer patients and their caring relatives during home care. Support Care Cancer 22:2775–2782
Trevino KM, Stern A, Hershkowitz R et al (2021) Managing Anxiety from Cancer (MAC): a pilot randomized controlled trial of an anxiety intervention for older adults with cancer and their caregivers. Palliat Support Care 19(2):135–145
Institute of Medicine (2007) Cancer care for the whole patient: meeting psychosocial health care needs. National Academies Press
Schuit AS, Holtmaat K, van Zwieten V et al (2021) Organizing psycho-oncological care for cancer patients: the patient’s perspective. Front Psychol 12:625117
Tondorf T, Grossert A, Rothschild SI et al (2018) Focusing on cancer patients’ intentions to use psychooncological support: a longitudinal, mixed-methods study. Psychooncology 27:1656–1663
Walker J, Hansen CH, Sawhney A et al (2013) Prevalence of depression in adults with cancer: a systematic review. Ann Oncol 24(4):895–900
Grassi L, Spiegel D, Riba M (2017) Advancing psychosocial care in cancer patients [version 1; peer review: 3 approved]. F1000Research 6(F1000 Faculty Rev):2083. https://doi.org/10.12688/f1000research.11902.1
The National Institute of Mental Health. Depression: signs and symptoms. The National Institute of Mental Health Website. Revised February, 2018. Accessed on December 7, 2020. https://www.nimh.nih.gov/health/topics/depression/index.shtml
Henry DH, Viswanathan HN, Elkin EP, Traina S, Wade S, Cella D (2008) Symptoms and treatment burden associated with cancer treatment: results from a cross-sectional national survey in the U.S. Support Cancer Care 16:791–801
Kissane DW, Maj M, Sartorius N (2011) Depression and cancer. John Wiley & Sons, West Sussex, UK
Lally BE, Geiger AM, Urbanic JJ et al (2009) Trends in the outcomes for patients with limited stage small cell lung cancer: an analysis of the surveillance, epidemiology, and end results database. Lung Cancer 64(2):226–231
Thun MJ, Hannan LM, Adams-Campbell LL et al (2008) Lung cancer occurrence in never-smokers: an analysis of 13 cohorts and 22 cancer registry studies. PLoS Med 5(9):e185
Radovic M, Kanesvaran R, Rittmeye A et al (2019) Multidisciplinary treatment of lung cancer in older patients: a review. J Geriatr Oncol 10(3):405–410
Samnaliev M, McGovern MP, Clark RE (2009) Racial/ethnic disparities in mental health treatment in six Medicaid programs. J Health Care Poor Underserved 20(1):165–176
Ellis J, Lin J, Walsh A, Lo C, Shepherd FA, Moore M et al (2009) Predictors of referral for specialized psychosocial oncology care in patients with metastatic cancer: the contributions of age, distress and marital status. J Clin Oncol 27:699–705
Giorgi A (2009) The descriptive phenomenological method in psychology: a modified Husserlian approach. PA. Duquesne University Press, Pittsburgh (ISBN 978-0-8207-0418-0)
Neuber BE, Witkop CB, Varpio L (2019) How phenomenology can help us learn from the experiences of others. Perspect Med Educ 8:90–97
Teherani A, Martimianakis T, Stenfors-Hayes T, Wadhwa A, Varpio L (2015) Choosing a qualitative research approach. J Grad Med Educ 7:669–670
Radloff LS (1977) The CES-D scale: A self report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Dominguez FJ, Lawrence C, Halpern EF, Drohan B, Grinstein G, Black DM, et al. (2007) Accuracy of self-reported personal history of cancer in an outpatient breast center. J Genet Couns. 16(3). https://doi.org/10.1007/s10897-006-9067-y
Martin LM, Leff M, Calonge N, Garrett C, Nelson DE (2000) Validation of self-reported chronic conditions and health services in a managed care population. AJPM 18(3):215–218
Kehoe R, Wu S, Leske MC, Chylack LT Jr (1994) Comparing self-reported and physician-reported medical history. Am J Epidemiol 139(8):813–818
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101
Sundler AJ, Lindberg E, Nilsson C, Palmer L (2019) Qualitative thematic analysis based on descriptive phenomenology. Nurs Open 6(3):733–739
