Trends in 10-Year Predicted Risk of Cardiovascular Disease Associated With Food Insecurity, 2007–2016
- 1Department of Cardiology, Westchester Medical Center and New York Medical College, Valhalla, NY, United States
- 2Department of Medicine, Westchester Medical Center and New York Medical College, Valhalla, NY, United States
- 3School of Medicine, St. George’s University, St. George’s, Grenada
Introduction: Consumption of a healthy diet improves cardiovascular (CV) risk factors and reduces the development of cardiovascular disease (CVD). Food insecure (FIS) adults often consume an unhealthy diet, which can promote obesity, type 2 diabetes mellitus (T2DM), hypertension (HTN), and hyperlipidemia (HLD). The Supplemental Nutrition Assistance Program (SNAP) is designed to combat food insecurity by increasing access to healthy foods. However, there is a paucity of data on the association of SNAP participation among FIS adults and these CVD risk factors.
Methods: The National Health and Nutrition Examination Survey (NHANES) is a publicly available, ongoing survey administered by the Centers for Disease Control and Prevention and the National Center for Health Statistics. We analyzed five survey cycles (2007–2016) of adult participants who responded to the CVD risk profile questionnaire data. We estimated the burden of select CVD risk factors among the FIS population and the association with participation in SNAP.
Results: Among 10,449 adult participants of the survey, 3,485 (33.3%) identified themselves as FIS. Food insecurity was more common among those who were younger, female, Hispanic, and Black. Among the FIS, SNAP recipients, when compared to non-SNAP recipients, had a lower prevalence of HLD (36.3 vs. 40.1% p = 0.02), whereas rates of T2DM, HTN, and obesity were similar. Over the 10-year survey period, FIS SNAP recipients demonstrated a reduction in the prevalence of HTN (p < 0.001) and HLD (p < 0.001) which was not evident among those not receiving SNAP. However, obesity decreased only among those not receiving SNAP. The prevalence of T2DM did not change over the study period in either group.
Conclusion: Over a 10-year period, FIS adults who received SNAP demonstrated a reduction in the prevalence of HTN and HLD, which was not seen among those not receiving SNAP. However, the prevalence of obesity and T2DM did not decline among SNAP recipients, suggesting that additional approaches are required to impact these important CVD risk factors.
Introduction
Cardiovascular disease (CVD) is a major global health challenge, and was responsible for 23% of total deaths in the United States (US) in 2017 (1). Consumption of a healthy and well-balanced diet is associated with better cardiovascular (CV) outcomes and has been demonstrated to improve CVD risk factors through decrease in body weight and various cardiometabolic pathways (2). Current guidelines emphasize a diet composed of fruits, vegetables, legumes, fish, nuts, whole grains, and fibers along with a reduction in sodium, processed meats, sugar-sweetened beverages (SSB), excess calories and refined foods (2, 3).
The US Department of Agriculture (USDA) defines food insecurity as economic and social conditions associated with limited and uncertain access to food (4). In 2018, 37.2 million Americans lived in food insecure (FIS) households (4). Inadequate financial resources, the high cost of food, and competing priorities often cause adults with food insecurity to consume an unhealthy and low quality diet (5–7). FIS adults often forgo purchasing specialized diets for medical conditions such as hypertension (HTN) or type 2 diabetes mellitus (T2DM) in favor of purchasing low-cost foods that are often energy dense but nutrient poor (8). As a result, food insecurity can lead to worsening of CVD risk factors including T2DM, HTN, hyperlipidemia (HLD), and obesity defined as BMI ≥ 30 kg/m2 (9), thus contributing to poor CV health.
The Supplemental Nutrition Assistance Program (SNAP, formerly called Food Stamps Program) is the largest federal food assistance program available for low-income households, and is designed to directly combat food insecurity (10). SNAP eligibility is based on household income, specifically targeting low income Americans living under the poverty level (11). Access to SNAP can potentially address high rates of CVD risk factors in FIS adults by increasing access to healthy foods. While few studies have shown a link between CVD risk factors and food insecurity (12, 13), there is a paucity of data on the association of SNAP participation amongst FIS adults and CVD risk factors. Understanding this relationship is important to determine whether any future expansions, additions or modifications to the SNAP program are needed to better serve the FIS population in the United States (US). We designed this study to investigate the prevalence of CV risk factors among the FIS population, and analyze the association between participation in SNAP and the change in CVD risk factors over a 10-year study period.
Materials and Methods
Data Source
The National Health and Nutrition Examination Survey (NHANES) is an ongoing cross-sectional survey administered by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics (NCHS). It is designed to describe the health and nutritional status of the non-institutionalized population of the United States (14). The NHANES database is publicly available for researchers, and the data are released in 2-year cycles. All NHANES participants complete an English or Spanish language questionnaire during a home interview. Participants then undergo a standardized physical examination (including height, weight).
Food Security
The food security module within NHANES is a questionnaire developed by the USDA to measure adult food security over the 12 months preceding the survey. Adult food security is categorized by NHANES as: full food security, marginal food security, low food security, and very low food security. In this study, we considered adults in the full food security category to be food secure (FS) and those categorized as having marginal, low and very low food security to be FIS.
