Abstract
Although cognitive impairment is well-documented in children with moyamoya disease (MMD), selective decline in specific neurocognitive domains remains controversial. The purpose of this study was to characterize the neurocognitive profile of children with MMD using the Das Naglieri Cognitive Assessment System (CAS) and the Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV). We analyzed the neurocognitive data of 30 children (median age, 7 years) with MMD who were assessed with the CAS and the WISC-IV before surgery. We focused on the comparison of standard scores and intraindividual differences across domains. The CAS scores significantly varied across four measures (standard scores, p < 0.001; intraindividual differences, p < 0.001). Post-hoc analyses revealed that the standard scores and intraindividual differences for successive processing were significantly lower than those for planning and attention. The WISC-IV scores did not significantly vary among the four measures, although the working memory index was the lowest among the four measures. The within-individual weakness in successive processing, a form of working memory function, may be a distinct characteristic of children with MMD. The CAS may be more sensitive than the WISC-IV for detecting this selective neurocognitive weakness in children with MMD.
Similar content being viewed by others
Introduction
Moyamoya disease (MMD) is a rare steno-occlusive cerebrovascular disease that involves the terminal portion of the bilateral internal carotid arteries. The age of onset of MMD has a bimodal peak: a major peak in the first decade of life and a moderate peak in the late 20s to 30s1.
Children with MMD commonly manifest ischemic symptoms, such as transient ischemic attacks (TIA) and stroke. However, children with MMD can also suffer from cognitive impairment. According to a recent systematic review, the prevalence of cognitive impairment is 30% (range 13% to 67%), and median intelligence quotient (IQ) is 98 (range 71 to 107)2. Long-term follow up studies have revealed that 10% to 20% of children with MMD have difficulty with social adaptation after adolescence because of cognitive impairment3,4,5,6,7. Such neurocognitive impairment is attributable to hypoperfusion in the vascular territories, which include the anterior and middle cerebral artery territories1,8 and the frontal lobe in particular9,10,11,12,13,14,15. Several multicentered registration studies, such as the Cognitive Dysfunction Survey of the Japanese Moyamoya Disease study16, are ongoing and aim to reveal neurocognitive and neuroradiological characteristics of moyamoya disease.
Although the mechanisms underlying neurocognitive impairment in moyamoya disease suggest selective impairment of specific neurocognitive domains that correspond to the vascular territories, the evidence remains controversial2,17. One possible reason is that the neuropsychological tests that are applicable to children are limited (e.g., the Wechsler Intelligence Scale for Children [WISC], the Das Naglieri Cognitive Assessment System [CAS], and the Kaufman Assessment Battery for Children). To date, there have been no studies conducted in children with MMD that have applied various neuropsychological tests on a large, representative, and standardized sample. Another possible reason for the controversy is that the interpretations of most available neuropsychological tests are based on comparisons with the normal population, which may underestimate the variability of neurocognitive domains within an individual.
The CAS is a standardized neuropsychological test developed by Das and Naglieri that focuses on the assessment of cognitive function, rather than intelligence, in children aged 5 to 17 years18. The official Japanese version of the CAS was developed in 200719. The CAS comprises four measures: planning, attention, simultaneous processing, and successive processing. It is unique in that it assesses “intraindividual differences,” which are statistical fluctuations (strengths and weaknesses) across measures within an individual20. For this reason, we routinely use CAS as a preoperative neuropsychological test, in addition to the WISC.
The WISC is the most commonly used neuropsychological test worldwide that measures the intellectual ability of children aged 5 to 16 years21. The official Japanese version of the WISC fourth edition (WISC-IV) was developed in 201022. The WISC-IV comprises four indices: verbal comprehension, perceptual reasoning, processing speed, and working memory. The WISC-IV implements a clinical method known as “the discrepancy analysis,” which aims to detect significant discrepancies among indexes in each individual. Kazumata et al. reported that discrepancies were most frequently observed between the verbal comprehension index and working memory index of the WISC-IV23. However, the discrepancy analysis of the WISC-IV is not necessarily suitable as a research method for detecting cognitive variability within a specific population. This is because, although discrepancy analysis of the WISC-IV only detects differences between each index, the CAS allows analyses of whether an index deviates from the average value of the entire individual. Therefore, the method whereby intraindividual differences are detected is limited in the WISC-IV.
