Abstract
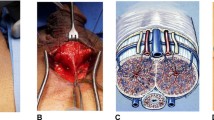
The artificial urinary sphincter, known as AMS 800, has been the gold standard for treating moderate to severe stress urinary incontinence in males for 40 years. Yet, the number of sphincters done globally is quite small and the majority of urologists doing them are infrequent implanters. Estimates for 2019 showed half of implanters did only one implant that year and worldwide only around 13,000 implantations were performed. The traditional two-incision technique of perineal exposure for cuff placement and abdominal incision for pump and pressure regulating balloon persists as the most common technique to surgically place an artificial urinary sphincter. Present estimates are that upwards of 80% are done via the perineal approach and that approach is the highly favored incision of large volume centers. The scrotal one-incision approach was invented by Wilson 20 years ago and was aimed at making the implantation of a sphincter quicker, easier and safer for the occasional implanter. These physicians perform 1–2 devices per year, comprise 60% of implanters who perform the surgery yearly, and implant 22% of all implanted devices. Our article targets these infrequent inserters discussing the history of the two techniques and what the authors have learned about the advantages and hazards of the one scrotal incision procedure over the last two decades.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
References
Scott FB, Bradley WE, Timm GW. Treatment of urinary incontinence by implantable prosthetic sphincter. Urology. 1973;1:252–9.
Wilson S, Delk FR, Henry GD, Siegel AL. New surgical technique for sphincter urinary control system using upper transverse scrotal incision. J Urol. 2003;169:261–4.
James MH, McCammon KA. Artificial urinary sphincter for post-prostatectomy incontinence: a review. Int J Urol. 2014;21:536–43.
Wilson SK, Delk JR, Salem EA, Cleves MA. Long-term survival of inflatable penile prostheses: single surgical group experience with 2384 first-time implants spanning two decades. J Sex Med. 2007;4:1074–9.
Fuller TW, Ballon-Landa E, Gallo Kelsey, Smith TG, Ajay D, Westney OL, et al. Outcomes and risk factors of revision and replacement artificial urinary sphincter implantation in radiated and non-radiated patients. J Urol. 2020. https://doi.org/10.1097/JU.0000000000000749.
Ravier E, Fassi-Fehri H, Crouzet S, Gelet A, Abid N, Martin X. Complications after artificial urinary sphincter implantation in patients with or without prior radiotherapy. BJU Int. 2015;115:300–7.
Van der AF, drake MJ, Kasyan GR, Petrolekas A, Cornu JN. Young Academic Urologists Functional Urology Group. The artificial urinary sphincter after a quarter of century: a critical systematic review of its use in male non-neurogenic incontinence. Eur Urol. 2013;63:681–9.
Shen YC, Chiang PH. The experience of artificial urinary sphincter implantation by a single surgeon in 15 years. Kaohsiung J Med Sci. 2013;29:157–60.
Kretschmer A, Husch T, Thomsen Frauke, Kronlachner D, Obaje A, Anding R. Complications and short-term explantation rate following artificial urinary sphincter implantation: results from a large middle European multi-institutional case series. Urol Int. 2016;97:205–11.
Demographics provided by Boston Scientific Marketing Department as per Wasscher B and Keefe V per Email on 4/23/2020
Matsushita K, Chughtai BI, Maschino AC, Lee RK, Sandhu JS. International variation in artificial urinary sphincter use. Urology. 2012;80:667–72.
Furlow WL. Implantation of a new semiautomatic artificial genitourinary sphincter: experience with primary activation and deactivation in 47 patients. J Urol. 1981;126:741–44.
Scott FB. The artificial urinary sphincter. Experience in adults. Urol Clin North Am. 1985;12:305–15.
Ludwig T, Dahlem R, Fisch M. Basic perineal and scrotal techniques. In: Moncada II, Martinez-Salamanca JI, Lledo-Garcia E, Mulcahy JJ. Textbook of urogenital prosthetic surgery. S.A. Madrid Spain: Editorial Medica Pan Americana; 2020. p. 271.
Mulcahy JJ. Tips for successful placement of artificial urinary sphincter. Contemp Urol. 1999;11:å46–51.
Wilson SK, Delk JR. Ectopic placement of AMS 800 urinary control system pressure regulating balloon. Urology. 2005;65:167–70.
Morey AF, Cefalu CA, Hudak SJ. High submuscular placement of urologic prosthetic balloons and reservoirs vis transcrotal approach. J Sex Med. 2013;10:603–10.