Study Population
We analyzed 10-year data from five survey cycles completed by adult participants ≥ 18 years of age, from months of January to December (2007–2008, 2009–2010, 2011–2012, 2013–2014, and 2014–2016). A total of 10,449 adults who participated in the NHANES surveys from 2007 to 2016 were included in the full analytic sample. From this cohort, 6,964 adults were identified as FS (66.6%), and 3,485 adults were identified as FIS (33.3%). The FIS adult participants were further categorized into those receiving SNAP benefits (63.3%) and those not receiving SNAP benefits (36.6%).
The presence or absence of each CVD risk factor (T2DM, HTN, HLD, obesity) was determined based on the response to the survey question: “Have you ever been diagnosed by a physician with this risk factor?” Respondents who were classified as SNAP participants, had accepted SNAP benefits in the 12 months preceding the survey.
Statistical Analysis
All analyses were performed using SPSS, version 26 (IBM, Chicago). Stratified weighted data were utilized to obtain nationwide estimates. Continuous variables were reported as mean ± standard deviation and compared using the Student t-test, and the categorical variables were reported as proportions and compared using the Chi-square test. We used multiple logistic regression analysis to determine temporal trends with survey year as the independent variable and the CV risk factor of interest as the dependent variable. The yearly prevalence of various CV risk factors among the study cohorts was reported along with P-trend.
Results
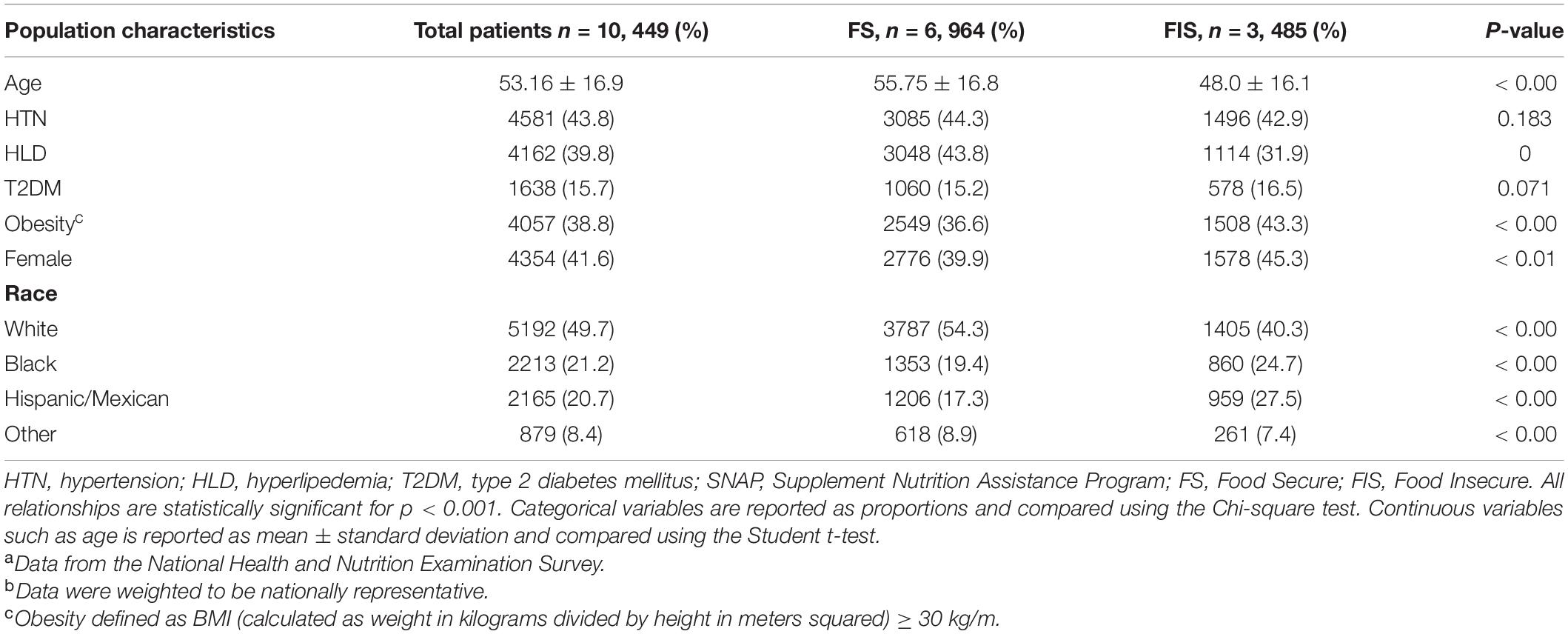
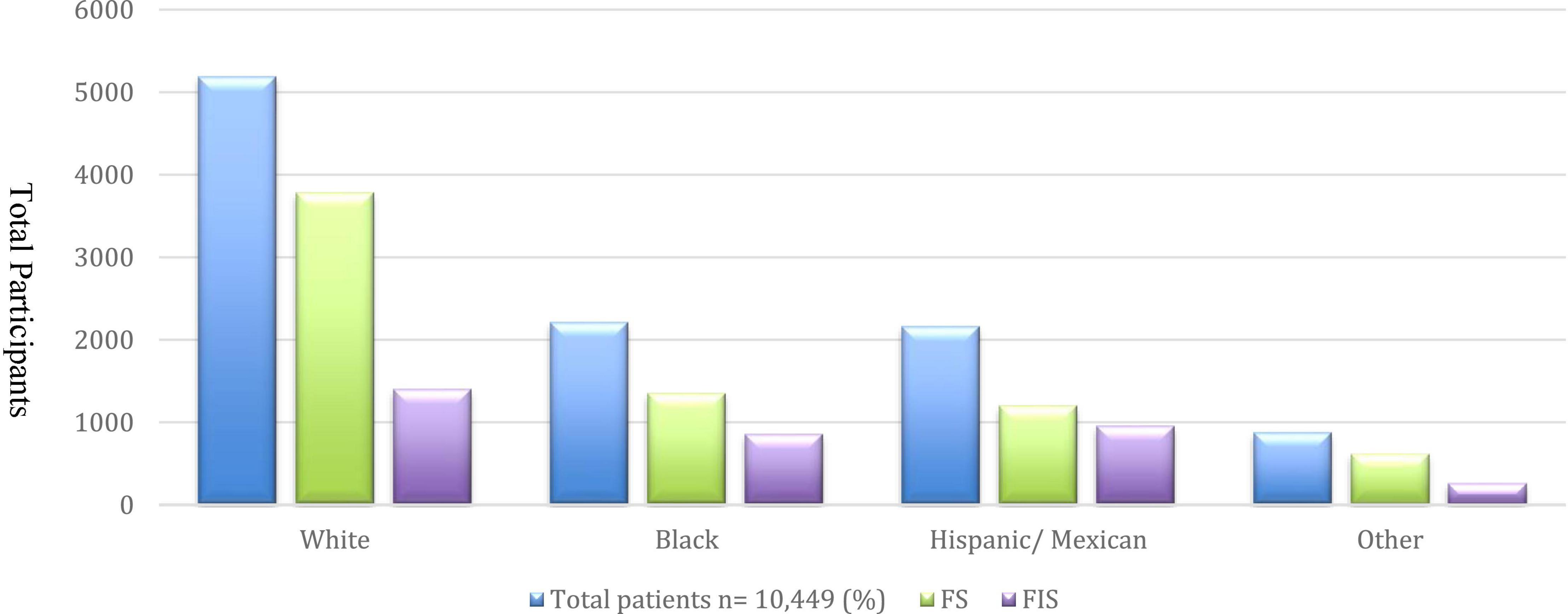
A total of 10,449 adults (mean age 53.16 ± 16.9, 41.6% females) who participated in the NHANES surveys from 2007 to 2016 were included in the full analytic sample. From this cohort, 6,964 adults were identified as FS (66.6%), and 3,485 adults were identified as FIS (33.3%). The prevalence of CVD risk factors in the total population, and according to food security status is shown in Table 1. CVD risk factors were highly prevalent among all participants. FIS adults were younger than those who were FS. The proportion of females (Table 1) and self-identified Blacks and Hispanics was