Abstract
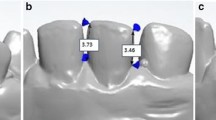
The purpose of this clinical study was to compare the effects of the gingival displacement techniques of retraction cord, cordless paste system, and Er,Cr:YSGG laser troughing on the periodontal tissues around the crown restoration produced using a digital scan. This was analyzed by recording the probing depth (PD), plaque index, gingival index (GI), mobility, sensitivity, and bleeding on probing (BOP) index. This study included 60 mandibular 1st molars from 52 participants (20 males and 32 females) requiring crown restoration. The margin lines of the crown preparations were placed 1 mm subgingivally. Based on the gingival displacement technique used, the patients were divided into three groups: retraction cord, cordless paste system, and Er,Cr:YSGG laser troughing. A digital scan of the prepared tooth was performed. Follow-up appointments were scheduled at five different times: 1st day, 1st month, 3rd month, 6th month, and 1st year. Six periodontal indices were used to assess the periodontal health. The chi-square test was used to compare categorical variables depending on the groups. There was a significant difference in the PD, GI, and BOP index scores among the three techniques during the 1-year clinical monitoring (p < 0.001). The PD in the three zones of the buccal surface showed a significant increase with time in the retraction cord and cordless paste system groups (p < 0.001). The highest GI scores were observed in the retraction cord group on the 1st day. The Er,Cr:YSGG laser troughing procedure produced lower PD, GI, and BOP index scores as compared to the retraction cord and cordless paste system procedures in the 1-year period.





Similar content being viewed by others
References
Pjetursson BE, Sailer I, Makarov NA, Zwahlen M, Thoma DS (2015) All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part II: Multiple-unit FDPs. Dent Mater 31(6):624–639. https://doi.org/10.1016/j.dental.2015.02.013
Stuffken M, Vahidi F (2016) Preimpression troughing with the diode laser: a preliminary study. J Prosthet Dent 115(4):441–446. https://doi.org/10.1016/j.prosdent.2015.10.008
Marotti J, Broeckmann J, Chuembou Pekam F, Praca L, Radermacher K, Wolfart S (2019) Impression of subgingival dental preparation can be taken with ultrasound. Ultrasound Med Biol 45(2):558–567. https://doi.org/10.1016/j.ultrasmedbio.2018.09.027
Samet N, Shohat M, Livny A, Weiss EI (2005) A clinical evaluation of fixed partial denture impressions. J Prosthet Dent 94(2):112–117. https://doi.org/10.1016/j.prosdent.2005.05.002
Tabassum S, Adnan S, Khan FR (2017) Gingival retraction methods: a systematic review. J Prosthodont 26(8):637–643. https://doi.org/10.1111/jopr.12522
Goutham GB, Jayanti I, Jalaluddin M, Avijeeta A, Ramanna PK, Joy J (2018) Clinical assessment of gingival sulcus width using various gingival displacement materials. J Contemp Dent Pract 19(5):502–506
Donovan TE, Chee WWL (2004) Current concepts in gingival displacement. Dent Clin N Am 48(2):433–444. https://doi.org/10.1016/j.cden.2003.12.012
Punj A, Bompolaki D, Garaicoa J (2017) Dental impression materials and techniques. Dent Clin N Am 61(4):779–796. https://doi.org/10.1016/j.cden.2017.06.004
Winkelmeyer C, Wolfart S, Marotti J (2016) Analysis of tooth preparations for zirconia-based crowns and fixed dental prostheses using stereolithography data sets. J Prosthet Dent 116(5):783–789. https://doi.org/10.1016/j.prosdent.2016.03.019
Gherlone EF, Maiorana C, Grassi RF, Ciancaglini R, Cattoni F (2004) The use of 980-nm diode and 1064-nm Nd: YAG laser for gingival retraction in fixed prostheses. J Oral Laser Appl 4(3):183–190
Alghazzawi TF (2016) Advancements in CAD/CAM technology: options for practical implementation. J Prosthodont Res 60(2):72–84. https://doi.org/10.1016/j.jpor.2016.01.003
Rayyan MM, Hussien ANM, Sayed NM, Abdallah R, Osman E, El Saad NA, Ramadan S (2019) Comparison of four cordless gingival displacement systems: a clinical study. J Prosthet Dent 121(2):265–270. https://doi.org/10.1016/j.prosdent.2018.05.010
Zimmermann M, Mehl A, Mormann WH, Reich S (2015) Intraoral scanning systems - a current overview. Int J Comput Dent 18(2):101–129
Nedelcu RG, Persson AS (2014) Scanning accuracy and precision in 4 intraoral scanners: an in vitro comparison based on 3-dimensional analysis. J Prosthet Dent 112(6):1461–1471. https://doi.org/10.1016/j.prosdent.2014.05.027
