Abstract
Background
Disparities based on socioeconomic factors such as race, ethnicity, marital status, and insurance status are associated with pancreatic cancer resection, but these disparities are usually not observed for survival after resection. It is unknown if there are disparities when patients undergo their treatment in a non-fee-for-service, equal-access healthcare system such as the Veterans Health Administration (VHA).
Methods
Patients having T1–T3 M0 pancreatic adenocarcinoma diagnosed between 2006 and 2017 were identified from the VHA Corporate Data Warehouse. Socioeconomic, demographic, and tumor variables associated with resection and survival were assessed.
Results
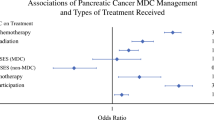
In total, 2580 patients with early-stage pancreatic cancer were identified. The resection rate was 36.5%. Surgical resection was independently associated with younger age [odds ratio (OR) 0.94, p < 0.001], White race (OR 1.35, p = 0.028), married status (OR 1.85, p = 0.001), and employment status (retired vs. unemployed, OR 1.41, p = 0.008). There were no independent associations with Hispanic ethnicity, geographic region, or Social Deprivation Index. Resection was associated with significantly improved survival (median 21 vs. 8 months, p = 0.001). Among resected patients, survival was independently associated with younger age (HR 1.019, p = 0.002), geographic region (South vs. Pacific West, HR 0.721, p = 0.005), and employment (employed vs. unemployed, HR 0.752, p = 0.029). Race, Hispanic ethnicity, marital status, and Social Deprivation Index were not independently associated with survival after resection.
Conclusions
Race, marital status, and employment status are independently associated with resection of pancreatic cancer in the VHA, whereas geographic region and employment status are independently associated with survival after resection. Further studies are warranted to determine the basis for these inequities.

Similar content being viewed by others
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913–21.
Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS. National failure to operate on early stage pancreatic cancer. Ann Surg. 2007;246(2):173–80.
McGhan LJ, Etzioni DA, Gray RJ, Pockaj BA, Coan KE, Wasif N. Underuse of curative surgery for early stage upper gastrointestinal cancers in the United States. J Surg Res. 2012;177(1):55–62.
Shaib Y, Davila J, Naumann C, El-Serag H. The impact of curative intent surgery on the survival of pancreatic cancer patients: a U.S. population-based study. Am J Gastroenterol. 2007;102(7):1377–82.
Shapiro M, Chen Q, Huang Q, et al. Associations of socioeconomic variables with resection, stage, and survival in patients with early-stage pancreatic cancer. JAMA Surg. 2016;151(4):338–45.
Bilimoria KY, Bentrem DJ, Tomlinson JS, et al. Quality of pancreatic cancer care at Veterans Administration compared with non-Veterans Administration hospitals. Am J Surg. 2007;194(5):588–93.
Khawja SN, Mohammed S, Silberfein EJ, Musher BL, Fisher WE, Van Buren G. Pancreatic cancer disparities in African Americans. Pancreas. 2015;44(4):522–7.
Cervantes A, Waymouth EK, Petrov MS. African-Americans and Indigenous Peoples have increased burden of diseases of the exocrine pancreas: a systematic review and meta-analysis. Dig Dis Sci. 2019;64(1):249–61.
Blanco BA, Poulson M, Kenzik KM, McAneny DB, Tseng JF, Sachs TE. The impact of residential segregation on pancreatic cancer diagnosis, treatment, and mortality. Ann Surg Oncol. 2020;28:3147.
Noel M, Fiscella K. Disparities in pancreatic cancer treatment and outcomes. Health Equity. 2019;3(1):532–40.
Shah A, Chao KS, Ostbye T, et al. Trends in racial disparities in pancreatic cancer surgery. J Gastrointest Surg. 2013;17(11):1897–906.
Molina G, Clancy TE, Tsai TC, Lam M, Wang J. Racial disparity in pancreatoduodenectomy for borderline resectable pancreatic adenocarcinoma. Ann Surg Oncol. 2021;28(2):1088–96.
Murphy MM, Simons JP, Ng SC, et al. Racial differences in cancer specialist consultation, treatment, and outcomes for locoregional pancreatic adenocarcinoma. Ann Surg Oncol. 2009;16(11):2968–77.
Heller DR, Nicolson NG, Ahuja N, Khan S, Kunstman JW. Association of treatment inequity and ancestry with pancreatic ductal adenocarcinoma survival. JAMA Surg. 2020;155(2):e195047.
Riall TS, Townsend CM Jr, Kuo YF, Freeman JL, Goodwin JS. Dissecting racial disparities in the treatment of patients with locoregional pancreatic cancer: a 2-step process. Cancer. 2010;116(4):930–9.
Singal V, Singal AK, Kuo YF. Racial disparities in treatment for pancreatic cancer and impact on survival: a population-based analysis. J Cancer Res Clin Oncol. 2012;138(4):715–22.
Zhu F, Wang H, Ashamalla H. Racial and socioeconomic disparities in the treatments and outcomes of pancreatic cancer among different treatment facility types. Pancreas. 2020;49(10):1355–63.
Liu JH, Zingmond DS, McGory ML, SooHoo NF, Ettner SL, Brook RH, Ko CY. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA. 2006;296(293):1973–80.
Shavers VL, Harlan LC, Jackson M, Robinson J. Racial/ethnic patterns of care for pancreatic cancer. J Palliat Med. 2009;12(7):623–30.