higher among FIS participants than FS participants of the survey (Figure 1). The prevalence of HLD and obesity were significantly higher among those with FIS, whereas rates of HTN and T2DM were similar in the two groups.
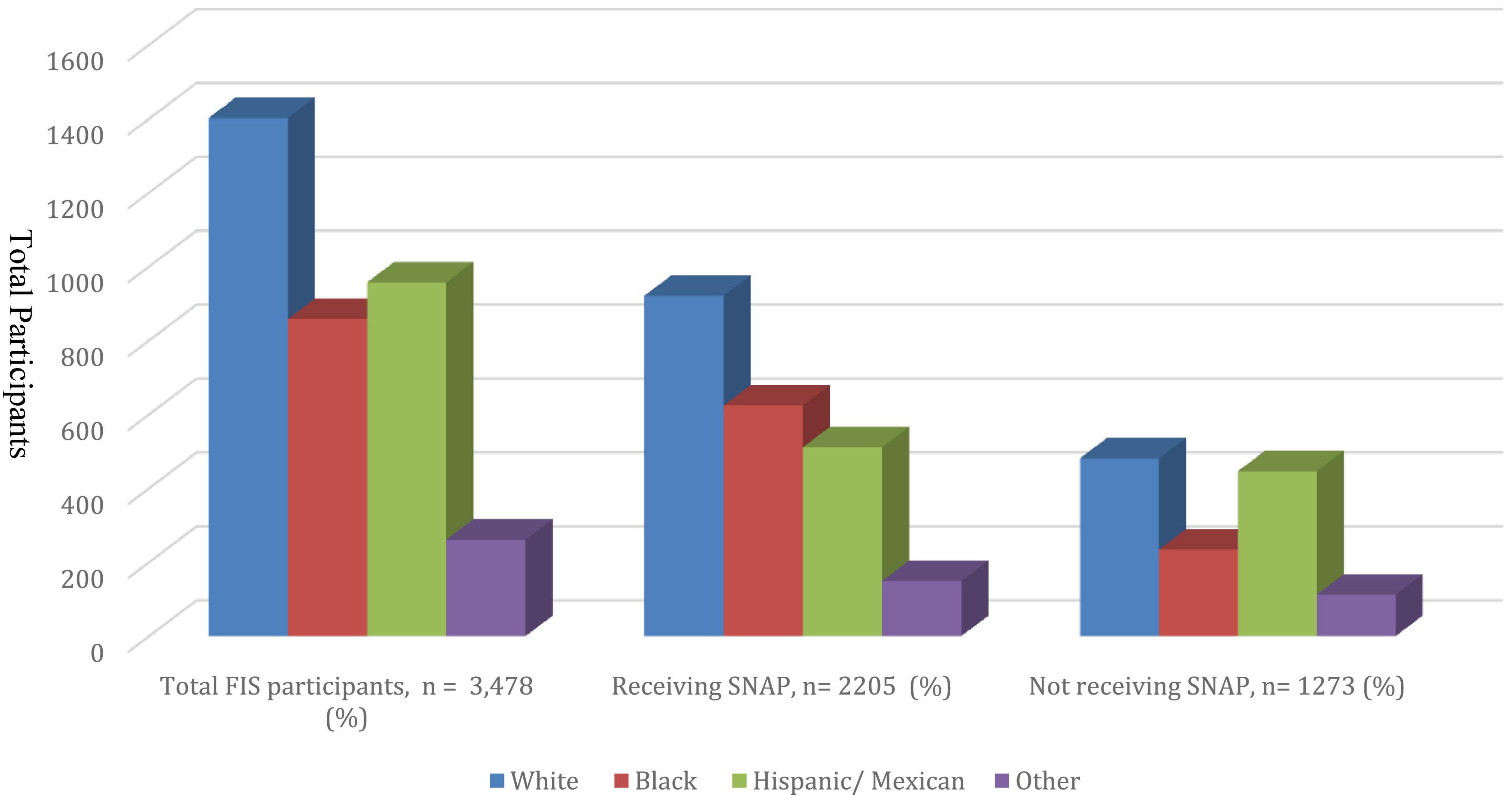
Characteristics of the FIS participants according to receipt of SNAP benefits are described in Table 2. Those receiving SNAP comprised 63.4% of the FIS population. SNAP participants were younger and more likely to be female and non-white. Among the FIS, higher proportion of self-identified whites (41.8%), participated in SNAP compared to self-identified Hispanics/Mexicans (23.2%) (Figure 2). As described in Table 2, FIS participants who received SNAP had a lower prevalence of HLD compared to those who did not receive SNAP (36.3 vs. 40.1%, p = 0.02). There was no significant difference in the prevalence of T2DM, HTN, or obesity between FIS participants receiving SNAP and FIS participants not receiving SNAP.
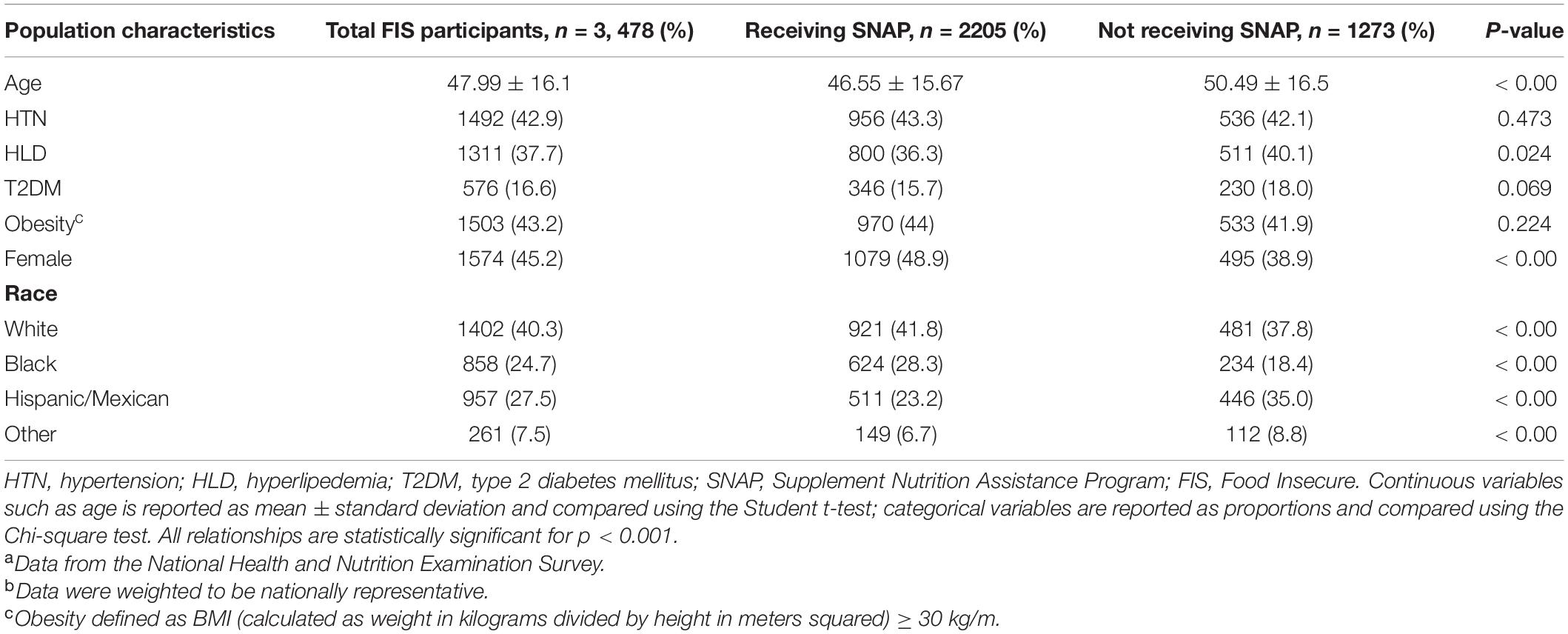
Table 2. Baseline characteristics of the adult food insecure participants of the survey, 2007–2016a–b.