Lee JJ, Jeong ID, Park JY, Jeon JH, Kim JH, Kim WC (2017) Accuracy of single-abutment digital cast obtained using intraoral and cast scanners. J Prosthet Dent 117(2):253–259. https://doi.org/10.1016/j.prosdent.2016.07.021
Mangano F, Gandolfi A, Luongo G, Logozzo S (2017) Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health 17(1):149. https://doi.org/10.1186/s12903-017-0442-x
Al Hamad KQ, Azar WZ, Alwaeli HA, Said KN (2008) A clinical study on the effects of cordless and conventional retraction techniques on the gingival and periodontal health. J Clin Periodontol 35(12):1053–1058. https://doi.org/10.1111/j.1600-051X.2008.01335.x
Tao X, Yao JW, Wang HL, Huang C (2018) Comparison of gingival troughing by laser and retraction cord. Int J Periodontics Restorative Dent 38(4):527–532. https://doi.org/10.11607/prd.3551
Sarmento HR, Leite FR, Dantas RV, Ogliari FA, Demarco FF, Faot F (2014) A double-blind randomised clinical trial of two techniques for gingival displacement. J Oral Rehabil 41(4):306–313. https://doi.org/10.1111/joor.12142
Akca EA, Yildirim E, Dalkiz M, Yavuzyilmaz H, Beydemir B (2006) Effects of different retraction medicaments on gingival tissue. Quintessence Int 37(1):53–59
Mizutani K, Aoki A, Coluzzi D, Yukna R, Wang C-Y, Pavlic V (2000) Izumi Y (2016) Lasers in minimally invasive periodontal and peri-implant therapy. Periodontology 71(1):185–212. https://doi.org/10.1111/prd.12123
Jetter C (2008) Soft-tissue management using an Er,Cr:YSGG laser during restorative procedures. Compend Contin Educ Dent 29(1):46–49
Azzi R, Tsao TF, Carranza FA Jr, Kenney EB (1983) Comparative study of gingival retraction methods. J Prosthet Dent 50(4):561–565. https://doi.org/10.1016/0022-3913(83)90581-4
Sulieman M (2005) An overview of the use of lasers in general dental practice: 2. Laser wavelengths, soft and hard tissue clinical applications. Dent Update 32(5):286–296. https://doi.org/10.12968/denu.2005.32.5.286
Sulieman M (2005) An overview of the use of lasers in general dental practice: 1. Laser physics and tissue interactions. Dent Update 32(4):228–236. https://doi.org/10.12968/denu.2005.32.4.228
Krishna Ch V, Gupta N, Reddy KM, Sekhar NC, Aditya V, Reddy GV (2013) Laser gingival retraction: a quantitative assessment. J Clin Diagn Res 7(8):1787–1788. https://doi.org/10.7860/jcdr/2013/5954.3292
Wilder-Smith P, Dang J, Kurosaki T (1997) Investigating the range of surgical effects on soft tissue produced by a carbon dioxide laser. J Am Dent Assoc 128(5):583–588. https://doi.org/10.14219/jada.archive.1997.0257
Akram Z, Shafqat SS, Niaz MO, Raza A, Naseem M (2020) Clinical efficacy of photodynamic therapy and laser irradiation as an adjunct to open flap debridement in the treatment of chronic periodontitis: a systematic review and meta-analysis. Photodermatol Photoimmunol Photomed 36(1):3–13. https://doi.org/10.1111/phpp.12499
Bennani V, Aarts JM, Schumayer D (2016) Correlation of pressure and displacement during gingival displacement: an in vitro study. J Prosthet Dent 115(3):296–300. https://doi.org/10.1016/j.prosdent.2015.08.008
Löe H, Silness J (1963) Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand 21(6):533–551. https://doi.org/10.3109/00016356309011240
Silness J, Löe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22(1):121–135. https://doi.org/10.3109/00016356408993968
Laster L, Laudenbach KW, Stoller NH (1975) An evaluation of clinical tooth mobility measurements. J Periodontol 46(10):603–607. https://doi.org/10.1902/jop.1975.46.10.603
Schiff T, Dotson M, Cohen S, De Vizio W, McCool J, Volpe A (1994) Efficacy of a dentifrice containing potassium nitrate, soluble pyrophosphate, PVM/MA copolymer, and sodium fluoride on dentinal hypersensitivity: a twelve-week clinical study. J Clin Dent 5 Spec No:87–92
Wang Y, Fan F, Li X, Zhou Q, He B, Huang X, Huang S, Ma J (2019) Influence of gingival retraction paste versus cord on periodontal health: a systematic review and meta-analysis. Quintessence Int 50(3):234–244. https://doi.org/10.3290/j.qi.a41976
Breen HJ, Rogers P, Johnson NW, Slaney R (1999) Option-4 algorithm for Florida pocket depth probe: reduction in the variance of site-specific probeable crevice depth measurements. J Clin Periodontol 26(8):511–518. https://doi.org/10.1034/j.1600-051x.1999.260804.x
