Abstract
Aims
The relationship between bisphenol A (BPA) and diabetes remains controversial. This study aims to investigate whether serum BPA level could predict the 5-year incidence of type 2 diabetes (T2D).
Methods
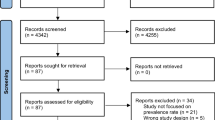
A nested case–control study was performed among Chinese who participated in the environment, inflammation and metabolic diseases study (2008–2013). Of the 3510 subjects who were free of diabetes, 232 subjects developed diabetes during the 5-year follow-up. Cases and controls were matched for age and gender by a ratio of 1:1. Homoeostasis model assessment was used to estimate basal β-cell function (HOMA-β) and insulin resistance (HOMA-IR). Participants were stratified into tertiles based on low, median and high baseline serum BPA levels. Regression models were used to analyze the relationship between serum BPA concentration and the incidence of T2D.
Results
At baseline, no significant difference in serum BPA concentration was observed between patients with T2D and controls [1.3 (0.3, 3.7) vs. 1.6 (0.4, 3.9) μmol/L, P = 0.199]; serum BPA concentration was positively associated with fasting plasma glucose (r = 0.27, P < 0.001); however, neither HOMA-β nor HOMA-IR correlated with serum BPA concentration. During the follow-up, baseline BPA levels could not predict the 5-year T2D incidence, whether or not adjusted for the potential confounders such as body mass index and blood pressure. [Low BPA tertile was the reference, OR 0.66 (95% CI 0.30, 1.44) for median, OR 0.93 (95% CI 0.41, 2.13) for high.]
Conclusion
BPA is not associated with a 5-year T2D incidence. These data do not support previous cross-sectional study that BPA exerted a detrimental effect on glucose metabolism.


Similar content being viewed by others
References
Menke A, Casagrande S, Geiss L, Cowie CC (2015) Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 314:1021–1029
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q et al (2017) Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317:2515–2523
Xu Y, Wang L, He J, Bi Y, Li M, Wang T et al (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310:948–959
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J et al (2010) Prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101
Ruiz D, Becerra M, Jagai JS, Ard K, Sargis RM (2018) Disparities in environmental exposures to endocrine-disrupting chemicals and diabetes risk in vulnerable populations. Diabetes Care 41:193–205
Song Y, Chou EL, Baecker A, You NC, Song Y, Sun Q et al (2016) Endocrine-disrupting chemicals, risk of type 2 diabetes, and diabetes-related metabolic traits: a systematic review and meta-analysis. J Diabetes 8:516–532
Vandenberg LN, Maffini MV, Sonnenschein C, Rubin BS, Soto AM (2009) Bisphenol-A and the great divide: a review of controversies in the field of endocrine disruption. Endocr Rev 30:75–95
Song Y, Hauser R, Hu FB, Franke AA, Liu S, Sun Q (2014) Urinary concentrations of bisphenol A and phthalate metabolites and weight change: a prospective investigation in US women. Int J Obes (Lond) 38:1532–1537
Melzer D, Osborne NJ, Henley WE, Cipelli R, Young A, Money C et al (2012) Urinary bisphenol A concentration and risk of future coronary artery disease in apparently healthy men and women. Circulation 125:1482–1490
Bae S, Hong YC (2015) Exposure to bisphenol A from drinking canned beverages increases blood pressure: randomized crossover trial. Hypertension 65:313–319
Moon MK, Jeong IK, Oh TJ, Ahn HY, Kim HH, Park YJ et al (2015) Long-term oral exposure to bisphenol A induces glucose intolerance and insulin resistance. J Endocrinol 226:35–42
Jayashree S, Indumathi D, Akilavalli N, Sathish S, Selvaraj J, Balasubramanian K (2013) Effect of bisphenol-A on insulin signal transduction and glucose oxidation in liver of adult male albino rat. Environ Toxicol Pharmacol 35:300–310
Lin Y, Sun X, Qiu L, Wei J, Huang Q, Fang C et al (2013) Exposure to bisphenol A induces dysfunction of insulin secretion and apoptosis through the damage of mitochondria in rat insulinoma (INS-1) cells. Cell Death Dis 4:e460
Lang IA, Galloway TS, Scarlett A, Henley WE, Depledge M, Wallace RB et al (2008) Association of urinary bisphenol A concentration with medical disorders and laboratory abnormalities in adults. JAMA 300:1303–1310