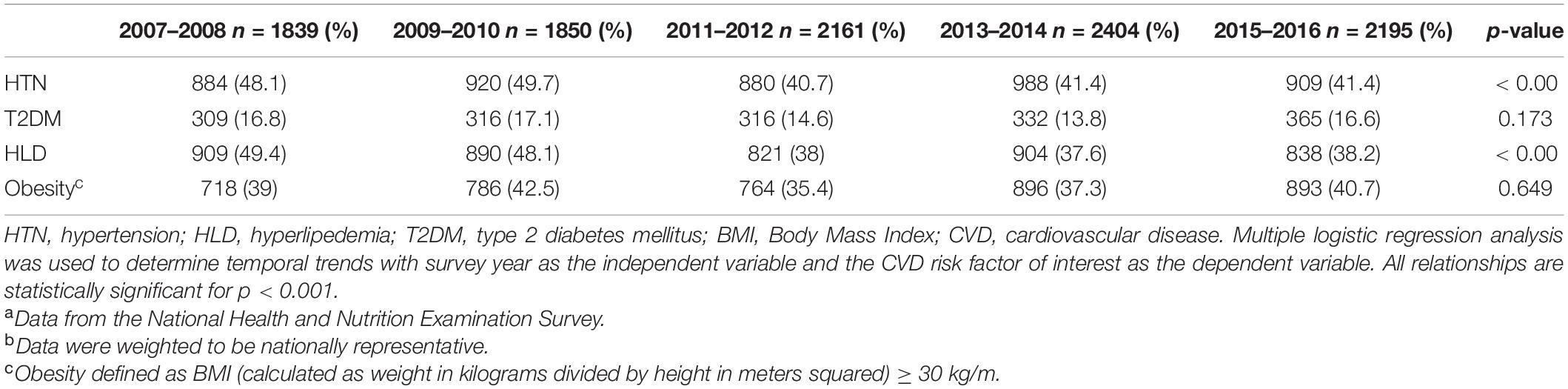
Among all NHANES participants, the prevalence of HTN and HLD decreased over the 10-year study period (Table 3). Rates of T2DM and obesity remained unchanged over the study period in the total population (Table 3). When analyzed according to food security status, similar trends were seen in both FS and FIS groups (Table 4). The prevalence of HTN and HLD showed statistically significant decrease over the study period in both FS and FIS groups (Table 4).
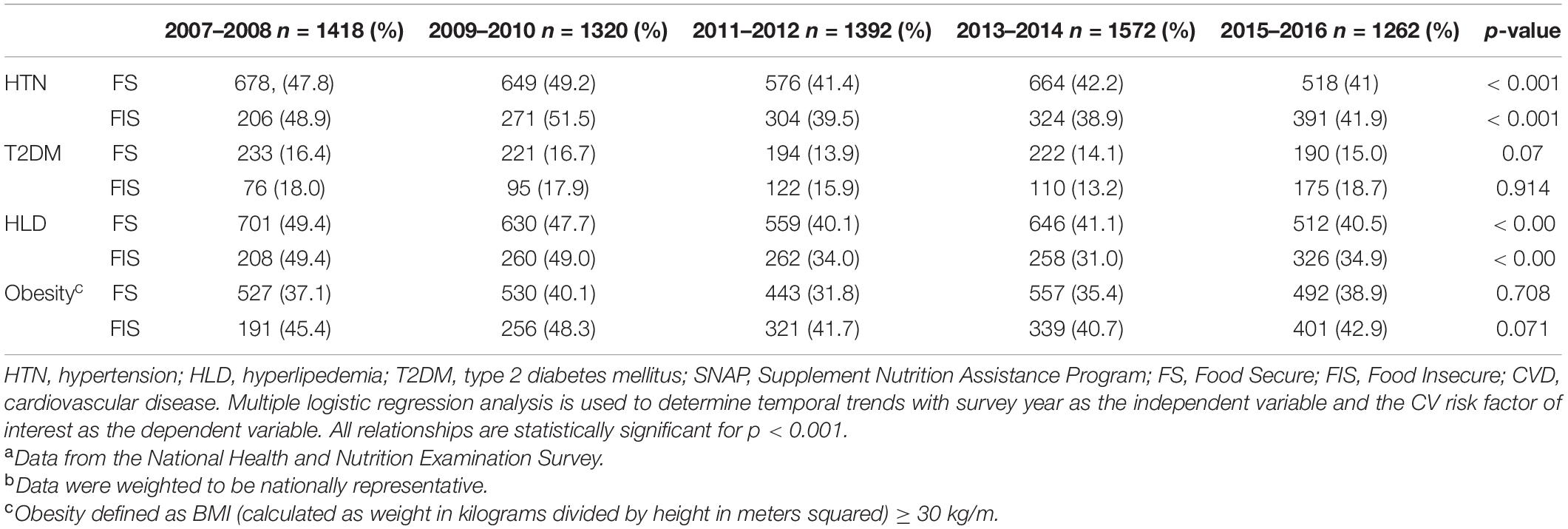
Table 4. Trends in CVD risk factors of adult food insecure participants of the survey, 2007–2016a,b.