Brito CG, Mulcahy JJ, Mitchel ME, Adams MC. Use of a double cuff AMS800 urinary sphincter for severe stress incontinence. J Urol. 1993;149:283–5.
O’Connor RC, Lyon MB, Guralnick ML, Bales GT. Long-term follow-up of single versus double cuff artificial urinary sphincter insertion for the treatment of severe postprostatectomy stress urinary incontinence. Urology. 2008;71:90–3.
Guralnick ML, Miller E, Toh KL, Webster GD. Transcorporal artificial urinary sphincter cuff placement in cases requiring revision for erosion and urethral atrophy. J Urol. 2002;167:2075–8.
Sotelo TM, Westney OL. Outcomes related to placing an artificial urinary sphincter using a single-incision, transverse scrotal technique in high risk patients. BJU Int. 2008;101:1124–7.
Henry GD, Graham SM, Cleves MA, Simmons CJ, Flynn B. Perineal approach for artificial urinary sphincter implantation appears to control male stress incontinence better than the transscrotal approach. J Urol. 2008;179:1475–9.
Henry GD, Graham SM, Cornell RJ, Cleves MA, Simmons CJ, Vakalopoulos I, et al. A multicenter study on the perineal versus penoscrotal approach for implantation of artificial urinary sphincter: cuff size and control of male stress urinary incontinence. J Urol. 2009;182:2404–9.
Wilson SK, Aliotta PJ, Salem EA, Mulcahy JJ. New enhancement of the scrotal one-incision technique for placement of artificial urinary sphincter allow proximal cuff placement. J Sex Med. 2010;7:3510–15.
Queissert F, Huesch T, Kretschmer A, Anding R, Kurosch M, kirschner-Hermans R, et al. Artificial urinary sphincter cuff size predicts outcome in male patients treated for stress incontinence: results of a large central European multicenter cohort study. Int Neurourol J. 2019;23:219–25.
Kretschner A, Husch Tanja, Thomsen F, Kronlachner D, Obaje A, Anding R, et al. Debates on Male Incontinence (DOMINO)-project. Complications and short-term explantation rate following artificial urinary sphincter implantation: results from a large middle European multi-institutional case series. Urol Int. 2016;97:205–11.
Shen YC, Chiang PH. Is the penoscrotal approach inferior to the perineal approach for artificial sphincter implantation in male urinary incontinence? A preliminary experience. Int J Urol. 2012;19:786–9.
Yafi FA, Delay KJ, Stewart C, Chiang J, Sangkum P, Hellstrom WJG. Device survival after primary implantation of an artificial urinary sphincter for male stress urinary incontinence. J Urol. 2017;197:759–65.
Staniorski CJ, Singal A, nettey O, Yura E, Keeter MK, Kieb S, Hofer MD. Revisiting the peonscrotal approach to artificial urinary sphincter surgery: how does it compare to the perineal incision for initial implantation? World J Urol 2020; https://doi.org/10.1007/s00345-020-03244-6. [Epub ahead of print].
Jamaer C, Bruyn HD, van Renterghem A, Baten E, van Renterghem K. Penoscrotal incision for primary implantation of AMS 800 urinary sphincter. J Sex med. 2019;16 Suppl 2:S22.
Bugeja S, Ivaz SL, Frost A, Andrich DE, Mundy AR. Urethral atrophy after implantation of an artificial urinary sphincter: fact or fiction? BJU Int. 2016;123:252–7.
Terlecki R, Wilson SK. A new paradigm for surgical revision of the artificial urinary sphincter for recurrent stress urinary incontinence. Int J Impot Res. 2020. [Epub ahead of print].
Rehder P, Gozzi C. Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol. 2007;52:860–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SKW: Consultant: AMT, Coloplast, International Medical Devices, Lecturer: Boston Scientific, Stockholder: NeoTract. OLW: Consultant: Boston Scientific. JJM: Consultant: Boston Scientific, Coloplast.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wilson, S.K., Westney, O.L. & Mulcahy, J.J. Twenty years later: is the scrotal one-incision AUS of value?. Int J Impot Res 34, 243–251 (2022). https://doi.org/10.1038/s41443-020-0317-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0317-6
This article is cited by
-
First safety outcomes for rigicon conticlassic® artificial urinary sphincter
International Journal of Impotence Research (2023)