To date, there have been no studies that have examined the neurocognitive function of children with MMD using both the CAS and the WISC. Determining whether specific neurocognitive weaknesses exist in children with MMD would be valuable for clinicians and rehabilitation professionals who support children with MMD.
The purpose of this study was to characterize the neurocognitive profile of children with MMD before surgery using the CAS and WISC-IV. We compared the scores of these neuropsychological tests and analyzed the intraindividual differences derived from these tests.
Methods
This cross-sectional study was approved by the ethics committee of Kyoto University Graduate School, Faculty of Medicine (R1417). Study procedures were carried out in accordance with the Declaration of Helsinki. For prospective data, informed assent was obtained from all individual participants and written informed consent was obtained from their parents. For retrospective data, all subjects gave opt-out consent.
Patients
The inclusion criteria were children aged 5 to 16 years who had been newly diagnosed with MMD and had undergone neuropsychological testing before surgery. Patients were diagnosed according to the criteria proposed by the Research Committee on Moyamoya Disease in Japan1. All moyamoya children aged 5 to 16 years and their parents were asked at their first visit whether they were willing to undergo neuropsychological tests.
A total of 40 children aged 5 to 16 years were admitted to Kyoto University Hospital between June 2016 and June 2020 and diagnosed with MMD. Of the 40 patients, 10 were excluded from the analyses for the following reasons: the patients and family declined the neuropsychological tests (2 patients); preoperative neuropsychological tests were not completed because of unstable symptoms (2 patients), limited examination schedule (1 patient); deafness (1 patient); lack of Japanese ability (1 patient); judgment by the psychiatrist that the neuropsychological test results were biased because of the patient’s developmental background (2 patients); and special education for gifted children (1 patient). This resulted in a total of 30 children for the analysis.
Clinical data were collected, which included sex, initial manifestations (e.g. TIA, stroke, intracranial hemorrhage, and headache), age at symptom onset and first admission, time interval between onset and first admission, Suzuki’s angiographical stage24, hemodynamic state assessed using single photon emission computed tomography (SPECT)25, laterality of disease involvement, presence or absence of posterior cerebral artery (PCA) involvement, and asymptomatic infarction on magnetic resonance imaging (MRI). PCA involvement was defined as stenosis greater than 50% in the P1 to P3 segment of either PCA, with decreased delineation of cortical arteries in either hemisphere6. The hemodynamic state for each hemisphere was graded according to SPECT findings into one of the following three stages: stage 0, normal baseline cerebral blood flow (CBF) with normal acetazolamide-challenged CBF; stage 1, normal baseline CBF with reduced acetazolamide-challenged CBF; and stage 2, reduced baseline CBF with reduced acetazolamide-challenged CBF25. Acetazolamide-challenged SPECT was not indicated for patients with severely reduced CBF in at least one hemisphere because of the risk of ischemic complication. Because this resulted in unclear differentiation between stages 0 and 1 in several hemispheres, we recorded hemodynamic state as either stage 2 or non-stage 2.
Neurocognitive evaluation
The CAS and the WISC-IV were performed as preoperative neurocognitive assessments. All but one participant underwent both tests during the first admission. Occupational therapists, who are proficient in neurocognitive testing, conducted all tests in a consistent manner. Table 1 shows the comparison of characteristics between the CAS and WISC-IV.
The CAS provides standard scores for each of the four scales of planning, attention, simultaneous processing, and successive processing (PASS) as well as a full scale score18. The standard scores are defined by a mean of 100 with a standard deviation of 15. Each PASS scale comprises three tasks, with the whole battery comprising 12 tasks. The intraindividual difference is calculated by subtracting the average of the four PASS standard scores from each PASS standard score20. The intraindividual difference is negative if an individual scores relatively low in one PASS scale compared with the other scales. To interpret the CAS, a significant level of intraindividual difference was defined for each measure based on a standardized sample19. According to the manual of the CAS and WISC-IV, we defined a significant intraindividual difference as − 11 points or lower.
The WISC-IV provides standard scores for the following measures: full scale IQ, verbal comprehension index (VCI), perceptual reasoning index (PRI), working memory index (WMI), and processing speed index (PSI)21. These standard scores are defined by a mean of 100 with a standard deviation of 15 and are based on a large and representative standardized sample. Unlike the CAS, the calculation of the intraindividual difference is not specified in the WISC-IV. However, we used the same method as the CAS for calculating intraindividual differences based on the WISC-IV for the purpose of performing analyses within each participant.