When FIS group was further analyzed according to participation in SNAP benefits, FIS SNAP participants demonstrated a significant reduction in the prevalence of HTN (p < 0.001) and HLD (p < 0.001) over the study period (Table 5). No significant change was noted in the prevalence of T2DM or obesity over 10 years (Table 5). Among the non-SNAP participants, HLD decreased significantly (p = 0.007) but HTN did not (Table 5). Remarkably, obesity rates decreased significantly only in the group not receiving SNAP (Table 5).
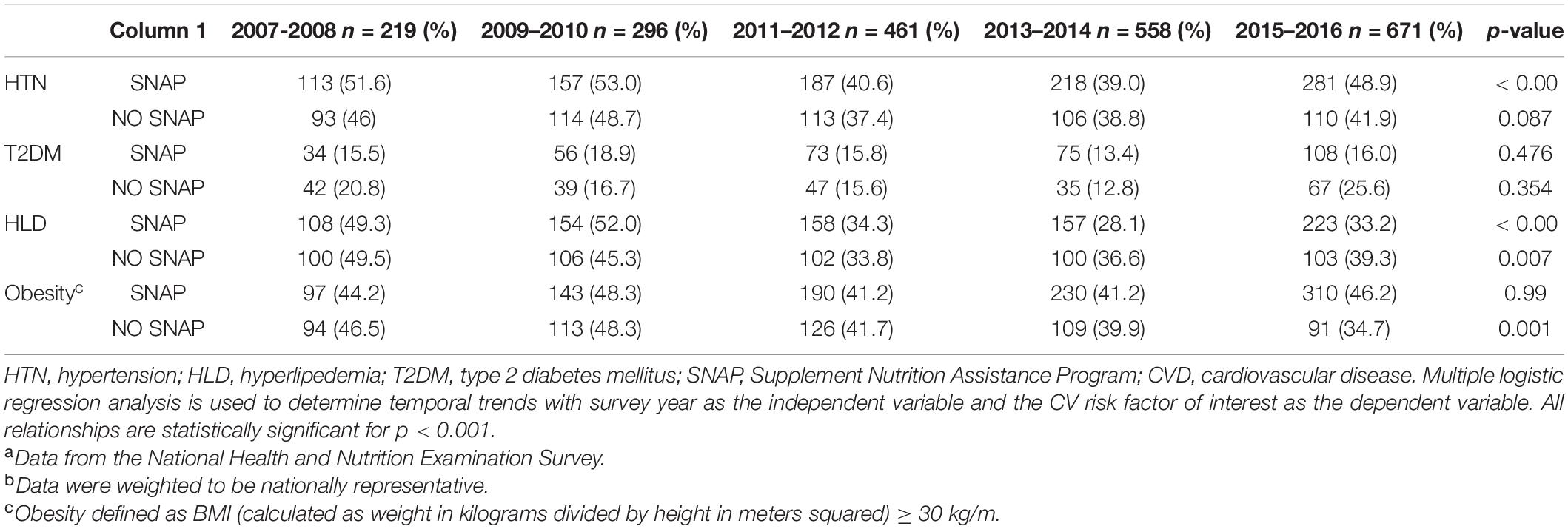
Table 5. Trends in CVD risk factors of adult food insecure participants of the survey, categorized by SNAP participation, 2007–2016 a–b.
Discussion
Our study provides important findings on the prevalence of CVD risk factors among FIS adults in the United States and the association with participation in SNAP.
The principal determinant of obesity and other cardiometabolic diseases is lifestyle, of which food habit is a main component (15). In our study, we found that the prevalence of obesity among FIS adults was higher compared to FS adults. Additionally, FIS SNAP participants did not show an improvement in the prevalence of obesity over 10 years. An interesting cross-sectional analysis by Myers et al. (16) from years 1999 to 2016 shows that prevalence of food insecurity has increased over the study period. Additionally, the study found that obese individuals had higher reports of food insecurity. Our study did not show statistically significant difference in prevalence of T2DM between FS and FIS groups. Similar prior studies (17, 18) however have shown association of food insecurity with poor glycemic and overall metabolic control in adults. Further studies are needed that examine association between food insecurity and CVD risk factors. Specific population subgroup analysis based on ethnicity, sex, and other social variables including economic, education level, geographic location, and marital status, can help identify factors which may reduce prevalence of both food insecurity and obesity in the long term.