Alhajj WA (2020) Gingival phenotypes and their relation to age, gender and other risk factors. BMC Oral Health 20(1):87. https://doi.org/10.1186/s12903-020-01073-y
Harrison JD (1961) Effect of retraction materials on the gingival sulcus epithelium. J Prosthet Dent 11(3):514–521. https://doi.org/10.1016/0022-3913(61)90234-7
Feng J, Aboyoussef H, Weiner S, Singh S, Jandinski J (2006) The effect of gingival retraction procedures on periodontal indices and crevicular fluid cytokine levels: a pilot study. J Prosthodont 15(2):108–112. https://doi.org/10.1111/j.1532-849X.2006.00083.x
Melilli D, Mauceri R, Albanese A, Matranga D, Pizzo G (2018) Gingival displacement using diode laser or retraction cords: a comparative clinical study. Am J Dent 31(3):131–134
Dederichs M, Fahmy MD, Kuepper H, Guentsch A (2019) Comparison of gingival retraction materials using a new gingival sulcus model. J Prosthodont 28(7):784–789. https://doi.org/10.1111/jopr.13093
Bennani V, Inger M, Aarts JM (2014) Comparison of pressure generated by cordless gingival displacement materials. J Prosthet Dent 112(2):163–167. https://doi.org/10.1016/j.prosdent.2013.09.035
Phatale S, Marawar P, Byakod G, Lagdive S, Kalburge J (2010) Effect of retraction materials on gingival health: a histopathological study. J Indian Soc Periodontol 14(1):35–39. https://doi.org/10.4103/0972-124x.65436
Chandra S, Singh A, Gupta KK, Chandra C, Arora V (2016) Effect of gingival displacement cord and cordless systems on the closure, displacement, and inflammation of the gingival crevice. J Prosthet Dent 115(2):177–182. https://doi.org/10.1016/j.prosdent.2015.06.023
Kazemi M, Memarian M, Loran V (2009) Comparing the effectiveness of two gingival retraction procedures on gingival recession and tissue displacement: clinical study. Res J Biol Sci 4(3):335–339
Huang C, Somar M, Li K, Mohadeb JVN (2017) Efficiency of cordless versus cord techniques of gingival retraction: a systematic review. J Prosthodont 26(3):177–185. https://doi.org/10.1111/jopr.12352
Ashri NY, Ai Rifaiy M, EI-Metwally A (2016) The effect of gingival retraction cord on periodontal health compared to other gingival retraction procedures: a systematic review. Periodontics Prosthodontics 2(3):19
Midwood I, Davies M, Newcombe RG, West N (2019) Patients’ perception of their oral and periodontal health and its impact: a cross-sectional study in the NHS. Br Dent J 227(7):587–593. https://doi.org/10.1038/s41415-019-0721-9
Chabanski MB, Gillam DG, Bulman JS, Newman HN (1997) Clinical evaluation of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department: a pilot study. J Oral Rehabil 24(9):666–672. https://doi.org/10.1046/j.1365-2842.1997.00552.x
Cortellini P, Tonetti MS, Lang NP, Suvan JE, Zucchelli G, Vangsted T, Silvestri M, Rossi R, McClain P, Fonzar A, Dubravec D, Adriaens P (2001) The simplified papilla preservation flap in the regenerative treatment of deep intrabony defects: clinical outcomes and postoperative morbidity. J Periodontol 72(12):1702–1712. https://doi.org/10.1902/jop.2001.72.12.1702
Needleman I, McGrath C, Floyd P, Biddle A (2004) Impact of oral health on the life quality of periodontal patients. J Clin Periodontol 31(6):454–457. https://doi.org/10.1111/j.1600-051X.2004.00498.x
Funding
This research was financially supported by Van Yuzuncu Yil University, Scientific Research Project Division (TSA-2019-7920).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This clinical trial was approved by Yuzuncu Yil University Medical Faculty Interventional Research Ethical Council (Resolution No: 05 Date: 13-11-2018). The international ClinicalTrials.gov study registry of the study was conducted on 17/01/2019 (NCT 03816930). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its latter amendments or comparable ethical standards.
Informed consent
All volunteers included in the study were informed about the purpose and method of the study and signed an informed consent form.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ünalan Değirmenci, B., Karadağ Naldemir, B. & Değirmenci, A. Evaluation of gingival displacement methods in terms of periodontal health at crown restorations produced by digital scan: 1-year clinical follow-up. Lasers Med Sci 36, 1323–1335 (2021). https://doi.org/10.1007/s10103-021-03266-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03266-5