Statistical analysis
Wilcoxon rank-sum test was used for comparison between groups with and without asymptomatic infarction for mean full scale CAS and WISC-IV scores.
Descriptive statistics of the CAS and the WISC-IV are presented as mean and standard deviation for both the standard scores and intraindividual differences. Normality of the data was evaluated using the Shapiro–Wilk test. To compare the standard scores across the four measures of the CAS and the WISC-IV within each individual, we used a one-factor repeated measures analysis of variance (ANOVA). To compare intraindividual differences across the four measures, we used a one-way ANOVA because it was calculated based on the average of the four measures and thus, a repeated analysis was not necessary. Post-hoc tests were performed using Tukey’s honestly significant difference (HSD) test.
All statistical analyses were performed using JMP 14 (SAS Institute Inc., Cary, NC, USA). All tests were two-sided, and p < 0.05 was considered to indicate statistical significance.
Results
Clinical characteristics
Table 2 shows the clinical characteristics of the 30 included and 10 excluded patients. For the included patients, the median age of first admission was 7 years (interquartile range, 5.75 to 10 years) and the median time interval between symptom onset and admission was 6 months (interquartile range, 1 to 19.5 months). Females accounted for 70% of the included patients. The most common initial manifestation was TIA, which accounted for 73.3% of the included patients. One patient with stroke exhibited cortical laminar necrosis in the left primary motor cortex, which was confirmed by MRI, and mild paralysis of the right lower extremity, from which the patient made a full recovery. Three patients exhibited MRI findings of past intraventricular hemorrhage with no apparent intraparenchymal damage. Although hemorrhagic stroke caused consciousness disturbance during the acute phase, all three patients recovered without any neurological deficit before undergoing neuropsychological tests. Eleven patients (36.7%) had stage 2 hemodynamic failure in the right hemisphere, and 10 patients (33.3%) had stage 2 hemodynamic failure in the left hemisphere. Sixteen patients (53.3%) had stage 2 hemodynamic failure in at least one hemisphere. Asymptomatic infarction was observed in 11 patients (36.7%), which included the three patients mentioned above who exhibited hemorrhagic presentation.
Neurocognitive findings
Mean full scale scores of CAS and WISC-IV were not statistically different between patients with and without asymptomatic infarction (CAS, p = 0.904; WISC-IV, p = 0.749).
Table 3 shows the descriptive statistics for each measure of the CAS and WISC-IV. All standard scores and intraindividual differences were normally distributed according to the Shapiro–Wilk test. The mean full scale scores of both the CAS and WISC-IV were within the normal range (102.2 ± 13.7 and 107.1 ± 14.4, respectively). The mean standard scores of the four separate measures in the CAS and the WISC-IV were also within the normal range, based on the standardized sample, except for planning (112.0 ± 13.3). In the CAS, scores for successive processing were the lowest among the four measures in terms of both standard scores and intraindividual differences (98.5 ± 14.1 and − 6.9 ± 8.7, respectively). In the WISC-IV, the WMI was the lowest among the four measures in terms of both standard scores and intraindividual differences (99.6 ± 13.7 and − 1.7 ± 8.7, respectively).
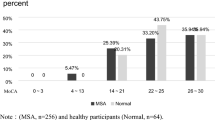
There was a statistically significant variance across all four measures of the CAS for standard scores and intraindividual differences, as shown in Table 3 and Fig. 1. The one-factor repeated measures ANOVA revealed a significant difference in the standard scores of the CAS (F (3,87) = 9.206, p < 0.001), but not in that of the WISC-IV (F (3,87) = 0.621, p = 0.603). The one-way ANOVA also revealed a significant difference in the intraindividual differences of the CAS (F (3,116) = 12.275, p < 0.001), but not in that of the WISC-IV (F (3,116) = 0.828, p = 0.481).
Graphs showing the neurocognitive data of each participant. (A) Standard score of the WISC-IV. (B) Standard score of the CAS. (C) Intraindividual difference in the WISC-IV. (D) Intraindividual difference in the CAS. The red dot indicates the mean value, and the error bar indicates the standard deviation. CAS cognitive assessment system, PRI perceptual reasoning index, PSI processing speed index, VCI verbal comprehension index, WISC Wechsler intelligence scale for children, WMI working memory index.