Aekplakorn W, Chailurkit LO, Ongphiphadhanakul B (2015) Relationship of serum bisphenol A with diabetes in the Thai population, National Health Examination Survey IV, 2009. J Diabetes 7:240–249
Sun Q, Cornelis MC, Townsend MK, Tobias DK, Eliassen AH, Franke AA et al (2014) Association of urinary concentrations of bisphenol A and phthalate metabolites with risk of type 2 diabetes: a prospective investigation in the Nurses’ health study (NHS) and NHSII cohorts. Environ Health Perspect 122:616–623
Hu J, Yang S, Wang Y, Goswami R, Peng C, Gao R et al (2015) Serum bisphenol A and progression of type 2 diabetic nephropathy: a 6-year prospective study. Acta Diabetol 52:1135–1141
Hu J, Wang Y, Xiang X, Peng C, Gao R, Goswami R et al (2016) Serum bisphenol A as a predictor of chronic kidney disease progression in primary hypertension: a 6-year prospective study. J Hypertens 34:332–337
Weng J, Li Y, Xu W, Shi L, Zhang Q, Zhu D et al (2008) Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet 371:1753–1760
Shankar A, Teppala S (2011) Relationship between urinary bisphenol A levels and diabetes mellitus. J Clin Endocrinol Metab 96:3822–3826
Bi Y, Wang W, Xu M, Wang T, Lu J, Xu Y et al (2016) Diabetes genetic risk score modifies effect of bisphenol A exposure on deterioration in glucose metabolism. J Clin Endocrinol Metab 101:143–150
Stojanoska MM, Milosevic N, Milic N, Abenavoli L (2017) The influence of phthalates and bisphenol A on the obesity development and glucose metabolism disorders. Endocrine 55:666–681
Alonso-Magdalena P, Morimoto S, Ripoll C, Fuentes E, Nadal A (2006) The estrogenic effect of bisphenol A disrupts pancreatic beta-cell function in vivo and induces insulin resistance. Environ Health Perspect 114:106–112
Wang X, Wang X, Chen Q, Luo ZC, Zhao S, Wang W et al (2017) Urinary bisphenol A concentration and gestational diabetes mellitus in Chinese women. Epidemiology 28(Suppl 1):S41–S47
Acknowledgements
The authors thank Laboratory of Endocrine and the Laboratory of Lipid & Glucose Metabolism, the First Affiliated Hospital of Chongqing Medical University.
Funding
National key research & development plan, major project of precision medicine research (2017YFC0909600, sub-project: 2017YFC0909602, 2017YFC0909603). National Key Clinical Specialties Construction Program of China to the Department of Endocrinology, the First Affiliated Hospital of Chongqing Medical University; and the National Natural Science Foundation of China (81370954, 81670785) to Qifu Li; and the Fundamental Science & Advanced Technology Research of Chongqing (Major Project, cstc2015jcyjBX0096) to Qifu Li. Chongqing Science and Technology Committee Innovation Project (Technology Development and Application of Precision Medicine, cstc2016shms-ztzx1003) to Qifu Li.
Author information
Authors and Affiliations
Contributions
Xiaoyu Shu and Siying Tang designed the study, oversaw the data collection and wrote the manuscript. Chuan Peng and Rufei Gao conducted the data analysis and contributed to the writing of the manuscript. Shumin Yang, Ting Luo and Yue Wang contributed to the study design and provided statistical expertise. Qingfeng Cheng contributed to the writing of the manuscript. Zhihong Wang assisted with the data collection and contributed to the writing and editing of the manuscript. Qianna Zhen contributed to the writing of the manuscript. Jinbo Hu and Qifu Li are the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
All human studies have been reviewed by the committee and have been performed in accordance with the ethical standards laid down in an appropriate version of the 1964 Declaration of Helsinki.
Informed consent
All participants gave their informed consent prior to their inclusion in the study.
Additional information
Managed by Massimo Porta.
Xiaoyu Shu and Siying Tang are co-first authors.
Rights and permissions
About this article
Cite this article
Shu, X., Tang, S., Peng, C. et al. Bisphenol A is not associated with a 5-year incidence of type 2 diabetes: a prospective nested case–control study. Acta Diabetol 55, 369–375 (2018). https://doi.org/10.1007/s00592-018-1104-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1104-4