Groenewald T (2004) A phenomenological research design illustrated. Int J Qual Methods 3(1):42–55
The American Cancer Society. Chemotherapy side effects. the American Cancer Society Website. Revised May 1, 2020. Accessed on April 10, 2021. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/chemotherapy-side-effects.html
Lindley C, McCune JS, Thomason TE et al (2001) Perception of chemotherapy side effects cancer versus noncancer patients. Cancer Pract 7(2):59–65
Ruhlmann CH, Iversen TZ, Okera M et al (2015) Multinational study exploring patients’ perceptions of side-effects induced by chemo-radiotherapy. Radiother Oncol 117(2):333–337
Granek L, Nakash O, Ben-David M, Shapira S, Ariad S (2018) Oncologists’ treatment responses to mental health distress in their cancer patients. Qual Health Res 28(11):1735–1745
Jean-Pierre P, Morrow GR, Roscoe JA et al (2010) A phase 3 randomized, placebo-controlled, double-blind, clinical trial of the effect of modafinil on cancer-related fatigue among 631 patients receiving chemotherapy: a University of Rochester Cancer Center Community Clinical Oncology Program Research base study. Cancer 116:3513–3520
Spathis A, Fife K, Blackhall F et al (2014) Modafinil for the treatment of fatigue in lung cancer: results of a placebo-controlled, double-blind, randomized trial. J Clin Oncol 32:1882–1888
Moraska AR, Sood A, Dakhil SR et al (2010) Phase III, randomized, double-blind, placebo-controlled study of long-acting methylphenidate for cancer-related fatigue: North Central Cancer Treatment Group NCCTG-N05C7 trial. J Clin Oncol 28:3673–3679
Pattyn E, Verhaeghe M, Sercu C, Bracke P (2014) Public stigma and self-stigma: differential association with attitudes toward formal and informal help seeking. Psychiatr Serv 65(2):232–238
Matthews AK, Corrigan PW, Rutherford JL (2003) Mental illness stigma as a barrier to psychosocial services for cancer patients. JNCCN 1(3). https://doi.org/10.6004/jnccn.2003.0032
Sannes TS, Pirl W, Rossi JS, et al. (2020) Identifying patient-level factors associated with interest in psychosocial services during cancer: a brief report. J Psychosoc Oncol 1–8. https://doi.org/10.1080/07347332.2020.1837329
Blank TO, Bellizzi KM (2008) A gerontologic perspective on cancer and aging. Cancer 112(11 Suppl):2569–2576
Kartins Klein B, Bamonti PM, Owsiany M, Maik A, Moye J (2021) Age differences in cancer-related stress, spontaneous emotion regulation, and emotional distress. Aging Ment Health 25(2):250–259
Robb C, Haley WE, Becker MA, Polivka LA, Chwa HJ (2003) Attitudes towards mental health care in younger and older adults: similarities and differences. Aging Ment Health 7(2):142–152
Mosher CE, Hanna N, Jalal SI et al (2013) Support service use and interest in support services among lung cancer patients. Lung Cancer 82(1):162–167
Acknowledgements
We are grateful for research support from Dr. Laura Hayman, PhD, RN, FAAN, FAHA, University of Massachusetts Boston, and the Patient Perceptions Project research participants.
Funding
This study was funded by grant U54-CA156732 to Drs. Park, Cannon, and Traeger from the National Institutes of Health/National Cancer Institute (NIH/NCI).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Emily Friedman, Elyse Park, Shelia Cannon, and Lara Traeger. The first draft of the manuscript was written by Sarah Skurla, Emily Friedman, and Lara Traeger and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Partners Human Research Committee, protocol # 2011-P-000815.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Skurla, S.E., Friedman, E.R., Park, E.R. et al. Perceptions of somatic and affective symptoms and psychosocial care utilization in younger and older survivors of lung cancer. Support Care Cancer 30, 5311–5318 (2022). https://doi.org/10.1007/s00520-022-06926-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06926-6