Table 4 shows the post-hoc multiple comparison of the CAS scores. Tukey’s HSD test applied to the CAS scores revealed that both the standard score and intraindividual difference of successive processing were significantly lower than those of planning (standard score, p = 0.002; intraindividual difference, p < 0.001) and attention (standard score, p = 0.047; intraindividual difference, p < 0.001). The intraindividual difference of simultaneous processing was significantly lower than that of planning (p = 0.002).
The mean value of the intraindividual difference in successive processing was lower in those with SPECT stage 2 than in those with non-stage 2 (− 7.6 ± 8.6 vs − 6.3 ± 8.9), although the difference was not significant.
The proportions of patients who exhibited significant intraindividual differences in each measure of the CAS and WISC-IV were as follows: planning (0/30 or 0%), attention (3/30 or 10%), simultaneous processing (4/30 or 13.3%), and successive processing (11/30 or 36.7%) for the CAS; and VCI (3/30 or 10%), PRI (5/30 or 16.7%), PSI (4/30 or 13.3%), and WMI (6/30 or 20%) for the WISC-IV.
Discussion
Our study had three main findings. First, children with MMD exhibited selective within-individual weaknesses in successive processing as measured by the CAS. Second, intelligence measured with the WISC-IV was within the normal range with or without infarction. Third, no significant variability across the intellectual domains of the WISC-IV was observed, although the score for the working memory index was the lowest. The first finding is novel because CAS has not been applied to children with MMD, except for in a pioneering case report written in Japanese26. Furthermore, we used both the CAS and WISC to assess children with MMD and showed that the CAS detected selective neurocognitive weaknesses that were not detected by the WISC-IV.
Successive processing in the CAS is thought to be similar in concept to the WMI in the WISC-IV as both involve the auditory recall of a sequence. The successive processing scale of the CAS comprises three tasks: immediate recall of a series of words (e.g. cat-flower-book); repetition of sentences with no actual meaning (e.g. white is blue); and sentence questions as syntactic comprehension (e.g. the blue yellows the green, and who yellows the green?). The WMI in the WISC-IV comprises digit span and letter-number sequencing, whereas successive processing in the CAS involves language recall. Das et al., one of the groups that developed the CAS, has explained that successive processing involves the articulatory loop of working memory, as proposed by Baddeley27. Furthermore, a validation study on the Japanese version of the WISC-IV also revealed a high correlation between the successive processing scale of the CAS and the WMI of the WISC-IV22. Therefore, it is reasonable to suggest that successive processing reflects a form of verbal working memory function. Further studies are required to determine which components of working memory are associated with neurocognitive weaknesses in children with MMD.
Interestingly, our result of selective weakness in successive processing corresponds to those of a previous study. Hsu et al. reported that selective impairment in immediate word recall, as measured by the Word List Test in the Wechsler Memory Scale, might be a characteristic of MMD children with younger onset and prolonged symptom duration17. The successive processing scale of the CAS, which requires the working memory of language, might better reflect the cognitive skills required in daily life and the difficulties experienced by patients, such as inability to follow schoolwork, trying to learn too many things simultaneously, and poor attention. Our results also suggest that such difficulties could occur even if overall intelligence, as defined by the full scale scores, is high. Alternatively, the WMI of the WISC-IV, which comprises only digit span, may simply be impractical and unsuitable for detecting neurocognitive characteristics in children with MMD.
Kazumata et al. have suggested that verbal function is relatively preserved in MMD children23, which is inconsistent with our results. However, one reason for why the verbal working memory tasks of the CAS were more affected than the digit span task of the WISC in our study is that the former task is more complex and difficult because it requires not only basic working memory ability but also semantic processing ability. Therefore, our results are not inconsistent with the suggestion of Kazumata et al. In addition, logically, whether verbal function or non-verbal function is more impaired is defined by the laterality of disease involvement and may be less related to working memory function per se. Although the relatively complex working memory tasks of the CAS seem suitable for MMD children, the optimal working memory task for detecting working memory weaknesses specific to children with MMD remain to be ascertained. This issue should be addressed in future studies.
Selective impairment of neurocognitive domains has been attributed to hypoperfusion in specific vascular territories that are predominantly affected in MMD. Arterial stenosis in MMD involves the internal carotid artery by definition and thus causes ischemia of the frontal lobe28. Numerous studies have demonstrated a close relationship between the dorsolateral prefrontal cortex and executive functions, including working memory29,30. Moreover, Lezak et al. described that the prefrontal lobe is involved in short-term memory31. Therefore, our finding of verbal working memory disturbance in MMD is consistent with brain dysfunctions typically reported in MMD patients. However, further studies on cerebral perfusion imaging are required to clarify the relationship between working memory and previously reported cerebral blood flow changes in children with MMD10,23.