Supplemental Nutrition Assistance Program is a federal program which offers financial assistance to eligible people, and is designed to strengthen food and nutritional security. Although previous reports (19) demonstrated that SNAP alleviates food insecurity and improves dietary quality, SNAP participants may in fact have lower quality diet than non-SNAP participants (20). While previous studies have shown that SNAP participation is effective in increasing intake of caloric and nutritious foods, SNAP participants overall do not meet the key recommended nutrition guidelines in daily food habits (20). Greater emphasis is needed to improve the diet quality, and subsequently the CV health of SNAP participants. Further, health care providers should be trained to screen for food security and have knowledge on how to address this topic with their patients.
There was a significant downward trend in the prevalence of HTN and HLD among the FIS SNAP participants over 10 years. Unhealthy diet is one of the top contributors for worsening CVD and associated risk factors (21). SNAP improves access of nutritionally adequate foods, and therefore has the capacity to influence household wellbeing beyond just nutrition and hunger, by directly impacting health outcomes of participants (2, 10). Despite this favorable trend in HTN and HLD in our study, prior studies have shown disparities in the diet quality between SNAP participants and the high income population (22). United States fruit and vegetable consumption in the low-income population remains below recommended levels (23). SNAP-Ed program is a USDA program which promotes healthier eating choices with a limited budget through education and awareness (24). The education programs, national campaigns from groups like American Heart Association (AHA) (25), and increase in public awareness on nutrition have shown an improvement in diet components of SNAP participants, including increase in whole grain, fruits, vegetables and decrease in SSB consumption (26). SNAP benefits are critical for many FIS low income families. Along with improving public education on nutrition, urgent reform and policy changes at state and local level that promote and support a healthier diet are needed. Mozaffarian and colleagues (27) who studied a model evaluating one such possible policy disincentivizing unhealthy food purchases, and incentivizing healthy food purchases including fruits and vegetables, noted a significant decrease in CV deaths and substantial cost benefits. More public health research assisting SNAP and other similar federal programs improving dietary quality of the participants is needed.
Our study has several limitations. First, as with all observational studies, our study cannot prove direct causality. Second, our data also does not allow for long-term assessment in SNAP participation and cardiovascular outcomes. Food security, depending on the adequacy of food, can wax and wane. As such, an individual’s level of food security, and therefore SNAP participation may change over time. The level of food security over time is not measured in our data, which focuses on the previous 12-months. Third, our analysis is based on the self-reported presence or absence of CVD risk factors, rather than actual measurement of these risk factors. Therefore, some misclassification is possible. Fourth, we were unable to exclude participants with established CVD, as the survey does not contain this information. Finally, NHANES only assesses responders’ food insecurity over the last 12 months before survey participation, and thus we were not able to assess long-term food security levels amongst survey participants.
Conclusion
Ready access to guideline-recommended nutrient intake remains a challenge in the United States. Our study shows the favorable trends in the prevalence of HTN and HLD among FIS SNAP participants over a 10 year period. Our study also highlights the persistence of high levels of T2DM and obesity in the adult FIS population. These findings support the need for continuing efforts toward promoting a sustainable, healthy diet among the low-income population and the need to further reduce the health disparities caused by food insecurity.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: NHANES, https://www.cdc.gov/nchs/nhanes/index.htm.
Author Contributions
PS designed and directed this study and wrote the manuscript. HC, JP, and WA provided conceptual and technical guidance. NS and JS provided guidance with statistical analysis for this study. RK, LM, and AS provided support with literature review and editing and background researching the topic of food insecurity. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: final data for 2017. Natl Vital Stat Rep. (2019) 68:1–77.
2. Yu E, Malik VS, Hu FB. Cardiovascular disease prevention by diet modification: JACC Health Promotion Series. J Am Coll Cardiol. (2018) 72:914–26.
3. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. (2019) 74:e177–232.
4. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018. Washington, DC: U.S. Department of Agriculture (2019).
5. Rose D, Oliveira V. Nutrient intakes of individuals from food-insufficient households in the United States. Am J Public Health. (1997) 87:1956–61. doi: 10.2105/ajph.87.12.1956
6. Mello JA, Gans KM, Risica PM, Kirtania U, Strolla LO, Fournier L. How is food insecurity associated with dietary behaviors? An analysis with low-income, ethnically diverse participants in a nutrition intervention study. J Am Diet Assoc. (2010) 110:1906–11. doi: 10.1016/j.jada.2010.09.011
7. Ford ES. Food security and cardiovascular disease risk among adults in the United States: findings from the National Health and Nutrition Examination Survey, 2003-2008. Prev Chronic Dis. (2013) 10:E202. doi: 10.5888/pcd10.130244
8. Morales ME, Berkowitz SA. The relationship between food insecurity, dietary patterns, and obesity. Curr Nutr Rep. (2016) 5:54–60. doi: 10.1007/s13668-016-0153-y
9. Centers for Disease Control and Prevention [CDC]. Defining Adult Overweight & Obesity. Available online at: https://www.cdc.gov/obesity/adult/defining.html#:~:text=Adult%20Body%20Mass%20Index&text=If%20your%20BMI%20is%20less,falls%20within%20the%20obesity%20range (accessed June 7, 2021).