Deville C Jr, Lee WR. Reconciling outcomes for Black men with prostate cancer within and outside the Veterans Health Administration. Cancer. 2021;127(3):342–4.
Peterson K, Anderson J, Boundy E, Ferguson L, McCleery E, Waldrip K. Mortality disparities in racial/ethnic minority groups in the Veterans Health Administration: an evidence review and map. Am J Public Health. 2018;108(3):e1–11.
Graham-Steed T, Uchio E, Wells CK, Aslan M, Ko J, Concato J. “Race” and prostate cancer mortality in equal-access healthcare systems. Am J Med. 2013;126(12):1084–8.
Riviere P, Luterstein E, Kumar A, et al. Survival of African American and non-Hispanic white men with prostate cancer in an equal-access health care system. Cancer. 2020;126(8):1683–90.
Zullig LL, Carpenter WR, Provenzale D, Weinberger M, Reeve BB, Jackson GL. Examining potential colorectal cancer care disparities in the Veterans Affairs health care system. J Clin Oncol. 2013;31(28):3579–84.
Zullig LL, Jackson GL, Weinberger M, Provenzale D, Reeve BB, Carpenter WR. An examination of racial differences in process and outcome of colorectal cancer care quality among users of the veterans affairs health care system. Clin Colorectal Cancer. 2013;12(4):255–60.
Voora RS, Kotha NV, Kumar A, et al. Association of race and health care system with disease stage and survival in veterans with larynx cancer. Cancer. 2021;127:2705.
Ganti AK, Subbiah SP, Kessinger A, Gonsalves WI, Silberstein PT, Loberiza FR Jr. Association between race and survival of patients with non-small-cell lung cancer in the United States veterans affairs population. Clin Lung Cancer. 2014;15(2):152–8.
Fillmore NR, Yellapragada SV, Ifeorah C, et al. With equal access, African American patients have superior survival compared to white patients with multiple myeloma: a VA study. Blood. 2019;133(24):2615–8.
McKay RR, Sarkar RR, Kumar A, et al. Outcomes of Black men with prostate cancer treated with radiation therapy in the Veterans Health Administration. Cancer. 2021;127(3):403–11.
Williams CD, Salama JK, Moghanaki D, Karas TZ, Kelley MJ. Impact of race on treatment and survival among U.S. veterans with early-stage lung cancer. J Thorac Oncol. 2016;11(10):1672–81.
Earles A, Liu L, Bustamante R, et al. Structured approach for evaluating strategies for cancer ascertainment using large-scale electronic health record data. JCO Clin Cancer Inform. 2018;2:1–12.
U.S. Department of Commerce Economics and Statistics Administration U.S. Census Bureau. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf.
U.S. Census Bureau’s American Community Survey (ACS). https://www.census.gov/programs-surveys/acs/.
Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2 Pt 1):539–59.
Robert Graham Center-Social Deprivation Index https://www.graham-center.org/rgc/maps-data-tools/sdi/social-deprivation-index.html.
Samuel CA, Landrum MB, McNeil BJ, Bozeman SR, Williams CD, Keating NL. Racial disparities in cancer care in the Veterans Affairs health care system and the role of site of care. Am J Public Health. 2014;104(Suppl 4):S562-571.
Wong MS, Hoggatt KJ, Steers WN, et al. Racial/ethnic disparities in mortality across the Veterans Health Administration. Health Equity. 2019;3(1):99–108.
Williams CD, Alpert N, Redding TS, et al. Racial differences in treatment and survival among veterans and non-veterans with stage I NSCLC: an evaluation of Veterans Affairs and SEER-Medicare populations. Cancer Epidemiol Biomarkers Prev. 2020;29(1):112–8.
Lee S, Reha JL, Tzeng CW, et al. Race does not impact pancreatic cancer treatment and survival in an equal access federal health care system. Ann Surg Oncol. 2013;20(13):4073–9.
Aizer AA, Chen MH, McCarthy EP, et al. Marital status and survival in patients with cancer. J Clin Oncol. 2013;31(31):3869–76.
Baine M, Sahak F, Lin C, Chakraborty S, Lyden E, Batra SK. Marital status and survival in pancreatic cancer patients: a SEER based analysis. PLoS ONE. 2011;6(6):e21052.
Swords DS, Mulvihill SJ, Brooke BS, Firpo MA, Scaife CL. Size and importance of socioeconomic status-based disparities in use of surgery in nonadvanced stage gastrointestinal cancers. Ann Surg Oncol. 2020;27(2):333–41.
Murphy MM, Simons JP, Hill JS, et al. Pancreatic resection: a key component to reducing racial disparities in pancreatic adenocarcinoma. Cancer. 2009;115(17):3979–90.
Zell JA, Rhee JM, Ziogas A, Lipkin SM, Anton-Culver H. Race, socioeconomic status, treatment, and survival time among pancreatic cancer cases in California. Cancer Epidemiol Biomarkers Prev. 2007;16(3):546–52.
Acknowledgment
This research was supported by VA MERIT Review Award I01-BX003771-02 (J.S.G.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Del Valle, J.P., Fillmore, N.R., Molina, G. et al. Socioeconomic Disparities in Pancreas Cancer Resection and Survival in the Veterans Health Administration. Ann Surg Oncol 29, 3194–3202 (2022). https://doi.org/10.1245/s10434-021-11250-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11250-0