The fact that the scores of the WISC-IV fell within the normal range in our patients is consistent with previous studies that showed average to above average overall intelligence in children with MMD17,32,33,34,35 These results may be interpreted as an underestimation of within-individual variability in assessments using the WISC, given that variability is not measured by this scale. To address this question, we applied the method used for calculating intraindividual differences in the CAS to the WISC-IV and found no significant variability among the four measures, although the WMI score was the lowest. These findings suggest that the WISC-IV is less able to detect characteristics of neurocognitive deficits in children with MMD.
The present study has several limitations. First, our study population was relatively small. Although our study is one of the given the rarity of the disease, larger studies are needed. Nevertheless, our study design of using two standardized tests that are rarely applied to children demonstrates some validity of our results on neurocognitive profiles. Second, our study had the potential to have been contaminated by selection bias because we only included preoperative patients. The exclusion of children under 5 years of age, for whom neuropsychological testing is inapplicable, or those who required acute surgery because of unstable symptoms may overestimate our results and limit their generalizability. Finally, this study did not include a control group.
Conclusions
Our assessment of the CAS suggests that a selective within-individual weakness in successive processing, a type of working memory, may be a characteristic of children with MMD. The CAS was more sensitive in detecting this selective neurocognitive weakness than the WISC-IV in children with MMD. Further studies are required to determine whether the CAS has value for clinical use in supporting the education and daily life of children with MMD.
References
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Intractable Diseases. Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol. Medico-chir. 52, 245–266 (2012).
Kronenburg, A. et al. Cognitive functions in children and adults with moyamoya vasculopathy: A systematic review and meta-analysis. J. Stroke 20, 332–341 (2018).
Nakashima, H., Meguro, T., Kawada, S., Hirotsune, N. & Ohmoto, T. Long-term results of surgically treated moyamoya disease. Clin. Neurol. Neurosurg. 99, 156–161 (1997).
Miyamoto, S. et al. Long-term outcome after STA-MCA anastomosis for moyamoya disease. Neurosurg. Focus 5, 5 (1998).
Phi, J. H. et al. Long-term social outcome in children with moyamoya disease who have reached adulthood. J. Neurosurg. Pediatr. 8, 303–309 (2011).
Funaki, T. et al. Impact of posterior cerebral artery involvement on long-term clinical and social outcome of pediatric moyamoya disease. J. Neurosurg. Pediatr. 12, 626–632 (2013).
Funaki, T., Takahashi, J. C. & Miyamoto, S. Late cerebrovascular events and social outcome after adolescence: Long-term outcome of pediatric moyamoya disease. Neurol. Med. Chir. (Tokyo) 58, 240–246 (2018).
Scott, R. M. & Smith, E. R. Moyamoya disease and moyamoya syndrome. N. Engl. J. Med. 360, 1226–1237 (2009).
Karasawa, J., Touho, H., Ohnishi, H., Miyamoto, S. & Kikuchi, H. Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease. J. Neurosurg. 77, 84–89 (1992).
Ohtaki, M. et al. Intellectual functions and regional cerebral haemodynamics after extensive omental transplantation spread over both frontal lobes in childhood moyamoya disease. Acta Neurochir. 140, 1043–1053 (1998).
Calviere, L. et al. Correlation between cognitive impairment and cerebral hemodynamic disturbances on perfusion magnetic resonance imaging in European adults with moyamoya disease: Clinical article. J. Neurosurg. 113, 753–759 (2010).
Sato, H., Sato, N., Tamaki, N. & Matsumoto, S. Chronic low-perfusion state in children with moyamoya disease following revascularization. Child’s Nerv. Syst. 6, 166–171 (1990).
Nakagawara, J. et al. Diagnostic imaging of higher brain dysfunction in patients with adult moyamoya disease using statistical imaging analysis for [123]iomazenil single photon emission computed tomography. Neurol. Medico-chir. 52, 318–326 (2012).
Kuroda, S., Houkin, K., Kamiyama, H., Abe, H. & Mitsumori, K. Regional cerebral hemodynamics in childhood moyamoya disease. Child’s Nerv. Syst. 11, 584–590 (1995).