10. Ratcliffe C, McKernan SM, Zhang S. How much does the supplemental nutrition assistance program reduce food insecurity? Am J Agric Econ. (2011) 93:1082–98. doi: 10.1093/ajae/aar026
11. U.S. Department of Agriculture Food and Nutrition Service. Supplement Nutrition Assistance Program (SNAP) Eligibility 2019. (2019). Available online at: https://www.fns.usda.gov/snap/recipient/eligibility (accessed October 1, 2022).
12. Mendy VL, Vargas R, Cannon-Smith G, Payton M, Enkhmaa B, Zhang L. Food insecurity and cardiovascular disease risk factors among mississippi adults. Int J Environ Res Public Health. (2018) 15:2016. doi: 10.3390/ijerph15092016
13. Vercammen KA, Moran AJ, McClain AC, Thorndike AN, Fulay AP, Rimm EB. Food security and 10-Year cardiovascular disease risk among U.S. adults. Am J Prev Med. (2019) 56:689–97. doi: 10.1016/j.amepre.2018.11.016
14. Centers for Disease Control and Prevention [CDC]. About the National Health and Nutrition Examination Survey. (2017). Available online at: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm (accessed October 1, 2022).
15. Sreenivasan J, Khan MS, Sharedalal P, Hooda U, Fudim M, Demmer RT, et al. Obesity and outcomes following cardiogenic shock requiring acute mechanical circulatory support. Circ Heart Fail. (2021) 14:e007937. doi: 10.1161/CIRCHEARTFAILURE.120.007937
16. Myers CA, Mire EF, Katzmarzyk PT. Trends in adiposity and food insecurity among US adults. JAMA Netw Open. (2020) 3:e2012767. doi: 10.1001/jamanetworkopen.2020.12767
17. Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. (2013) 36:3093–9. doi: 10.2337/dc13-0570
18. Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. (2007) 22:1018–23. doi: 10.1007/s11606-007-0192-6
19. Executive Office of the President of the United States. Long-Term Benefits of the Supplemental Nutrition Assistance Program. Washington, DC: Executive Office of the President of the United States (2015).
20. Andreyeva T, Tripp AS, Schwartz MB. Dietary quality of americans by supplemental nutrition assistance program participation status: a systematic review. Am J Prev Med. (2015) 49:594–604. doi: 10.1016/j.amepre.2015.04.035
21. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/S0140-6736(12)61766-8
22. Conrad Z, Rehm CD, Wilde P, Mozaffarian D. Cardiometabolic mortality by supplemental nutrition assistance program participation and eligibility in the United States. Am J Public Health. (2017) 107:466–74. doi: 10.2105/AJPH.2016.303608
23. Olsho LE, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: a randomized controlled trial of the USDA Healthy Incentives Pilot. Am J Clin Nutr. (2016) 104:423–35. doi: 10.3945/ajcn.115.129320
24. Molitor F, Doerr C. SNAP-Ed policy, systems, and environmental interventions and caregivers’ dietary behaviors. J Nutr Educ Behav. (2020) 52:1052–7. doi: 10.1016/j.jneb.2020.05.013
25. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. (2010) 121:586–613. doi: 10.1161/circulationaha.109.192703
26. Korczak R, Marquart L, Slavin JL, Ringling K, Chu Y, O’Shea M, et al. Thinking critically about whole-grain definitions: summary report of an interdisciplinary roundtable discussion at the 2015 Whole Grains Summit. Am J Clin Nutr. (2016) 104:1508–14. doi: 10.3945/ajcn.115.126672
27. Mozaffarian D, Liu J, Sy S, Huang Y, Rehm C, Lee Y, et al. Cost-effectiveness of financial incentives and disincentives for improving food purchases and health through the US Supplemental Nutrition Assistance Program (SNAP): a microsimulation study. PLoS Med. (2018) 15:e1002661. doi: 10.1371/journal.pmed.1002661
Keywords: prevention, food insecuirty, nutrition, cardiovascular health, cardiovascular prevention
Citation: Sharedalal P, Shah N, Sreenivasan J, Michaud L, Sharedalal A, Kaul R, Panza JA, Aronow WS and Cooper HA (2022) Trends in 10-Year Predicted Risk of Cardiovascular Disease Associated With Food Insecurity, 2007–2016. Front. Cardiovasc. Med. 9:851984. doi: 10.3389/fcvm.2022.851984
Received: 10 January 2022; Accepted: 29 April 2022;
Published: 24 May 2022.
Edited by:
Ruan Kruger, North-West University, South AfricaReviewed by:
Mansi Patil, Asha Kiran JHC Hospital, IndiaVasudevan Ramachandran, Bharath Institute of Higher Education and Research, India
Copyright © 2022 Sharedalal, Shah, Sreenivasan, Michaud, Sharedalal, Kaul, Panza, Aronow and Cooper. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Parija Sharedalal, psharedalal@gmail.com
 Parija Sharedalal
Parija Sharedalal Neal Shah2
Neal Shah2  Liana Michaud
Liana Michaud Risheek Kaul
Risheek Kaul