Araki, Y. et al. Cognitive function of patients with adult moyamoya disease. J. Stroke Cerebrovasc. Dis. 23, 1789–1794 (2014).
Takagi, Y. et al. Cognitive dysfunction survey of the Japanese patients with moyamoya disease (cosmo-japan study): Study protocol. Neurol. Medico-chir. 55, 199–203 (2015).
Hsu, Y. H., Kuo, M. F., Hua, M. S. & Yang, C. C. Selective neuropsychological impairments and related clinical factors in children with moyamoya disease of the transient ischemic attack type. Child’s Nerv. Syst. 30, 441–447 (2014).
Naglieri, J. & Das, J. Cognitive Assessment System Interpretive Handbook. 1–11. (The Riverside Publishing, 1997).
Naglieri, J. & Das, J. Cognitive Assessment System Interpretive Handbook. 33–79. (Nihon Bunka Kagakusha, 2007).
Naglieri, J. Essentials of CAS Assessment. 69–81. (Wiley, 1999).
Wechsler, D. Technical and Interpretive Manual for the Wechsler Intelligence Scale for Children-Fourth Edition. 7–16. (Harcourt Assessment Inc, 2003).
Wechsler, D. Technical and Interpretive Manual for the Wechsler Intelligence Scale for Children-Fourth Edition. 45–97. (Nihon Bunka Kagakusha, 2010).
Kazumata, K. et al. Association of cognitive function with cerebral blood flow in children with moyamoya disease. J. Neurosurg. Pediatr. 25, 62–68 (2020).
Suzuki, J. & Kodama, N. Moyamoya disease–A review. Stroke 14, 104–109 (1983).
Takahashi, J. C. et al. Impact of cortical hemodynamic failure on both subsequent hemorrhagic stroke and effect of bypass surgery in hemorrhagic moyamoya disease: A supplementary analysis of the Japan Adult Moyamoya Trial. J. Neurosurg. 134, 940–945 (2021).
Aihara, Y. et al. Clinical features of magnetic resonance imaging and angiography image findings and cognitive dysfunction in pediatric moyamoya disease: Psychological evaluation based on cognitive function examination. Nerv. Syst. Child. 42, 355–363 (2017).
Das, J., Naglieri, J. & Kirby, J. Assessment of Cognitive Processes the PASS Theory of Intelligence. 52–74. (Allyn & Bacon, 1994).
Kuroda, S. & Houkin, K. Moyamoya disease: Current concepts and future perspectives. Lancet Neurol. 7, 1056–1066 (2008).
Goldman-Rakic, P. The prefrontal landscape: implications of functional architecture for understanding human mentation and the central executive. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 351, 1445–1453 (1996).
Baddeley, A. D. & Hitch, G. J. Developments in the concept of working memory. Neuropsychology 8, 485–493 (1994).
Lezak, M. Neuropsychological Assessment 3rd edn. (Oxford University Press, 1995).
Ishii, R., Takeuchi, S., Ibayashi, K. & Tanaka, R. Intelligence in children with moyamoya disease: Evaluation after surgical treatments with special reference to changes in cerebral blood flow. Stroke 15, 873–877 (1984).
Matsushima, Y., Aoyagi, M., Nariai, T., Takada, Y. & Hirakawa, K. Long-term intelligence outcome of post-encephalo-duro-arterio-synangiosis childhood moyamoya patients. Clin. Neurol. Neurosurg. 99, 147–150 (1997).
Lee, J. Y. et al. Neurocognitive profiles of children with moyamoya disease before and after surgical intervention. Cerebrovasc. Dis. 31, 230–237 (2010).
Kim, W. et al. Neuropsychological impacts of indirect revascularization for pediatric moyamoya disease. Childs. Nerv. Syst. 34, 1199–1206 (2018).
Acknowledgements
We appreciate the guidance of Dr. Kazumichi Yoshida, Dr. Ryosuke Ikeguchi, Manabu Nankaku, and Rie Yamawaki. We thank Sarina Iwabuchi, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection, analysis or interpretation were performed by all authors. The first draft of the manuscript was written by Y.K., T.F. and K.U., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kusano, Y., Funaki, T., Ueda, K. et al. Characterizing the neurocognitive profiles of children with moyamoya disease using the Das Naglieri cognitive assessment system. Sci Rep 12, 3638 (2022). https://doi.org/10.1038/s41598-022-07699-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07699-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.